Introduction
Infective endocarditis is a relatively rare but life-threatening disease. In a systematic review of the global burden of infective endocarditis, the gross incidence ranged from 1.5 to 11.6 cases per 100,000 person-years, with high-quality data available only in ten countries, mostly by high-income countries. When untreated, the mortality is high. Even with the best available therapy, contemporary mortality rates are approximately 25%.1 This condition is usually a complication of Staphylococcus aureus bacteremia, which is divided into 4 clinically different groups: users of injecting drug users, hospitalized patients with nosocomial infections, recipients of prosthetic valves and non-injecting drug users.2 Compared with endocarditis caused by streptococci, enterococci or other pathogens, Staphylococcus aureus endocarditis is associated with higher rates of central nervous system complications. In most series, bacterial meningitis is an early feature of the complex manifestation of endocarditis. Note that more than one-third of patients with meningitis develop additional neurological complications such as ischemic stroke, intracranial hemorrhage or cerebral abscess.3 Patients with Staphylococcus aureus endocarditis experience unspecific and fuzzy symptoms; therefore, the duration of that microorganisms present in the bloodstream may be of importance, so it is recommended that patients with meningitis due to Staphylococcus aureus should be examined for endocarditis as other manifestations outside the central nervous system. The risk of embolic events in this pathology is directly proportional to the infective load of the microorganism (e.g. Staphylococcus), the size and mobility of the vegetation, the elapsed time since the infection and the involved valve. Mitral location implies a greater risk than the aortic one.4 This involvement is explained by its pathophysiologic mechanism since the dissemination of emboli infected in brain or meningeal vessels can lead to meningitis or brain abscess, intracerebral hemorrhage and cerebral ischemic event. The atypical presentation highlights the difficulties both in early diagnosis and in the treatment of these patients.5
Case report
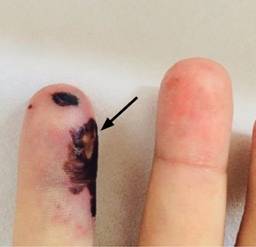
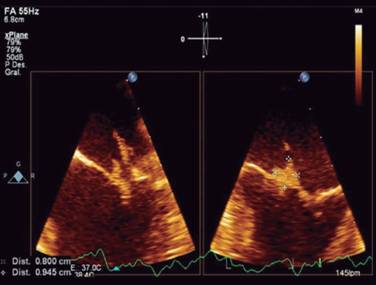
A 37-year-old man, previously healthy, with no history of contagious infectious disease and cardiovascular disease. He is from the State of Mexico, with history of intravenous opioids use (tramadol) 7 times per week, for chronic lower back pain secondary to lumbar herniated disc of one year of progress. The clinical condition started while he was driving, with sudden alteration of alertness manifested by disorientation, drowsiness and aphasia, their relatives observed it so that he was transferred to a private hospital. Upon admission, he remained disoriented. The physical examination is notable for a IV/VI holosystolic murmur over the apex radiating to the axilla. There were painful, nodular, erythematous, skin lesions localized in the pads of the fingers, as well as small, painless, flat spots, red to bluish red on the palms and soles [Osler’s nodes (Figure 1) and Janeway’s lesions (Figure 2)]. The rest of the physical and neurological examination did not present abnormalities. He was admitted to the Medical Center «20 de Noviembre» with fever of 38 oC, breathing rate of 24 rpm, heart rate of 115 bpm, blood pressure 100/60 mmHg. Fluid therapy and empirical antibiotic therapy were started (vancomycin and ceftriaxone). Initial laboratory test results with complete blood count indicating leukocytes of 23,000 mm3, platelets of 108,000 mm3, blood creatinine of 1.3 mg/dL, the rest remained unchanged. Blood cultures were negative. Cranial tomography (cranial CT) without evidence of areas of ischemia or hemorrhage. We proceeded to do a lumbar puncture and the cerebrospinal fluid (CSF) analysis showed cloudy fluid, glucose of 32 mg/dL, proteins of 165 mg/dL, leukocytes of 1760 and lymphocyte of 0. The CSF culture result was isolation of Staphylococcus aureus at 72 hours. The report of the transthoracic echocardiogram was: a structurally normal mitral valve, maximum gradient of 6 mmHg, medium gradient of 3 mmHg, with maximum velocity of 1.2 m/s, with a jet of severe regurgitation, reaching the left atrium roof. Maximum velocity of the jet of 4.4 m/s, with a suggestive image of a vegetation on the anterior leaflet. The transesophageal echocardiogram showed no thickened valves, with a vegetation of 1 × 0.9 cm-sized vegetation on the anterior leaflet, in segments 1 and 2, which oscillated during the cardiac cycle, with a filiform appendix adhered to the distal end of the vegetation (Figure 3), that affected the severe regurgitation jet which was visualized along the lateral wall of the atrium. Vital signs remained stable within the course; however, 72 hours after, he presented decreased alertness of less than 8 points of the Glasgow scale, with respiratory failure requiring advanced airway management and mechanical ventilation, entering the intensive care unit. Due to persistent hemodynamic instability and high-risk of embolism 5 days after entering, he required surgical intervention with valve replacement. He did not present post-surgical complications. Due to clinical state improvement, he was extubated 72 hours after surgical intervention, with no neurological sequela and without cardiac failure, data that might be frequent complications of this disease. Clinically this case meets the modified Duke criteria for clinically infective endocarditis due to the presence of vascular lesions and embolic phenomena, cultures with the presence of Staphylococcus aureus isolated from cerebrospinal fluid and the presence of a vegetation on the echocardiogram.
Discussion
It is important to take into account the neurological complications in a patient presenting infective endocarditis, by performing a thorough initial comprehensive examination. In different studies, the neurological complication is generally indicated; however, it must include a wide range of complications ranging from unspecified manifestations, such as not focal encephalopathy, convulsions or headache, to stroke or severe cerebral hemorrhage. This comprehensive approach could lead to confusion when screening for the true effect of the cerebral involvement on the result of endocarditis or the relationships between brain injury and certain characteristics (size of vegetation and valve involvement).6 In this particular case, the neurological involvement was identified early, and cardiac involvement was suspected due to the presence of a typical clinical condition. In intravenous drug users, more than 30% of infections of the central nervous system are due to Staphylococcus species. In these patients, endocarditis comprises 8% of all acute infections, precedes meningitis and mostly affects the right cardiac structures, mainly affecting the tricuspid valve. It is believed that the great structural damage to the right heart valves is secondary to injected particles with great bacterial load, as well as subtle abnormalities of the immune function of the patient may also have a role in the pathogenesis.7 In contrast, the endocarditis due to Staphylococcus aureus that affects the left heart valves is often associated with high morbidity and mortality, while the right-sided endocarditis is less severe and is most associated with the use of intravenous drug use.8 It is important to emphasize that the detection of clinically silent ischemic or hemorrhagic brain injury can affect performance or the time of surgery, the choice of prosthetic valves and antimicrobial or anticoagulant therapy planning. They should be referred to centers experienced in debridement of infected tissues and infectious diseases for the antibiotics choice.9 Endocarditis in patients with meningitis is associated with a high rate of neurological and systemic complications; it requires a prolonged treatment with antibiotics and cardiac surgery in selected patients. Quick diagnosis and the initiation of antibiotics are of great importance to prevent a primary or recurrent neurological complication. Early surgery in high-risk patients is the second cornerstone of cerebral embolism prevention.10 There are multiple therapeutic challenges of infective endocarditis and include aspects of antibiotic therapy and indications and surgical techniques for its definitive cure. From the point of view of antibiotic treatment, the absence of randomized studies hinders the recommendation of guidelines. This fact is particularly relevant in the case of infective endocarditis due to S. aureus. Despite the fact that it is currently the organism that commonly causes endocarditis, it is not set out which is the better (more effective and less toxic) antibiotic treatment and hospital mortality remains high. Currently, the therapeutic guidelines provide multiple options for Staphylococcal endocarditis, all of them with low scientific level evidence. In this sense, some authors have advocated to change the point of view, to leave a position of consensus that can be difficult to reach, instead of that to describe the different antibiotic guidelines used in reference centers, showing that mortality does not depend on following these guidelines, which is probably more related to the existence of multidisciplinary equipment for the management of this complex entity.11 In this case, the patient was treated with antibiotic therapy based on third-generation cephalosporin plus a glycopeptide completing 4 weeks of treatment, fighting the specific bacterial agent. The surgical treatment was performed within the first week of his hospitalization due to the risk presented. It is a case with a different clinical condition and great complexity in terms of manifestations and complications that can arise, in addition that there are currently multiple descriptions and treatment guidelines. However, they do not show impact on mortality, thus risk factors and clinical conditions must be suspected, and early approach must be initiated and therapeutic interventions must be provided along with multiple management in order to improve the patient prognosis.
Conclusion
Infective endocarditis is characterized by multiple neurological complications. In this particular case, bacterial meningitis is yet an atypical manifestation that must be significantly suspected in patients with risk factors, like in this case the intravenous opioids users. Although the overall incidence of this pathology has remained stable, the incidence of infective endocarditis caused by Staphylococcus aureus has increased. It is the most common causal organism in most areas of the industrialized world, it is partly due to the increased importance of contact of the patient with health care as a principal risk associated with infection (e.g., intravascular catheters, surgical wounds, permanent prosthetic devices, hemodialysis).10 It is essential to make an early diagnosis, as well as to receive comprehensive treatment working together cardiologists, neurologists, infectious disease specialists and thoracic surgeons, since nowadays the complications such as bacterial resistance, decision of surgical treatment and embolic events, lead to increased risk of complications and increased mortality.











 nueva página del texto (beta)
nueva página del texto (beta)