The SARS-COV-2 has caused a pandemic with not only sanitary but economic and social repercussions as well. Without having a specific treatment, with a slow vaccination process and with the appearance of more contagious variants, we must continue to implement the preventive measures which should also be emphasized if we want to return to our daily activities. Traditional preventive measures are designed to reduce the transmission of droplets produced by infected individuals when sneezing or coughing. However, a large proportion of the cases appear to airborne transmission of aerosols.
Possible ways of transmission: SARS-COV-2 has a diameter of 0.06 to 0.14 microns1. The viral particles are in most cases, transmitted by respiratory secretions from infected patients in the form of drops which have dimensions within the range of < 0.6 to 1,000 microns2. The virus is carried directly by respiratory secretions to susceptible subjects or indirectly when in contact with contaminated surfaces by those secretions.
There’s an ongoing debate about whether the virus is also transmitted through aerosols and in what portion. To that, the answer seems to be yes, it can also be transmitted by aerosols.
Studies from 1940 and 1950’s classified the respiratory secretions by their size: droplet (those above 5 microns) and in aerosols (below 5 microns)3. These studies suggest that drops gravitate and settle at a maximum distance of approximately 2 meters. It is on the basis of these ancient investigations that public health policies recommend a physical distance of 2 meters.
More recently it has been shown that this binary concept of just drops and aerosols is insufficient in order to understand the turbulent movement of the respiratory secretions. It has been postulated that the direct transmission of the virus occurs through high-impulse cloud that carries the particles over long distances (dynamic model of turbulent clouds)2,4. It has been demonstrated that when a person coughs, sneezes, shouts, talks or even just breathes, the respiratory secretions (loaded with the virus) are casted in all sizes4. Drops bigger than 100 microns fall in under 3 seconds at a distance of 2 meters, while those with dimensions of approximately 1 micron can dehydrate and remain as «droplet nuclei» in the air for up to 12 hours and can also travel longer distances with air currents5. Regarding the transmission of COVID-19, there’s no hard evidence that demonstrates that it only stays within the 2 meter range but there is more evidence aiming towards a transmission through drops and aerosol sprays (as discussed later on). Due to its dimensions, it’s possible that aerosols containing the virus can be transferred to deeper regions of the airways.
Other viruses that have caused important epidemics, like Influenza and SARS, also show evidence of transmission which includes aerosols. In 19796 an influenza outbreak was reported in passengers from a commercial flight. Before taking off, an engine failure was reported. 54 passengers were kept in the cabin (one of whom had influenza symptoms) for at least an hour without air conditioning or an extraction system. Later on, they allowed the passengers to leave the plane while the repair continued but for those who chose to stay, remained inside the plane for up to three hours. Finally, they took off and arrived at their destination. At the 72 hour mark, 72% of the passengers had symptoms and in 20 out of those 22 there was serological evidence of the infection: 86% in those who had stayed more than three hours versus 56% when they had stayed inside less than that period of time. To explain this, authors provide the explanation of the dispersion of aerosols inside the cabin when neither the air conditioning nor the extraction system works. In 20037 a flight with a symptomatic person by SARS and 119 other passengers reported that 20 people developed SARS and 2 probable SARS only 4 days after the flight. Once located and interrogated, they denied being in contact with patients with SARS before or after the flight. The majority of the infected passengers were seated at a distance of 2.3 meters (relative risk 3.1, IC 1.4-6.9 when compared with the rest of the passengers) which according to authors, points to a probable transmission caused by coughing or sneezing droplets. Aircraft ventilation is considered efficient to keep the environment free of pathogens since it exchanges air every 3-4 minutes and goes through a high-efficiency filter system designed to filter particles from 0.3 to 1 micron8. This may have reduced the risk of infection at greater distances within the cabin. Another outbreak that caught attention and also points to dispersion by aerosols was reported in 20049. 187 cases of SARS occurred in an apartment complex in Hong Kong, and more than half of the patients with SARS (99 patients) lived in building E. Residents from the upper and middle levels of building E had a significantly higher risk than the rest of the residents that lived in the inferior part of the building; this finding is consistent with an ascending column of polluted hot air in the air duct generated from a mid-level apartment unit. Once a computational model of the dynamics of the winds was made, it was possible to explain the spread of aerosols and the secondary contagion of other cases in 3 adjacent buildings.
In relationship to COVID-19, there’s also evidence of dispersion and secondary contagion of aerosols contaminated by the virus. Studies have demonstrated viral RNA detected with polymerase chain reaction (PCR). Although this doesn’t demonstrate viable virus in sufficient quantity to produce infections, it does indicate the possibility of viral transmission via droplets and aerosols.
A study made in University of Nebraska10 demonstrated the presence of viral RNA disseminated in the rooms of isolated patients with COVID-19. Samples from the air and multiple surfaces of 11 of those rooms were taken. Samples of air collected more than 6 feet away from the patients were positive for viral RNA, as were samples taken in hallways outside of the rooms. An outbreak of COVID-19 in an apartment building in Hong Kong11 could’ve been secondary to a faulty pipeline where contaminated feces from one case may have allowed the virus to spread by air. Epidemiological analysis and study of air conditioning flows also support an outbreak inside a restaurant in China where there was the spread of several people sitting at different Tables where the current from the air conditioning most likely spread the aerosols of a patient12. In Bergamo, Italy13, viral particles were detected in the air of an industrial zone that was heavily impacted by SARS-CoV-2. There was an outbreak in a building in Seoul14 where 1145 people worked and lived in, and whom were tested, 97 were positive and of these, 94 were in a call-center on the 11th floor, out of a total of 216 employees located on that floor (43.5%) and of those, the majority were seated working on the same side, which makes suspicion about the dispersion of aerosols through air conditioning. Other outbreak reports in choirs15 and churches16 where in addition to the congregation of several people in a closed environment, singing can facilitate the dispersion of aerosols, as it has been shown that raising the volume of the voice generates more drops and aerosols than with lower volumes17. In all these outbreaks, although contagion through drops or fomites is not completely ruled out, it’s strongly suspected that the transmission mechanism was through aerosols.
Another phenomenon that has contributed to the rapid spread of the virus is the phenomenon of super-spreading. This occurs when the index case is capable of infecting a large number of susceptible subjects. Several reports in Asian cities18 and in Israel19 have shown how 10% of primary cases are capable of triggering up to 80% of the cases reported in those cities. In South Korea, a religious leader appears to be the causative of 63.5% of all the cases reported in Seoul20. In Jordan21 at a wedding with 360 attendants, the index case infected 85 people. This phenomenon although complex and not well studied, seems to depend on: the degree of infectivity of the carrier, the exposure time of the susceptible subjects and the setting where the exposure takes place. It’s estimated that the viral dissemination by index cases is greater in the pre-symptomatic period and during the onset of symptoms22 and as a result, up to 44% of secondary cases are infected during the pre-symptomatic stage of the index cases.
As we’ve seen there is evidence that the SARS-COV-2 virus can be transmitted not only by drops and microdroplets that directly contaminate susceptible subjects or objects that function as fomites, but also through aerosols which is not a minor risk factor as we have seen in the description of various outbreaks that predominate in closed places and with crowds. As long as there is no effective treatment, any preventive measure that helps reduce transmission and is not harmful should be welcomed, as is the case with face masks.
Benefits of the use of face masks (FM) in the general population
FM have been an important part of surgical asepsis for several years and in times of pandemics its use outside the operating room has played a relevant role in trying to stop the spread of infections. We are currently facing a new pandemic, COVID-19, which still has no specific treatment. Deaths continue to increase on a day to day basis and health services are under pressure from saturation. Recent evidence about airway transmission has led public health policies to recommend the universal use of FM, basing this decision also on the «precautionary principle» where there is little to lose and much to gain. In 200523 the World Commission on the Ethics of Scientific Knowledge and Technology states that «When human activities may lead to morally unacceptable harm that is scientifically plausible but uncertain, actions shall be taken to avoid or diminish that harm. Morally unacceptable harm refers to harm to humans or the environment that is threatening to human life or health». This is the «precautionary principle».
Initial statements from health organizations such as the World Health Organization were inconclusive, recommending the use of FM only for those with suggestive symptoms of COVID-19 in order to reserve them for health workers24 despite the fact that in another statement from 2019 they had recommended the use of FM for the general public in the situation of a severe pandemic since its partial protective effect could have an important impact on the decrease of transmission25.
Face mask’s history
There is evidence that shows FM being used by doctors all the way back to the Middle Ages, they were known as the «sharp doctors» because of the shape of the masks they used. It is likely that they contained aromatic herbs such as cinnamon or cloves and carried them in order to avoid being infected with the «miasma» (putrefactive emanations) that was believed to transmit the plague26.
In 1867 Lister postulated that surgical wound infections were caused by microorganisms that Louis Pasteur had recently described. In the 1880s surgeons suspected that these germs contaminated wounds through hands, instruments being used or even through exhalation and to top it off it was the cause of the «hospital gangrene» that very frequently complicated surgeries, especially abdominal ones and those involving the bones. In those same years Carl Flügge demonstrated that the respiratory drops had bacteria and in 1897, the surgeon Johann Mikulicz proposed the use of a FM that he described as «a piece of gauze tied to the cap with two cords that covered the nose, mouth and beard»27.
FM were initially single layered and shortly after double layer in an attempt to prevent the spread of droplets in a more effective way. At the beginning of the 20th century it wasn’t implemented very often and in 1914 the surgeon Fritz Konig considered that its use (along with the use of gloves) was unnecessary and also caused irritation of the hands and face26. Weaver28 reported a decrease in the spread of diphtheria from 23 to 8%, and scarlet fever from 8% to 0 in the periods 1914-1916 and 1916-1917 among nurses at the Durand Hospital in Chicago once the use of chiffon FM was implemented. Haller29 and Weaver30 described the first studies on the filtration capacity of FM made of chiffon by testing several layers (from 1 to 8) and with a variable number of threads per inch. Patients infected with pneumococcus29 or streptococcus30 coughed with or without FM which varied in design (depending on the layers and the number of threads) into Petri dishes at a distance of 1229 or 630 feet. They concluded that the FM that offer better filtration should be made up of 3 layers with a number of threads per inch of 32 × 2629 or 3 layers, 44 × 4030. With more layers there was greater difficulty in breathing. In 1921 Kirschner26 in a chapter dedicated to «measures to combat infections in surgeries» states that it is necessary to carry the FM. To avoid contamination, their use became popular and by 1937 almost all the photographs of surgeons show them with FM31.
During the 1910 plague of Manchuria and the Influenza pandemic between 1918-1919 FM were introduced for the first time outside of the operating room aiming to protect health workers and the general population. In fact, the decrease in mortality rates in some cities such as San Francisco was partly attributed to its use. Most of them were made of washable material, so they were reused for a long time. With time, they were replaced by others made of synthetic materials and by the 1960s almost all were disposable since synthetic fibers deteriorated with sterilization. The industry in charge of designing disposable FM conducted studies about their efficiency, but the reusable ones were not studied enough so over time the idea that they were unsafe to use spread27.
Mask’s efficiency
The efficiency of FM depends on a combination of multiple factors: the material they are designed with and its capacity to block out the entrance and exit of particles, the amount of leak that is around and the good use of the person wearing it.
The use of a physical barrier like a FM can be an effective way of avoiding the spread of respiratory droplets. A 5 step mechanism must occur in order for filtration to control aerosols32: sedimentation, inertial impact, interception, diffusion and electrostatic attraction. For aerosols from 1 to 10 microns the first two filtration mechanisms are the predominant ones. Both the diffusion caused by Brownian movement and the mechanical interception of the particles are the predominant mechanisms for particles that measure between 100 nanometers and 1 micron. For particles in the range of nanometers (which can easily escape the fiber tissues) predominates the electrostatic attraction.
Even with the best material, if the FM does not adhere to the face, the virus-containing particles can penetrate through the gaps. Leaks can also occur if the clamping mechanism is weak.
The way in which the FM is carried is also important. If not positioned correctly, even a N95 FM that sticks to the face, will not achieve all the benefits it can offer.
Home-made masks (HMM): these masks are in no way recommended for health workers that come in contact with COVID-19 patients. As has been shown with influenza, its use by health workers leads to a higher frequency of infections than the use of medical masks33. Carrying a HMM can help prevent the spread of infectious agents and in a pandemic situation where the general population does not have access to N95 or medical mask, the use of these FM may be one more alternative to other public health measures aimed stop infections.
There are several studies on its efficiency where various materials have been tested. In 200834 HMM from tea cloth, medical mask and N95 were compared and the protection offered for the carrier was found to be 50 times higher for N95 vs HMM, and 25 times higher for medical mask vs HMM. That efficiency descended quickly after 3 hours of use for both the N95 and medical mask. The degree of protection for the dissemination abroad of all of them was lower compared to the protection to the carrier. They conclude that even so, HMM can help along with other measures to decrease the number of reproduction and to control epidemics.
Rengasamy35 conducted laboratory tests with different materials: one-layer HMM with t-shirts, towels, scarfs and cotton. The particles went from 0.2 to 1 micron and they compared the efficiency with the N95. For the N95 the penetration was below 5%, meanwhile the other materials had a penetration between 40-90%, therefore the protection it offers is pretty low for the particles within those disseminations.
Davies36 tested the HMM made up of cotton t-shirts in 21 healthy subjects. The subjects would cough with the masks placed in a box from which cultivation samples were taken and compared against subjects with medical mask or without FM. There were so few colonies obtained in the subjects without FM that it was not possible to observe differences between the groups.
Bae37 evaluated the effectiveness of medical mask (made of three-layer polypropylene) and of cotton (100% cotton of 2 layers) to filter SARS. CoV-2. Four symptomatic patients were asked to cough without FM, with medical mask and with cotton HMM. A Petri dish with viral transport medium was placed 20 cm away. The viral count with or without FM showed practically no differences. However, the authors retracted38 since the detected PCR values were very close to the detection limit, so these values are not reliable and their results were not interpretable.
Ma39 analyzed the effect hand washing and FM on the avian Influenza virus. The quantification of the virus was by means of the PCR reaction technique. In addition to being more than 98% effective in eliminating the virus with handwashing with soap and a 0.25% chlorine solution, N95, medical mask and HMM with four layers of kitchen paper were able to block the virus within the aerosol in a 99.98, 97.14 and 95.15% respectively.
Konda and collaborators32 studied the functioning of various fabrics (natural and synthetic) (cotton, silk, chiffon, flannel, various synthetic fabrics and their combinations) and the effect of multiple layers combined to evaluate the benefits of the different filtration mechanism over particles within the 10 nm to 6 micron range, and they compared them with the N95 and the medical mask. When single layers were used, the filtration efficiency ranged from 5 to 80% for particles smaller than 300 nm and from 5 to 95% for those larger than 300 nm. The filtration efficiency improved when more layers were implemented and when combinations were used: with combinations (like cotton-silk, cotton-polyester, cotton-flannel) it was greater than 80% for particles smaller than 300 nm and greater than 90% for those greater than 300 nm. The authors mention that the greater effectiveness with the combinations may be the result of the mixed effect of mechanical and electrostatic filtration. This efficiency in the studied materials was almost similar to that observed with the N95. But to achieve this, there should be no leaks. When leaks exist (like it occurs with the medical mask and HMM) the efficiency dropped to 60%.
Mueller40 analyzed the leakage percentage of HMM with different designs and compared them with medical masks and N95. The HMM were able to remove between 38 and 96% of the particles studied with a range of 0.02 to > 1 micron. By adding a layer of nylon tights, it was possible to noticeably reduce leaks around the FM and significantly improve filtration efficiency. In 5 of the 10 materials tested, the efficiency was higher than that observed with 3M medical masks.
In hamsters infected with SARS-CoV-2, FM reduces not only the frequency of infection but also the manifestations. Chan41 placed infected hamsters and healthy hamsters in two separate boxes, the boxes had porous walls and the air flow was unidirectional towards healthy hamsters. 66.75% of the healthy hamsters were infected. Subsequently, a layer of FM fabric was placed on the walls, with which the contagion rate decreased to 16.7% and, furthermore, the manifestations of infection and histopathological changes after being sacrificed were less compared to infected hamsters without the FM layer, which means that the infectious dose could also decrease.
Impact of universal use of home-made mask
Mathematical models have been done in an attempt to predict the effect of non-pharmacological measures to try to mitigate the pandemic42. The effective use of medical mask (with an estimated efficiency over 70%) could have eliminated the pandemic if only 70% of the New York residents would have used them. With the use of HMM (with an estimated efficiency below 30%, although as we have already seen, this efficacy may be greater with multi-layer HMM and fabric blending32,40), a significant decrease in the number of cases could also have been achieved, without getting rid of the pandemic. But if other non-pharmaceutical preventive variables were included (hand washing, social distance, etc.) in the mathematical model associated with the use HMM with a calculated efficiency of 30%, the pandemic could also have been eliminated.
Eikenberry43 simulated another model with the data on the dynamics of contagions from New York and Washington: with the use of HMM with an efficiency of 50% used by 80% of the population, deaths could have been reduced by a range between 17 and 45% in a period of 2 months, and even with a HMM with efficiency of only 20%, mortality could decrease by 2 to 9%.
Worby and Chang44 investigated the role of face mask use and distribution among the general public using mathematical modeling, in order to better understand the reduction in infections and deaths and how to optimize distribution in a resource-limited setting. They consistently observed that the random distribution of masks throughout the general population is a suboptimal strategy. In contrast, prioritizing the elderly population, and retaining a supply of masks for identified infectious cases generally leads to a larger reduction in total infections and deaths.
In China45 during the SARS epidemic a case-control study was carried out that compared the exposure of 94 cases that had not come in contact with patients, with 281 cases infected with close contacts. It was found that in these 94 patients the risk factors were: having visited clinics with possible patients with SARS, eating out and frequently traveling by taxi. By multivariable analysis, persons who always wore masks had a 70% lower risk of being diagnosed with clinical SARS compared with those who never wore masks, and persons with intermittent mask use had a 60% lower risk.
In regards to COVID-19, an epidemiological analysis of confirmed cases was carried out in Hong Kong46, specifically in infected persons who used or did not use FM. In addition, the incidence per million inhabitants in Hong Kong and other countries was compared with population densities, public health systems, and measures of social distance similar but that do not routinely use FM in the general population. The incidence in Hong Kong (129 cases per million inhabitants) was significantly lower (p < 0.001) than in Spain (2,983), Italy (2,250), Germany (1,241), France (1,151), the United States (1,102), United Kingdom (831), Singapore (259) and South Korea (200). Compliance in the use of FM in the general public was 96.6% (range 95.7-97.2%). They observed 11 outbreaks in recreational places where the use of face mask was not forced against only 3 outbreaks in work places where its use was forced (p = 0.036). The widespread use in Hong Kong after the first case of COVID-19 was reported is probably due to the poor experience of the SARS epidemic in the population.
Zhang et al47 demonstrated that measures such as social distancing were insufficient in Italy and New York to stop transmission, and until the use of FM was implemented, it was possible to reduce dissemination.
In the German province of Jena48, ever since the use of FM became mandatory, the number of new infections decreased by 1.32% per day (almost 25% in 20 days). When analyzing the changes by age groups, the most benefited were those over 60 years of age, where in 20 days the transmission was reduced by just over 50%, while in those under 60 the reduction in that period of time was 10 to 20%.
In Washington D.C.49 ever since the use of FM became mandatory, a daily decrease of 0.9, 1.1, 1.4, 1.7 and 2% was observed between days 1-5, 6-10, 11-15, 16-20 and 21 or more. It is estimated that thanks to this mandatory order, there were about 200 thousand fewer cases between March 31 and May 22, 2020.
In a multivariate analysis on the possible predictors of mortality of 196 countries Leffler50 found that the duration of infection in a country, and a high proportion of the population over 60 years of age were associated with higher mortality rate per capita, while the use of FM by the population was negatively associated with mortality (all with p < 0.001).
In China51 the majority of the contacted cases are reported to be intrafamily. In a retrospective study Wang 52 demonstrated in the multivariate analysis that the factors that favorable influenced the reduction of intrafamily transmission were: the use of FM of every member within the household before (OR = 0.22) or after the appearance of symptoms (OR = 0.20) and the frequent use of alcohol or chlorine-based disinfectants (OR = 0.18).
In a meta-analysis of 172 observational studies and 44 comparative studies Chu53 identified that a distance greater than 1 meter, eye protection and the use of FM (OR 0.15) (N95, medical mask or reusable multi-layer cotton) can help achieve a reduction in the risk of infection.
We know that the economic impact will appear almost in parallel with the health impact. The Goldman Sachs group has made an estimate of the benefit that the widespread use of FM in the US can have54. During the January-April quarter, social distancing measures and the closure of economic activities (the sum of both variables measured by an effective closure index or ECI for its initials in English) caused a drop in gross domestic product of 17%. They calculate that if they managed to make the use of FM mandatory throughout the United States (and not only in some states, while in others it is only «recommended» to use it) the infection rate would decrease to 0.6-0.7% for every seven days, instead of the existent increase of 2.9% every seven days based on the data from the days of the publication. In order to achieve these results and be able to observe a decrease in the number of infections without forcing the use of the FM, one would have to increase the ECI to a level that would cause an additional drop in gross domestic product of 5%.
The change in the paradigm from not recommending the use of FM to promoting its use in a generalized way has been based on the knowledge of the spread of SARS-CoV-2 in the pre-symptomatic phase and in asymptomatic patients with high viral loads. The use of FM serves as a means of control to prevent the dispersion of droplets and aerosols, and to reduce the risk of contamination from the exterior. There are those who mention that its use can give a feeling of false security, while others say its use should be reserved for health workers only. Some more say that there is a lack of randomized, double-blind studies55 that have demonstrated the efficacy of FM in the community. The absence of evidence must be distinguished from the evidence of absence. Indirect information in the presence of a pandemic such as the current one should be sufficient argument to promote its use. The fear of its improper use must be replaced by intense educational campaigns on its correct use56 (Figures 1 and 2) and the fear of shortages must lead to the massive manufacture of FM that would also generate sources of employment. The «precautionary principle» must be followed if we are to prevent the population from paying the high price of the pandemic with their health and their lives, and all the other collateral damage such as economic impact, suicides due to isolation and helplessness generated by loss of jobs.
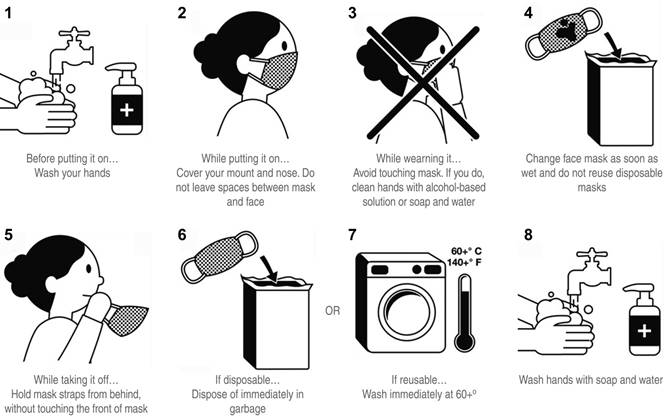
Tomado de https://www.teamosv.com/guidance/.
Figure 1: Using face masks. How to use, remove and dispose a face mask safely.











 nueva página del texto (beta)
nueva página del texto (beta)



