INTRODUCTION
Human gait is a complex process that involves many systems such as bones, joints, muscles, peripheral nerves, spinal cord, and the brain. When one, or some, of these systems fail or present some limitations, the gait process is altered and becomes a pathological gait [1] [2] [3] [4]. Therefore, the analysis of the human gait represents an important instrument for the early and timely identification of pathologies, and a component of follow-up rehabilitation programs [5] [6] [7] [8] [9]. In addition, gait analysis is also important to the design of equipment, devices, rehabilitation systems, prostheses, orthoses, and humanoid robots [10] [11] [12] [13] [14]. Moreover, it can be used in sports science to improve the techniques and performance of athletes. However, such a diagnostic tool requires the use of biomechanical parameters to characterize and evaluate the human gait performance.
Several research works have undertaken the assessment of human gait as a prevention, monitoring, and diagnostic tool. For example, it can be possible to avoid foot ulcers in diabetic patients by increasing foot motion during the intermedia stance phase of the gait cycle [15]. Patients with knee osteoarthritis (KOA) often adopt a type of antalgic gait as their disease progresses [16]. These patients generally try to protect the damaged knee by biomechanical adaptations that may affect the movement of the joints of the lower extremities and the lower back [17] [18]. Gait and balance abnormalities have been described even at early stages in the diagnosis of Alzheimer's ailment [19]. Similarly, a fall during gait can be the result of specific characteristics of gait disturbances related to neurological disorders [20]. Additionally, it has been observed that robotic gait rehabilitation can improve the biomechanical parameters in chronic hemiplegic patients [21].
Numerous biomechanical parameters have been used in the analysis of the human gait. It was reported that gait patterns and parameters values often vary with the gait velocity [22], a parameter used to identify groups of elderly patients who are at increased risk of death and serious morbidity after cardiac surgery [23]. The spatiotemporal parameters have been related to the gait mechanics of the KOA progression [24] [25] [26]. Cadence, stride length, and gait velocity are the main gait parameters that provide a general idea of how well patients can walk [27]. In addition, the joint angles of the knee flexion and leg shortening effect parameters are very relevant when analyzing the kinematics of the knee and designing knee prostheses [28].
Over time, the interest in analyzing the performance and characteristics of human gait through biomechanical parameters has increased because human gait alterations can be associated with pathologies known to cause bad body postures and muscle imbalance [19] [29] [30] [31] [32]. However, in the clinical area the gait analysis still relies on the knowledge and experience of the specialist, which represents a certain degree of subjectivity. In addition, few studies have correlated the gait parameters and metrics with clinical problems such as musculoskeletal, neurological, and circulatory problems [33]. Furthermore, there is not a comprehensive baseline study to ease the understanding and selection of biomechanical parameters for normal and pathological gait analyses. Therefore, the objective of this research work is to identify and analyze the main biomechanical parameters commonly used in the assessment of human gait.
MATERIALS AND METHODS
Literature search
A literature review was carried out to identify research papers dealing with biomechanical parameters used in the human gait analysis. Original articles published in scientific journals indexed in PubMed, Web of Science, Scopus, Science Direct, and Google Scholar, were considered. Although no date of publication limits were used, papers published during the last ten years were mainly considered to identify the latest advances. The keywords and mesh terms related to human gait (gait and walking), type of gait (normal, healthy, pathological, hemiplegic, parkinsonian, paraparetic, dancer, apraxic, ataxic, vestibular, equinus, steppe, multisensory deficits, diabetic, prudent, senile, antalgic, dysmetric, Trendelenburg, and claudic), and biomechanical parameters, (temporal, spatial, spatiotemporal, angular, force, strength, kinematic, and kinetic), were used in the search.
In the first search, 380 publications were selected. Next, the title, abstract, and conclusions of each paper were reviewed and the following selection criteria applied: 1) the study should be based on a quantitative analysis of pathological or healthy gait, 2) the study should report the analysis of pathological gaits caused by neurological, musculoskeletal and circulatory problems, 3) the study should use kinematic and kinetic parameters, and other particular parameters according to the case study or pathology, 4) the study should indicate application areas, and 5) priority was given to papers that included the use of three-dimensional digital measurements in gait analysis. The first three criteria were mandatory and the last two were desired. Two independent researchers (authors) conducted searches by applying the criteria and resolving discrepancies. A total of 144 papers were finally selected.
Analysis of the parameters
In order to identify the most important biomechanical parameters reported in the literature, the selected papers were analyzed in detail. Then a classification of the gait parameters was established according to the following application areas: clinical, sports, and research. Furthermore, the parameters used in the analysis of pathological gaits were identified and classified according to the cause of the pathology as: circulatory, musculoskeletal, and neurological. Finally, set theory was used to systematically analyze the biomechanical parameters, and to facilitate their selection according to the application area. The complete flow chart of the methodology used in this study is shown in Figure 1.
RESULTS AND DISCUSSION
Demographic and anthropometric data
The demographic and anthropometric information of the patient is essential when conducting a gait analysis. Table 1 summarizes the demographic and anthropometric parameters reported in the literature.
Table 1 Anthropometric and demographic data required for human gait analysis.
| Data | Description | |
|---|---|---|
| Anthropometric | Ankle width | The anthropometric length between the lateral and medial malleolus of each leg. |
| ASIS width | The horizontal distance between the anteroposterior iliac spines. | |
| Body mass index | A key index for relating weight to height. | |
| Bodyweight | The force that induces the gravity on the human body. | |
| Foot length | The anthropometric length between the heel and the big toe. | |
| Foot width | The anthropometric length between the first and fifth metatarsal heads. | |
| Knee width | The anthropometric length between the lateral and medial epicondyles of the femur. | |
| Lower leg length | The anthropometric length between the lateral femoral condyle and the lateral malleolus. | |
| Pelvic height | The anthropometric length between the superior iliac crest and the ischium when seated on a stiff chair. | |
| Pelvic width | The anthropometric length between the right and left superior iliac crests. | |
| Standing height | The height of a person from foot to head. | |
| Thigh-length | The anthropometric length between the greater trochanter and the lateral femoral condyle. | |
| Demographic | Age | The time that a person has lived (in years). |
| Duration of the disease | The elapsed time of having a disease condition (in years). | |
| Gender | Male/Female. | |
| Marital status | The status of a person according to the civil registration. | |
| Employment | The activity where a person is hired to perform a series of specific tasks. | |
| Place of birth | City, state, and country where she/he was born. | |
| Residence | Place where she/he lives. |
The demographic data comprises general information about the group of people such as age, gender, place of residence, as well as social or economic characteristics such as occupation, marital status, etc. The most common demographic data used for gait analysis are age and gender.
Table 1 also describes the anthropometric data used in gait analyses. Since computer vision systems, tracking systems, or force plates are commonly used in gait studies, it is important in the collection of anthropometric data to have a robust benchmark that can be used to calibrate the vision system, define the dimensions of the walkway, locate the force plates, etc. [34] [35] [36]. A tendency to decrease the amount of anthropometric information required in gait analyses was also observed [37] [38] [39].
Gait analysis applications
In general, six main application areas were identified and the percentage of each calculated, Table 2[40] [41] [42] [43] [44] [45] [46] [47] [48] [49] (based on the number of uses in each application area relative to the total number of uses). The six application areas were then rearranged into three generic types: clinical (56%), research (31%), and sports (13%) applications; similarly, as reported by Muro-de-la-Herran [33].
Table 2 Main applications of gait analysis and proposed classification.
| Applications of gait analysis | Use (%) | Proposed classification | Use (%) |
|---|---|---|---|
| Diagnosis | 25 | Clinical | 56 |
| Rehabilitation | 31 | ||
| Art and entertainment | 9 | Research | 31 |
| Ergonomics and industrial applications | 13 | ||
| Fundamental and applied research | 9 | ||
| Sports | 13 | Sports | 13 |
Gait parameters
In the literature, human gait biomechanical parameters have been classified in several ways. However, all the classifications converge on the use of spatial, temporal, angular, and strength biomechanical parameters. Table 3 presents the biomechanical parameters most used in the literature for gait analysis. In this table, each parameter has been classified, defined, and identified according to the application area.
Table 3 Description of the biomechanical gait parameters and their applications.
| Application | ||||||||
|---|---|---|---|---|---|---|---|---|
| Type of parameter | Reference | Biomechanical gait parameters | Acronym | Unit | Definition | Clinic | Research | Sports |
| Spatial | 33 | Accumulated altitude | ACA | m | The vertical distance traveled. | X | ||
| 53-56 | Height of step | HS | m | The movement of the lower extremities gives a height to the step, avoiding the drag of the feet. | X | |||
| 28 | Shortening effect of the leg | SEL | % | The natural shortening effect of the lower limb in the swing phase, generated by the knee joint to avoid tripping. | X | |||
| 30, 34, 53-65 | Step length | SL | m | The distance between the placements of a foot. | X | X | X | |
| 30, 57-60 | Step width | SW | m | The distance between two equivalent points of two consecutive footprints. | X | X | X | |
| 30, 34, 53-65 | Stride length | STL | m | The distance between the placements of the same foot. A stride is equivalent to a complete gait cycle. | X | X | X | |
| 53-56 | Traveled distance | TD | m | The length of the journey traveled. | X | X | ||
| Temporal | 30, 34, 53-65 | Cadence | CAD | steps/min | The number of steps taken in a time interval. | X | X | X |
| 53-56 | Gait autonomy | GA | min | The maximum time that a person can walk, considering the number and duration of stops. | X | |||
| 30, 34, 53-65 | Gait phases | GP | % | Set of divisions of the gait cycle. | X | X | X | |
| 30, 34, 53-65 | Gait velocity | GV | m/s | The distance traveled in a defined time interval. | X | X | X | |
| 30, 34, 53-65 | Stance time | STT | s | The time elapsed from the moment that the heel touches the ground until the toes are lifted, for each foot. | X | |||
| 30, 34, 53-60, 64-66 | Step time | ST | s | The time elapsed between the placement of one foot and the placement of the other. | X | |||
| 53-56 | Stop duration | SD | s | The time in which both feet are on the ground, without being part of a gait phase. | X | |||
| 34, 53-56, 64-66 | Stride velocity | STV | m/s | The distance traveled in one stride in a defined time interval. | X | X | X | |
| 30, 34, 53-65 | Swing time | SWT | s | The time elapsed from when the foot is lifted off the ground until it touches it again, for each foot. | X | |||
| Angular | 30, 53-60 | Body posture (inclination, symmetry) | BP | o | The direction of a corporal segment with respect to geometric references (usually the conventional references). | X | X | X |
| 30, 34, 53-60, 64-66 | Body segment orientation | BSO | o | Geometric description of the behavior of the body referenced to geometric entities. | X | X | ||
| 30, 34, 53-60, 64-66 | Joint angles | JAN | o | The angle between two members due to the biomechanical movements of the joints (hip, knee, ankle). | X | X | ||
| 30, 53-60 | Step angle | SA | o | Direction of the foot during the step. | X | X | X | |
| Force | 30, 34, 53-60, 64-66 | Ground reaction forces | GRF | N | The forces generated on the floor due to weight and walking. | X | X | |
| 30, 53-63 | Momentum | MO | N·m | Measurement of the rotating potential that a joint performs against a force to a specific line. | X | X | ||
| 30, 34, 53-60, 64-66 | Muscle activation index | EMG | mV | Electrical activity produced by muscles. | X | X | ||
| 30, 53-60 | Muscle force | MF | N | The forces generated in the limbs due to the action of the contractions and tractions of the muscles. | X | X | ||
| Others | 53-56 | Existence of tremors | ET | Yes/ No | Presence of disturbances in the form of oscillation patterns. | X | ||
| 53-56 | Falls | FA | Yes/ No | Any event that precipitates the individual to the ground against his will. | X | |||
| 53-56 | Long-term monitoring of gait | LTMG | h, d | The monitoring history of the gait behavior in an established period. | X | X | ||
| 53-56 | Route | RUT | - | Specification of the path walked on the walkway. This path can be straight or curve. | X | X | ||
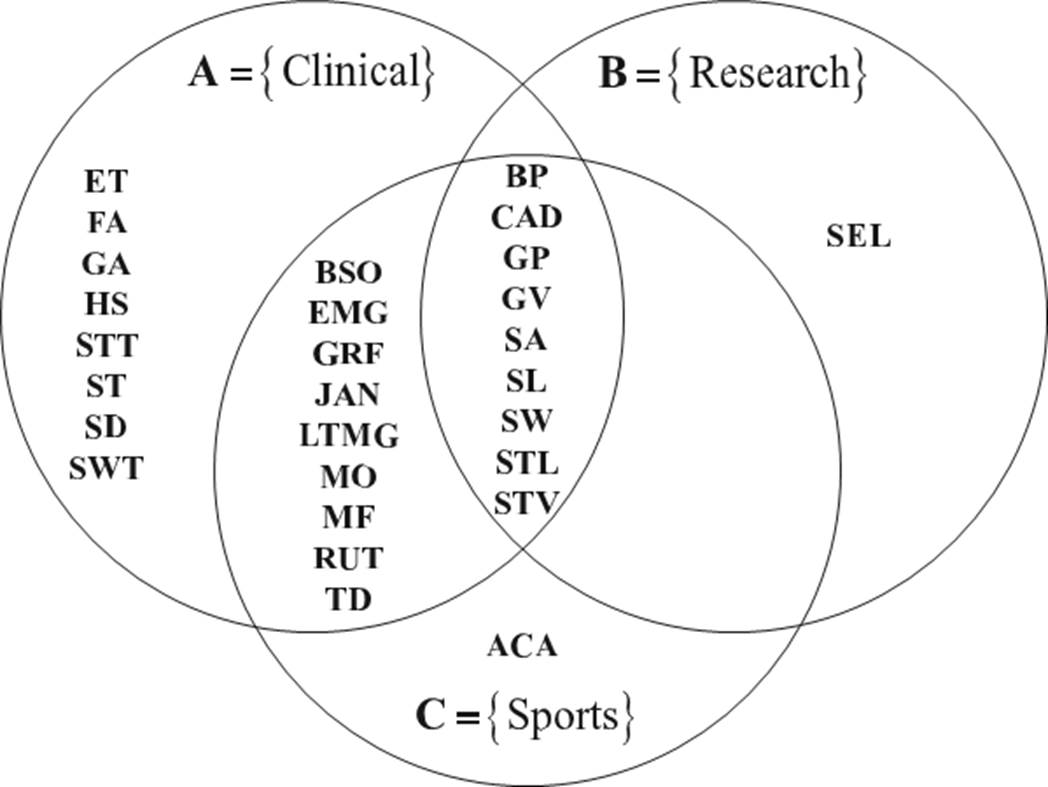
In order to systematically analyze the biomechanical parameters, set theory is used. Three sets A, B and C are defined and correspond to the parameters used in clinical, research, and sports applications, respectively. The common parameters among the three sets are given by the intersection of the three sets, as shown in Figure 2.
Figure 2 shows that the spatiotemporal parameters predominate in the three application areas. Notice that between the research and the sports sets, and between the research and the clinical sets, there are no common parameters besides those parameters described by the intersection A∩B∩C. This suggests that clinical applications make use of most of the biomechanical parameters used in gait analysis.
Clinical gait parameters
The disability due to gait problems represents approximately 55% of the total disabilities worldwide [50]. These gait disorders may be a consequence of various pathologies, which are known to disturb human motor functions. The most common semiology of the pathological processes that affect human gait is pain, limitation of movement, muscular weakness, and deficit of neurological control [29] [51]. Consequently, the study of the characteristics of human gait by means of biomechanical parameters represents a potential tool for the diagnosis, treatment and monitoring of some pathologies. In the literature, many gait pathologies have been analyzed and classified according to the root cause of the functional impairment [27] [29] [33] [51]. Based on a preliminary study [52], three large groups of pathologic causes are proposed: neurological, musculoskeletal, and circulatory.
Table 4 synthesizes the clinical gait parameters according to the type of pathology, and presents the parameters used in healthy gait analysis, extending the work presented by Muro-de-la-Herran [33]. On the other hand, Table 5 presents the biomechanical parameters and the demographic and anthropometric data used in pathological gait analyses.
Table 4 Synthesis of the gait parameters according to the type of pathology.
| Pathological gait according to the origin of the problem | Healthy gait [34,64-66,144-147] | |||||
|---|---|---|---|---|---|---|
| Type of parameter | Gait parameter | Acronym | Neurological [19,20,53-56,67-128] | Musculoskeletal [30,57-60,129-142] | Circulatory [61-63,143] | |
| Spatial | Step height | HS | X | |||
| Step length | SL | X | X | X | X | |
| Step width | SW | X | X | X | ||
| Stride length | STL | X | X | X | X | |
| Traveled distance | TD | X | ||||
| Temporal | Cadence | CAD | X | X | X | X |
| Gait autonomy | GA | X | ||||
| Gait phases | GP | X | X | X | X | |
| Gait velocity | GV | X | X | X | X | |
| Stance time | STT | X | X | X | X | |
| Step time | ST | X | X | X | ||
| Stop duration | SD | X | ||||
| Stride velocity | STV | X | X | |||
| Swing time | SWT | X | X | X | X | |
| Angular | Body posture | BP | X | X | ||
| Body segment orientation | BSO | X | X | X | ||
| Joint angles | JAN | X | X | X | ||
| Step angle | SA | X | X | |||
| Force | Ground reaction forces | GRF | X | X | X | |
| Momentum | MO | X | X | X | ||
| Muscle activation index | EMG | X | X | X | ||
| Muscle force | MF | X | X | |||
| Others | Existence of tremors | ET | X | |||
| Falls | FA | X | ||||
| Long-term monitoring of gait | LTMG | X | ||||
| Route | RUT | X | ||||
Table 5 Gait parameters and data for pathological and healthy gaits.
| Pathological Gait (Origen of the problem) | Healthy Gait [34,64-66,144-147] | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neurological | Musculoskeletal | Circulatory | ||||||||||||||||
| Type of parameters | Biomechanical gait parameters | Hemiplegic [53-56,67,68] | Parkinsonian[19,69-73] | Paraparetic (in scissors) [74-78] | Dancer (typical of Korea) [79-86] | Apraxic [20,87-89] | Ataxic (taloneant) [90-93] | Ataxic (cerebellar) [94-99] | Vestibular (star or compass) [100-106] | Equinus (steppe) [107-112] | Abnormalities associated with multisensory deficits [113-118] | Prudent [119-122] | Senile [123-128] | Antalgic [30,57-60,129-132] | Dysmetric[133-137] | Trendelenburg[138-142] | Claudic [61-63,143] | |
| Spatial | Step height | X | X | |||||||||||||||
| Step length | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Step width | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| Stride length | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Traveled distance | X | |||||||||||||||||
| Temporal | Cadence | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| Gait autonomy | X | X | ||||||||||||||||
| Gait phases | X | X | X | X | X | X | X | X | X | X | X | |||||||
| Gait velocity | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |
| Stance time | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Step time | X | X | X | X | X | |||||||||||||
| Stop duration | X | X | ||||||||||||||||
| Stride velocity | X | X | X | X | ||||||||||||||
| Swing time | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| Angular | Body posture | X | X | X | X | X | X | X | ||||||||||
| Body segment orientation | X | X | X | X | X | X | X | X | X | X | X | |||||||
| Joint angles | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| Step angle | X | X | X | X | ||||||||||||||
| Force | Ground reaction force | X | X | X | X | X | X | |||||||||||
| Momentum | X | X | X | X | X | |||||||||||||
| Muscle activation index | X | X | X | X | ||||||||||||||
| Muscle force | X | X | X | X | ||||||||||||||
| Others | Existence of tremors | X | X | |||||||||||||||
| Falls | X | X | X | X | X | |||||||||||||
| Long-term monitoring of gait | X | |||||||||||||||||
| Route | X | |||||||||||||||||
| Demographic and anthropometric data of patients | Age (years) | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Body mass (Kg) | X | X | X | |||||||||||||||
| Body mass index (Kg/m2) | X | X | X | X | X | X | X | X | X | X | ||||||||
| Duration of the disease (years) | X | X | X | X | X | X | X | X | X | X | X | X | ||||||
| Place of birth | X | |||||||||||||||||
| Gender (F/M) | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Height (m) | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| Weight (Kgf) | X | X | X | X | X | X | X | X | X | X | X | X | ||||||
ANALYSIS AND DISCUSSION
Pathological and healthy gaits
Figure 3 shows the biomechanical parameters used in the assessment and analysis of pathological and healthy (normal) gaits, referred to as set P and H, respectively. It is observed that in the study of pathological gaits most of the gait parameters reported in the literature are used. The spatiotemporal parameters predominate in the study of both pathological and healthy gaits.
As shown in Table 5, most of the spatiotemporal and angular parameters are used in the analysis of pathological gaits caused by neurological disorders. For instance, senile gait studies all the spatiotemporal and angular parameters except the distance traveled, step angle, and body posture are used. The literature also su- ggests that the step height parameter is mainly used in the study of prudent and senile pathological gaits, the traveled distance is used in the analysis of dancer gait, and the stop duration temporal parameter is used in the study of Parkinsonian and senile gaits. Likewise, in the study of Parkinsonian and ataxic cerebellar pathological gaits, all angular parameters are used; in contrast, in the analysis of prudent pathological gaits these angular parameters are not used. The joint angles and body segment orientation parameters are commonly used in the analysis of hemiplegic, Parkinsonian, paraparetic, dancer, cerebellar ataxic, equinus, and senile gaits.
On the other hand, the analysis of pathologic gaits caused by musculoskeletal disorders makes use of many spatiotemporal parameters, and all angular parameters. In the antalgic gait analysis, the ground reaction force and the mo- mentum parameters are used, whilst in the study of dysmetric and Trendelenburg gaits the muscle force parameter is used. Regarding other parameters, the gait phases parameter is used in the analysis of musculoskeletal pathologies.
The main circulatory pathological gait reported in the literature is the claudic gait, which requires several spatiotemporal parameters, and the momentum and gait phases parameters. The gait phases parameter is important in order to identify the most critical phase or phases of this pathological gait.
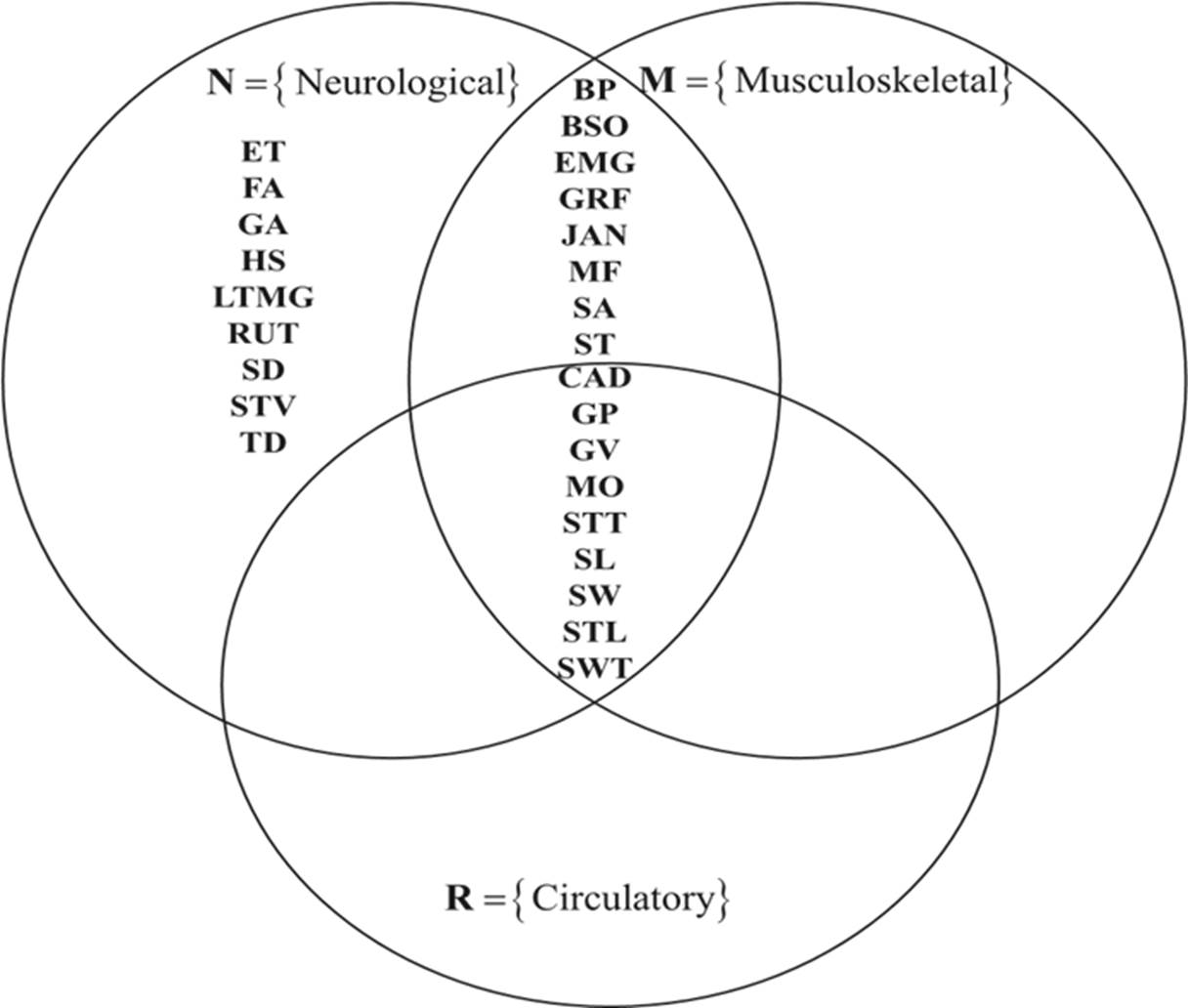
Figure 4 shows the gait parameters used to analyze Musculoskeletal, Neurological, and Circulatory pathologies, referred to as sets M, N, and R, respectively. In this figure, the common parameters used for these pathologies correspond to the intersection of the three sets. On the other hand, the common parameters between the musculoskeletal and neurological pathologies, besides those given by the intersection: M∩N∩R, are: muscle activation index, step angle, step time, body posture, muscle strength, joint angles, body segment orientation, and ground reaction forces. It is observed that the analysis of neurological pathologies demands the use of all the parameters, whereas the analysis of circulatory pathologies makes use of the common parameters of the three clinical applications.
Spatial parameters
Figure 5(a) shows the spatial parameters used in the analysis of pathological and healthy gaits. It is observed that the common parameters used for both pathological and healthy gaits are the step length and stride length. On the other hand, the most common spatial parameters used in pathological gait studies are the step length, step width, and stride length. The traveled distance and height of step are mainly used in the study of pathological gait because of neurological disorders.
Temporal parameters
Figure 5(b) shows that the gait velocity, cadence, gait phases, swing time, and stance time parameters are the most used temporal parameters, and they correspond to the intersection of the four sets H∩M∩N∩R. The step time is the most common parameter in the study of healthy gaits, and musculoskeletal, and neurological gaits. The stride velocity parameter is used in neurological and healthy gait analyses. The gait autonomy and stop duration parameters are only used in the analysis of pathological gait caused by neurological disorders.
Angular parameters
Figure 5(c) shows the common angular parameters used in the analysis of healthy, musculoskeletal, and neurological gaits. The literature also suggests that the analysis of pathological gaits due to circulatory problems does not use angular parameters [31] [32] [33]. The angular parameters BP and SA are mainly used in the assessment of pathological gaits caused by musculoskeletal and neurological problems.
Force parameters
Figure 5(d) shows that the EMG and GRF are frequent force parameters used in the analysis of musculoskeletal, neurological, and healthy gaits. The MF parameter is mainly used in the analysis of musculoskeletal and neurological pathologies, whilst the MO parameter has only been used in pathological gait studies.
Ranking of parameters
In order to rank the biomechanical parameters used in the analysis of pathological and healthy gaits, two criteria were defined: 1) the relevance of the parameter in the research studies, and 2) the frequency, which was calculated using the following expression:
where f is the frequency percentage, n is the number of times the parameter was used in the selected papers. A normalization process was then considered, given a value of 1 to the most used parameter. Regarding the relevance criterion, a value of 1 was given to those parameters with the largest reliability, the most common in different gait analysis (set theory), and the most cited. A relevance value of 0 was assigned to the rest of the parameters. Table 6 shows the results, where it is observed that gait velocity is the most frequently used parameter in the study of human gait because it assesses the functional mobility of an individual and affects his/her gait pattern. Moreover, most of the biomechanical parameters decrease at slower gait velocities and increase at faster gait velocities.
Table 6 General ranking of gait parameters based on their relevance and frequency of use in the literature.
| Gait parameters | Relevance value | % frequency of use | Frequency value | Relevance and frequency value |
Ranking |
|---|---|---|---|---|---|
| Gait velocity | 1 | 8.76 | 1.00 | 2.00 | 1 |
| Cadence | 1 | 7.73 | 0.88 | 1.88 | 2 |
| Stance time | 1 | 7.73 | 0.88 | 1.88 | |
| Step length | 1 | 7.73 | 0.88 | 1.88 | |
| Stride length | 1 | 7.73 | 0.88 | 1.88 | |
| Step width | 1 | 7.22 | 0.82 | 1.82 | 3 |
| Joint angles | 1 | 6.70 | 0.76 | 1.76 | 4 |
| Swing time | 1 | 6.70 | 0.76 | 1.76 | |
| Gait phases | 1 | 5.67 | 0.65 | 1.65 | 5 |
| Ground reaction forces | 1 | 3.09 | 0.35 | 1.35 | 6 |
| Muscle activation index | 1 | 2.06 | 0.24 | 1.24 | 7 |
| Body segment orientation | 0 | 5.67 | 0.65 | 0.65 | 8 |
| Body posture | 0 | 3.61 | 0.41 | 0.41 | 9 |
| Falls | 0 | 2.58 | 0.29 | 0.29 | 10 |
| Momentum | 0 | 2.58 | 0.29 | 0.29 | |
| Step time | 0 | 2.58 | 0.29 | 0.29 | |
| Muscle force | 0 | 2.06 | 0.24 | 0.24 | 11 |
| Step angle | 0 | 2.06 | 0.24 | 0.24 | |
| Stride velocity | 0 | 2.06 | 0.24 | 0.24 | |
| Existence of tremors | 0 | 1.03 | 0.12 | 0.12 | 12 |
| Gait autonomy | 0 | 1.03 | 0.12 | 0.12 | |
| Step height | 0 | 1.03 | 0.12 | 0.12 | |
| Stop duration | 0 | 1.03 | 0.12 | 0.12 | |
| Long-term monitoring of gait | 0 | 0.52 | 0.06 | 0.06 | 13 |
| Route | 0 | 0.52 | 0.06 | 0.06 | |
| Traveled distance | 0 | 0.52 | 0.06 | 0.06 |
The next most used parameters are cadence, stance time, step length, and stride length. It is also observed that the spatiotemporal and angular biomechanical parameters are the most used in the study of both pathological and healthy gaits. The least popular biomechanical parameters reported in the literature are traveled distance, long-term monitoring of gait, and route, which are specific for the evaluation of dancer, ataxia (taloneant), and vestibular pathologies, respectively. Notice that although these parameters are not very popular parameters, they may be as important as the spatiotemporal parameters for some particular pathologies. The results also revealed that the temporal parameters are the most popular with 37% of use, followed by the spatial parameters with 24%, the angular parameters with 18%, the force parameters with 8%, and others with 13%.
According to Whittle MW [27], the cadence, gait velocity, and stride length parameters provide a general idea of how well a patient walks. However, the results of this research work suggest that the stance time is also important. For instance, in the study of musculoskeletal-related gait pathologies [57] [60] [140] [142], the stance time is an indicator of the improvement or deterioration of the pathology. On the other hand, although the stride length of both limbs may be the same, the step length of each limb may be different, as reported by Kirtley C [148]; for this reason, many studies have considered it relevant. The step width is another relevant parameter, [67] [68] [143] [148], which tends to increase with a balance disorder.
General discussion
The proposed analysis and classification of the gait parameters represent a general and practical guide to select the parameters for healthy or pathological gait studies. In general, the spatiotemporal and angular parameters are the most used because they allow a detailed and objective study of the human gait. However, other parameters are specific and important for particular pathologies, such as the cartilage thickness [149], which is used in the study of antalgic gait due to knee or hip osteoarthritis. In this work, only the most general pathologies and parameters reported in the literature have been considered.
It was also observed that most of the pathological gait studies (90%) reported in the literature were conducted on a walkway instead of an electric treadmill. This is because in the analysis of pathological gaits, the gait velocity is a parameter that depends on the pathology, and the evolution and progress of the patient. In contrast, in the studies related to healthy gait, the gait velocity is usually an independent variable that is defined and varied using an electric treadmill.
The stance time parameter is indicative of the improvement, or severity of pain, in the antalgic gait caused by knee osteoarthritis [131]. For example, an increment of the stance time is an indication that the pain experienced by the patient is less and therefore the support of the loading has improved. The use of the step height parameter has not been reported in the literature; however, it can be used in the study of musculoskeletal pathological gaits since it is closely linked to the angular parameter of the knee articulation. The step height parameter may vary due to musculoskeletal pathologies or due to the use of certain footwear, such as the use of high heels, as reported by Arellano [28].
The leg shortening effect parameter is also an important parameter that has been mentioned qualitatively in some works, but a complete quantitative study has not been reported yet. This leg shortening effect may be relevant when designing knee prostheses.
Finally, it can be said that most of the research works related to pathological gait have been conducted considering only intrinsic conditions such as age, gender, weight, etc., or the type of pathology. Few studies have considered both intrinsic and extrinsic conditions such as climbing slopes, walking with a front-load, using a certain type of footwear, walking whilst texting or calling by cell phone, etc.
CONCLUSIONS
A review and analysis of the main biomechanical gait parameters used in the literature to study pathological and healthy gaits has been presented. The gait parameters have been identified and classified according to the type of physical quantity (spatial, temporal, angular, force and others) and according to the application area (clinical, sports and research). The clinical applications were subdivided according to the pathological disorder into neurological, musculoskeletal, and circulatory applications, being the neurological area the one that uses most of the gait parameters. The overall most common parameters are body posture, cadence, gait phases, gait velocity, step angle, step length, step width, stride length, and stride velocity. Finally, it can be said that the results presented in this investigation can be used as a practical guide to identify and select the main biomechanical parameters commonly used in the analysis and monitoring of human gaits under pathological or normal conditions.











 nueva página del texto (beta)
nueva página del texto (beta)