Introduction
Simulation-based training has become a comprehensive practice to improve skill levels in procedures such as intubation1. Control of the airway is the first and most critical treatment. The «A» in the ABC requires that no other action can be taken until the airway is safe, since if the airway is not safe, nothing can help the patient2.
Intubation performed outside the operating room is often performed on an emergency basis, with no time to obtain adequate airway assessment, in patients with poor cardiovascular reserve, often in geographically challenging settings, and by staff with less training than anesthesiologists3.
It is the fundamental responsibility of an anesthesiologist to maintain adequate gas exchange by ensuring the airway, and tracheal intubation is an essential skill in both elective and emergency anesthesia4. Clinicians performing endotracheal intubation must be competent to perform this technical skill safely5.
Medical students present a high level and a broad field of theoretical knowledge, but lack practical experience and, therefore, must be trained in the use of supraglottic airway instruments, particularly in emergency departments and intensive care unit, tracheal intubation should be mastered by students in their last year of career without the recommended experience as a basic skill in the context of their professional training6.
In particular, unsuccessful intubation attempts have been associated with a higher rate of serious complications in emergency patients6,7. These and other factors contribute to intubation outside the operating room that carries an increased risk of adverse events, such as esophageal intubation, hypoxemia, cardiovascular collapse, and cardiac arrest. The risk of one or more adverse events increases when inexperienced or inadequately trained personnel attempt intubation3.
In the education of medical students, the teaching program is designed to train them to perform orotracheal intubation with a manikin. And the orotracheal intubation was a test among the objective simulation constructive examination for the medical license examination in South Korea8. Orotracheal intubation is a basic technique to secure the airway of patients9. In actual practice, it is difficult for many physicians to carry out the procedure in an emergency situation, because they had not received sufficient training10.
A recent study found that anesthesia residents who performed flexible fibroscopic intubation on manikins failed to intubate in 55% of cases11.
Chandra, et al, conducted an investigation to determine the training modality that was the most effective in achieving adequate training in airway management simulation. They found no additional benefit of training in an expensive simulator compared to a simple bench model12.
The hypothesis of the present study was that the use of mobile remote technology in learning intubation laryngoscopy in a training hospital provides a difference in the learning process in orotracheal intubation. The objective was to determine the success of the use of mobile remote technology in learning intubation laryngoscopy during training in the hospital.
Material and methods
Experimental, comparative, non-blind and randomized stu1dy which was made up of a population of 137 participants. Students of the Bachelor of Medicine career at the Universidad Autónoma de Nuevo León School of Medicine who were selected by the Department of Anesthesiology of the University Hospital «Dr. José E. González» of the UANL for the preparation of this research.
137 patients were included in the first instance, this in relation to a previous calculation of the sample size that determined that 70 students would be necessary for each study group (group A and B), later applying the selection criteria they ended up being a total of 117 participants. The inclusion criteria used in this study were: participants who are students of the UANL medical school, older than 18 years, both genders, people who have not had training on orotracheal intubation. The exclusion criteria selected were: students not enrolled in the UANL medical school and those students with previous training in intubation. The only elimination criterion was: participants who during the investigation decide to quit training.
The study was carried out with prior authorization from the Research Ethics Committee and under verbal informed consent, since it corresponds to the observation of the performance of an activity on manikins.
The population described above was randomly assigned to two groups A and B, which were jointly given a theoretical class on intubation technique. In the same way, both groups were given an additional visualization session via remote intubation on manikins, in addition to basic training in orotracheal intubation with a videolaryngoscope and an explanation of the orotracheal intubation technique. Later, laryngoscopies were performed on the manikin, by the participant until the objective was achieved, while the variables to be measured were observed and documented. At the end of the training, a satisfaction survey was applied to all participants. Later, in another time period, they were allowed to make an attempt at intubation with the opposite technique to that used at the beginning, and in this way to determine which technique was most useful to achieve effective training prior to successful intubation on a manikin.
The results were emptied into an Excel table for later analysis by SPSS version 24. Subsequently, an equivalence formula of proportions of two populations was used to assess the equivalence of the videolaryngoscope against the conventional laryngoscopy technique to find the percentage of improvement in the technique. With a confidence of 99% and a power of 90%, with an expected percentage of success of 70 with 30% of amplitude, leaving a range of success between 55% and 85%.
Results
A total of 117 participants were chosen for the preparation of the results of this study in such a way that they were divided into two groups: group A (65 participants) and group B (52 participants). In both group A and group B participants in this study, the female gender predominated, in group A 46 (70.8%) were women and 19 (29.2%) were men, while group B, 32 (61.5%) of the participants were women, while the remaining 20 (38.5%) were men.
In the case of group A, the mean of the academic year was 7.12 ± 1.14 and in the case of group B it was 7.16 ± 1.22, with a p value of 0.98.
The students in group A performed an average of 1.77 ± 0.93 repetitions of conventional laryngoscopy, while with the use of a videolaryngoscope they performed an average of 1.08 ± 0.37 times. The results of group B in terms of number of repetitions of conventional laryngoscopy were 1.16 ± 0.37, as well as with the use of videolaryngoscope they were 1.31 ± 0.58.
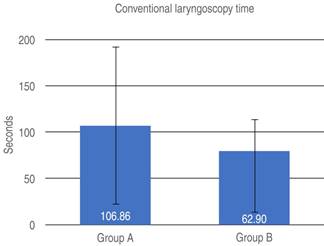
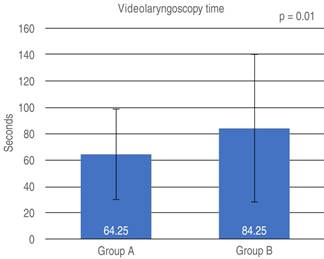
The time in which the members of the study managed to perform the procedures was evaluated. Group A managed to perform conventional laryngoscopy in an average time of 106.86 ± 84.87 seconds (p = 0.002), while group B performed it in 62.90 ± 65.81. In the same way, the videolaryngoscope time was taken, where group A reported an average time of 64.25 ± 34.23, while the time recorded in group B was 84.25 ± 55.67 seconds (p = 0.01) (Figures 1 and 2). The results obtained showed a significant value probably related to the methodology used when preparing the students before performing the practice intubations.
The members of group A responded to the satisfaction survey on the practice of conventional laryngoscopy that was applied to them, where 46 (70.8%) of the participants showed a strong agreement, 18 (27.7%) agreed somewhat, and only 1 (1.5%) person said they did not agree or disagree. While those in group B, 27 (51.9%) of the participants expressed that they strongly agreed with the elaboration of the procedures, 24 (46.2%) said they somewhat agreed, as well as 1 (1.9%) preferred not to give an answer.
In the same way, with videolaryngoscope, a satisfaction survey was also carried out in which the members of group A, 62 (95.4%) of the participants said they strongly agreed with the practice, 1 (1.5%) expressed neither agreement nor disagree, as well as 2 (3.1%) did not give an answer to the question. In group B, 50 (96.2%) said they strongly agreed with the practice, only 1 (1.9%) disagreed and on the other hand 1 (1.9%) student did not give an answer.
During the procedure, the participants reported having undergone some complications when performing conventional laryngoscopy (Table 1). In group A, 18 (27.7%) of the students reported having problems causing a dental injury, 9 (13.8%) presented problems due to intubation of the esophagus, 11 (16.9%) students reported having both difficulties already mentioned, and on the other hand, 27 (41.5%) said they had no complications. In group B, 17 (32.7%) participants said they had difficulties in causing a possible dental injury, 35 (67.3%) of the participants reported no complications.
Table 1: Complications presented during conventional laryngoscopy (group A and B).
| Number of times presented | Percentage of students who presented it | ||||
|---|---|---|---|---|---|
| Complications | Group A | Group B | Group A | Group B | p* |
| Dental injury | 18 | 17 | 27.7 | 32.7 | 0.64 |
| Dental injury + intubation in esophagus | 11 | — | 16.9 | — | 0.001 |
| Intubation in esophagus | 9 | — | 13.8 | — | 0.001 |
| None | 27 | 35 | 41.5 | 67.3 | 0.07 |
* Student t test.
Complications experienced by students at the time of videolaryngoscope were also recorded (Table 2). In group A, 8 (12.3%) of the participants had problems causing a possible dental injury, 1 (1.5%) person had problems due to intubation of the esophagus, and the remaining 56 (86.2%) participants said they had no complications. In group B, the most common complication was dental injury with 12 (23.1%) cases, 1 (1.9%) person expressed having difficulties when introducing the tube, 1 (1.9%) person could cause a dental injury, as well as had difficulty due to intubation of the esophagus, and the remaining 38 (73.1%) students did not present complications (Table 3).
Table 2: Comparison of complications presented during videolaryngoscopy in group A and B.
| Number of times presented | Percentage of students who presented it | ||||
|---|---|---|---|---|---|
| Complications | Group A | Group B | Group A | Group B | p* |
| Dental injury | 8 | 12 | 12.3 | 23.1 | 0.11 |
| Dental injury + intubation in esophagus | — | 1 | — | 1.9 | 0.89 |
| Intubation in esophagus | 1 | — | 1.5 | — | 0.87 |
| Difficulty inserting the tube | — | 1 | — | 1.9 | 0.89 |
| None | 56 | 38 | 86.2 | 73.1 | 0.43 |
* Student t test.
Table 3: Associated p values between groups.
| Variable | Type of variable | p | Interpretation |
|---|---|---|---|
| Age* | Quantitative numerical | 0.65 | NS |
| Gender | Qualitative numerical | 0.37 | NS |
| Academic degree* | Quantitative numerical | 0.98 | NS |
| Number of conventional laryngoscopies* | Quantitative numerical | 0.001 | S |
| Number of videolaryngoscope laryngoscopies* | Quantitative numerical | 0.009 | S |
| Conventional time* | Quantitative numerical | 0.002 | S |
| Videolaryngoscope time* | Quantitative numerical | 0.01 | S |
| Number of complications* | Quantitative numerical | 0.05 | S |
NS = not significant; S = significant.
* The two-tailed Student’s t test is used.
Discussion
Orotracheal intubation must be performed by trained personnel, a situation which is not common to happen at the time of performing this procedure, for that reason the training of doctors and future doctors has been proposed for a long time so that in the future they are trained if at any time they have to perform an intubation. In the study carried out by Lee et al in 2013, they were able to observe that orotracheal intubation training was necessary for medical personnel in the management of the airway2. Chandra et al have conducted an investigation on the training modality that would prove to be the most effective in structuring simulation training of airway management, in their study they did not find any additional benefit of training in an expensive simulator compared to a model simple bench12. In the study that we conducted, inexperienced medical students, after providing them with theoretical and practical knowledge, were able to perform intubations on training manikins.
Despite the fact that orotracheal intubation is considered a basic technique, studies have observed that it was difficult for many doctors to perform this procedure because they had not received sufficient training, which is why it is provided. In a simulation carried out by Starck et al in which inexperienced physicians performed intubations, they reported that videolaryngoscope had a higher success rate compared to direct laryngoscopies with a significantly greater difference10. In the study that we carried out, similar results were reflected, with videolaryngoscope being the ones that were performed successfully in most cases compared to conventional laryngoscopy.
In the study by Chew et al, it was observed that during the use of the canalized King Vision videolaryngoscope and McGrath had a mean intubation time of 41.3 ± 20.3 seconds and 38.5 ± 18.7 seconds respectively(13), while in the study that we did the conventional laryngoscopies were carried out in an average time of 84.8 ± 67.4 seconds between groups A and B, while videolaryngoscope were performed in an average time less than 74.25 ± 44.4 seconds. This difference between the results was found to be significant, which could be associated with the previous preparation that the students participating in the study had.
In the aforementioned study, participants when choosing which videolaryngoscope they would prefer for teaching said they were pleased with both devices used13. In our study at the time of conducting the satisfaction survey, 60% of the participants taking into account both groups A and B said they were satisfied with the use of the conventional laryngoscope, while 96% of the participants in both groups reported To be pleased with the use of the videolaryngoscope, the videolaryngoscope has been a useful tool for teaching residents in training14, this method being the one that globally increases the confidence score compared to conventional laryngoscopy.
Conclusions
The use of mobile remote technology is shown to be effective for the preparation of physicians and future physicians when performing an orotracheal intubation, although it is well known that performing this procedure in a training hospital is not the same as doing it on a real patient when needed due to the environment, time and accuracy that is required to be done during real scenarios.
Videolaryngoscope was more appropriate than conventional laryngoscopy when performed in inexperienced personnel, being performed in less time, showing fewer complications on the part of students during its performance, as well as allowing students to show higher success scores compared to conventional laryngoscopy.











 text new page (beta)
text new page (beta)