Introduction
Currently anomalies of the origin of the coronary arteries have become important due to the clinical outcome that has been presented, especially in adults, as acute coronary ischemic syndrome, heart failure, syncope, dyspnea and angina. The current incidence of anomalous origin of coronary arteries is from 0.1% to 8.4%. It has been described that anomalous origin of coronary arteries in young people and athletes can lead to sudden death. There are coronary anomalies that imply a different type of risk ranging from low to high risk, with the highest risk being intra-arterial paths with anomalous origin. The main challenge is the timely diagnosis in those patients without coronary risk factors and without valve disease. One of the main initial diagnostic tools is transthoracic echocardiography in the parasternal short axis view at the level of the great vessels. In patients with a poor echocardiographic window, other diagnostic tools are transesophageal echocardiography, computed tomography and magnetic resonance imaging.
Case report
A 50-year-old male with positive smoking during 30 years with a smoking rate of 22.5 packs/year, with a history of hypothyroidism (15 years), mixed dyslipidemia and systemic hypertension. He began his current condition 48 hours before hospital admission with oppressive chest pain 7/10 in intensity, of approximately 30 minutes without irradiation. One day after hospital admission he presented during sleep, oppressive chest pain 7/10 in intensity, accompanied with diaphoresis and nausea lasting more than 30 minutes. So he arrived to the emergency medical service, where a 12- lead electrocardiogram with leads V7-V9 was performed. The ECG showed sinus rhythm, with QRS axis at 45o, heart rate 72 bpm, p wave 40 msec, PR segment 120 msec, QT 388 msec, QTc 421 msec, Q wave in DII and aVF and a 2 mm of ST segment elevation in V7-V9. The patient underwent percutaneous transluminal coronary angioplasty (PTCA) facilitated with Gp IIbIIIa inhibitor (tirofiban). PTCA found absence of the trunk of the left coronary artery, anterior descending artery with independent origin of the left coronary sinus and a short lesion of 20% in the middle segment with TIMI 3 flow (Figure 1); anomalous origin of the circumflex artery from the right aortic sinus, inferior to the ostium of the right coronary artery. It was visualized with 100% occlusion and probable thrombus at the end of the proximal segment, which recanalized due to contralateral collateral circulation Rentrop I (Figure 2). The right coronary artery was dominant and tortuous with a 40% short lesion in the middle segment TIMI 3 flow (Figure 3). Left ventriculography demonstrated mild diaphragmatic hypokinesia, LVEF 55%, D2VI 15 mmHg, and anomalous origin of the circumflex. Circumflex lesions were treated with 3 ORSIRO stents 3 × 15 mm, 3 × 15 mm and 3 × 13 mm with good result flow TIMI 3 (Figures 4 to 6). Optical coherence tomography (OCT) evidenced an adequate attachment of the struts of the stents. The patient had a satisfactory evolution in the Coronary Care Unit.2

Figure 1: Angiography of left anterior descending artery where absence of circumflex artery is observed.
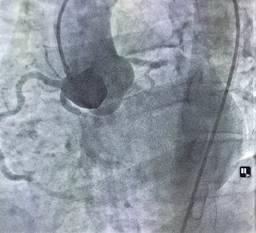
Figure 2: Angiography of the aortic root that documents independent origin of the circumflex artery from the right coronary sinus with proximal segment occlusion.

Figure 3: Angiography showing dominant right coronary artery with 40% lesion in mid-segment, TIMI 3 flow.
Discussion and review of the topic
Congenital anomalies of the coronary arteries can be defined in three large groups, such as alterations in the origin and course of the coronary arteries, alterations of the anatomy of the arteries and alterations in the termination of the arteries.1,3 The classification of this type of anomalies in terms of its severity has not yet been clarified since there are authors that divide them into important, serious, hemodynamically significant and minor and in recent reviews in quantitative and qualitative terms to determine the severity of them.3
Some of the classifications that have been proposed are:3
Abnormalities of origin and path.
Intrinsic anomalies of the coronary anatomy.
Abnormalities of coronary termination.
Abnormal connection of the coronary arteries.
The incidence of sudden death associated with congenital anomalies of the coronary arteries is 0.6% (1 of 162 cases), this is the importance of the timely detection of this type of alterations.4
The anomalous coronary development can arise from the interruption of a chain of molecular and cellular mechanisms. The molecular signals are provided by or directed to specific cell populations.5
The Wilms tumor suppressor gene (Wt1), the zinc transcription factor, is involved in the regulation of retinoic signaling secreted by the epicardium.5 The Wt1-dependent alteration of the retinoic acid synthesis in the epicardium directly or indirectly regulates the expression of PDGF (platelet-derived growth factor) A, B receptors in epicardial-derived cells (EPDC), which interferes with the differentiation of smooth muscle progenitor cells. The cell-to-cell Notch/Delta signaling pathway, which is necessary to promote the fate of the arterial endothelium during the development of coronary blood vessels. Downregulation of the nuclear transcription factor Coup-tfII, a Notch repressor, positive regulation of Ephrinb2 expression in CA progenitor cells (coronary arteries) also correlates with CA endothelial specification, although the underlying genetic mechanism that controls this process is unknown. Finally, fibroblast growth factors (FGFs) and vascular endothelial growth factor (VEGF) secreted by myocardium participate in the regulation of the fate of coronary endothelial cells and vascular assembly.
The anomalous origin of the coronary arteries is usually asymptomatic, although the spectrum of symptoms and associated syndromes is wide, the anomalies of the coronary artery that give symptoms are limited to those that cause a significant alteration in the myocardial perfusion. Coronary anomalies most likely to cause myocardial infarction, ischemia, or ventricular tachycardia are an anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA), large coronary arteriovenous fistulas, and anomalies associated with courses between the great vessels. The other anomalies of the coronary artery are rarely associated with symptoms or sudden death.1,4
Diagnostic tests should be stratified initially based on the age of patients under 35 years. The objective is to prevent sudden death in a primary way, for which the suggested diagnostic tools are ergometry, echocardiography and nuclear stress tests. In patients over 35 years of age, whose main aim is the prevention of ischemic disease, stratification should be made with echocardiography, coronary artery tomography and cardiac magnetic resonance and even coronary angiography (CA).1 Within CA it can be mentioned that, as in patients with deep myocardial bridges, prolonged pressure on the coronary arteries during systole and early diastole can decrease coronary blood flow. In these cases, intravascular ultrasound (IVUS) offers a superior resolution to obtain images of the coronary arteries throughout the cardiac cycle and, therefore, is designated as a class IIa indication to identify the mechanisms of coronary flow restriction. In 10% of 31 patients who were evaluated with IVUS presented ischemia refractory to nitroglycerin in which it was necessary to place stents. It has been proposed that OCT could give a better spatial evaluation of the vessel than the IVUS. The evaluation of the fractional flow reserve (FFR) with a cut-off point of 0.8 demonstrates the existence of congenital alterations of the coronary arteries.4
The treatment of congenital anomalies of the coronary arteries is focused on three principles: medical treatment and follow-up, coronary angioplasty with stenting and surgical repair.1,3,4 The primary objective of these three options of treatment is the prevention of sudden death. The medical treatment is based on beta-blockers combined with the limitation of physical activity. The percutaneous treatment with stenting is indicated in those cases with origin in the opposite side and that present reverse ischemia by nuclear medicine as in patients with stenosis by IVUS of more than 50% in comparison with the distal lumen of the vessel or in those patients who present severe symptoms and high risk of sudden death.4
The surgical treatment of the anomalous origin of the coronary arteries, is indicated in those in which left circulation has an anomalous origin and a large amount of myocardial tissue is at risk and in those anomalous origins that show obstructive injury or have an intraarterial pathway.1,4,6 Although there is not much evidence about the behavior in this type of patients, the therapeutic decision is based on the symptoms as well as on the risk stratification. Nowadays, there are on-going studies that will assist to take better decisions.4











 nueva página del texto (beta)
nueva página del texto (beta)



