Introduction
Chronic degenerative diseases such as type 2 diabetes mellitus (DM2), systemic arterial hypertension and dyslipidemia, have been on the rise in the present century and are considered as cardiovascular risk factors (CVRF) as well as tobacco consumption.1-3 The metabolic syndrome (MetS) is defined as the association of different metabolic risk factors that predispose to the development of cardiovascular disease and type 2 diabetes mellitus. The National Education and Cholesterol Program (NCEP ATP III) defines it as the presence of abdominal obesity, glucose intolerance, dyslipidemia, and hypertension.4,5
The acute coronary syndrome (ACS) accounts for approximately 80% of cases of sudden death in adults and in most of them represents the first and last clinical manifestation.6,7 Contrast induced nephropathy (CIN) is defined as the absolute increment of serum creatinine (sCr) ≥ 0.5 mg/dL or an increment more than 25% of basal creatinine, without any other identified cause over a period of 48 hours after exposure to contrast material.8-10
CIN is the third cause of hospital renal lesion, only next to hypoperfusion and drug toxicity. A prior renal damage is the most important risk factor according to the risk scale of Mehran, placing the patients in a high-risk group.11-13 The reported incidence of CIN ranges from 1-2% in patients without renal failure with preexisting renal disease and in the presence of non-modifiable risk factors (RF), it increased up to 25%. Risk factors are divided into 2 categories: I. Non-modifiable factors: age > 75 years, type 2 DM, systemic arterial hypertension, renal insufficiency (sCr > 1.5 mg/dL or creatinine clearance < 60 mL/min), heart failure, hepatic cirrhosis, renal transplant, multiple myeloma, acute myocardial infarction and nephrotic syndrome.
II. Modifiable factors: dehydration, hypotension, non-steroid anti-inflammatories, use of diuretics, use of > 140 mL of contrast medium, repeated application of contrast material in periods shorter than 24 hours, hypoalbuminemia, use of nephrotoxic antibiotics and anemia.14-18
There are few studies referable to the impact of MetS on the development of CIN, post elective percutaneous coronary intervention (PCI) in non-diabetic patients, where CIN occurred with higher frequency in patients with MetS compared with those without it.19-23
Few studies have been performed in patients with infarction code with and without MetS, associated with CIN. MetS is alarmingly increasing in our population, so the aim of our study was to identify whether patients with ACS plus MetS have a higher risk of developing CIN than those without MetS.21,24,25
Material and methods
A prospective, observational, longitudinal, and comparative study was conducted during the period May 1, 2017 to January 30, 2018 at the Hospital de Especialidades «Antonio Fraga Mouret» del Centro Medico Nacional «La Raza» (HECMN), Instituto Mexicano del Seguro Social. The project was authorized and registered by the local health research committee with number 3501, R-2017-3501-49.
The study was performed in patients with ACS admitted to the Coronary Care Unit (CCU) or the Intensive Care Unit (ICU), and after PCI for their continuous monitoring, given the high risk of electrical or mechanical complications that may arise from the ACS itself or from PCI. The contrast medium (CM) employed in the Cath Lab was Omnipaque, a hydro soluble, non-ionic CM (350 mg of iodine/mL). The employed dose was calculated based on the formula: 5 mL of contrast per kilogram body weight/sCr (mg/dL) (maximum dose of 300 mL).26 MetS was diagnosed based on the NCEP ATP III criteria (abdominal obesity, glucose intolerance, dyslipidemia, and hypertension). The CIN was defined as the absolute increase in serum creatinine ≥ 0.5 mg/dL or an increase more than 25% of basal creatinine without any other identified cause within 48 hours after exposure to the CM.7,15,27,28
Patients were divided into two groups according to their characteristics: group A, patients with MetS and group B, without MetS. Only were selected, patients with acute coronary syndrome, with sCr ≤ 1.2 mg/dL and with glomerular filtration rate (GFR) ≥ 60 mL/min prior to PCI. These measurements were estimated by the formula of Cockcroft-Gault (140-age) (kg weight)/sCr mg/dL (72) or (0.85 in women).11 Later, during their stay in ICU or CCU, sCr was measured at 24 and 48 hours.
Statistical analysis: a descriptive analysis of each of the variables of the two groups expressed in frequencies, percentages and relative risk (RR) was done. Quantitative free distribution variables were summarized in median and measurement of dispersion was conducted with interquartile ranges, (IR) 25 and 75. The statistical test for analysis of free distribution quantitative variables was performed with Mann Whitney U test. For categoric variables, a bivariate analysis was performed with Chi-square (χ2) test. Variables showing to be significant were further analyzed using logistic backward stepwise regression with likelihood-ratio and a confidence interval of 95% p = 0.05. All statistical analyses were performed using IBM’s software SPSS v 20. p values ≤ 0.05 were significant.
Results
Four hundred twenty patients with infarction code were studied: 323 men (76.9%) and 97 women (23.1%), with a mean age of 62 years for men and 64 for women, interquartile range (IR) 56-70 years. Successful PCIs were 357 (85%) and failed PCIs 63 (15%). The population was divided into two groups: group A with MetS 176 (41.9%) and group B without MetS 244 (58.1%). CIN was more frequent in men, 53 (12.6%) compared with women, 19 (4.5%). However, the stratified analysis did not reveal statistically significant differences between the two genders for the occurrence of CIN: RR:0.853, CI:95% 0.532-1.36, (p = 0.513) (Table 1).
Table 1: Analysis of logistic regression of independent risk factors for contrast induced nephropathy with primary percutaneous coronary intervention.
| Risk factor | RR | CI | p |
|---|---|---|---|
| Male gender | 1.93 | 0.69-2.21 | 0.4660 |
| Smoking | 1.12 | 0.66-1.92 | 0.6520 |
| Type 2 diabetes mellitus | 1.96 | 1.14-3.36 | 0.0130* |
| Metabolic syndrome | 2.05 | 1.33-3.15 | 0.0012* |
| ACS inferior localization | 1.11 | 0.72-1.71 | 0.6000 |
| ACS anteroseptal | 1.11 | 0.69-1.80 | 0.6500 |
| Bivascular disease | 1.33 | 0.87-2.05 | 0.1860 |
| Multivessel disease | 1.52 | 1.0-2.3 | 0.0500* |
ACS = Acute coronary syndrome, RR = Relative risk, CI = Confidence interval 95%.
* p < 0.05.
The presence of CIN was found in 72 patients (17.1%), of whom 43 (10.2%) were from group A and 29 (6.9%) from group B, RR: 2.05, CI: 95% 1.33-3.15, (p = 0.0012). The average elevation in sCr at 48 hours in the group A was by 1.88 mg/dL. CI: 95% 1.82-1.91, (p = 0.001). We observed that patients with type 2 DM without MetS 94 (22.4%) showed a RR: 1.96, CI:95% 1.14-3.36, (p = 0.013). The comorbidities found in group A were in order of frequency as follows: systemic arterial hypertension 157 (37.3%), visceral obesity 142 (33.8%), dyslipidemia 102 (24.2%) and glucose intolerance 34 (8%) which are all components of MetS. Eighty percent of patients presented three components of MetS and 20% had the four components. The prevalence of type 2 DM with MetS was 136 patients (32.4%) (Table 2).
Table 2: Characteristics of patients with acute coronary syndrome who developed or not contrast induced nephropathy.
| n = 420 | Group A n = 176 n (%) |
Group B n = 244 n (%) |
p |
|---|---|---|---|
| Sex | M = 124 (29.5) | M = 199 (47.4) | 0.0800 |
| W = 52 (12.4) | W = 45 (10.7) | ||
| Mean age, IR. | 62 (60-64) | 64 (62-66) | 0.0470* |
| Smoking | 137 (32.6) | 193 (46) | 0.7570 |
| Sedentary lifestyle | 165 (39.3) | 231 (55) | 0.6880 |
| Systemic arterial hypertension | 157 (37.3) | 59 (14.0) | 0.0010* |
| Visceral obesity | 142 (33.8) | 34 (8.0) | 0.0010* |
| Dyslipidemia | 102 (24.2) | 74 (17.6) | 0.0010* |
| Glucose intolerance | 34 (8.0) | 142 (34.4) | 0.0440* |
| Previous infarction | 34 (8.0) | 25 (6.0) | 0.0080* |
| Type 2 DM | 136 (32.4) | 94 (22.4) | 0.0001* |
| CIN | 43 (10.2) | 29 (6.9) | 0.0012* |
| sCr: 48 hours mg/dL (CI) | 1.88 (1.82-1.91) | 1.02 (0.87-1.2) | 0.0010* |
| Contrast media mL. IR | 120 (100-153) | 120 (100-153) | 0.8680 |
DM2 = Type 2 diabetes mellitus, CIN = Contrast induced nephropathy, IR = Interquartile range, mL = Milliliters, sCr = Serum creatinine, CI = Confidence interval 95%.
*p < 0.05.
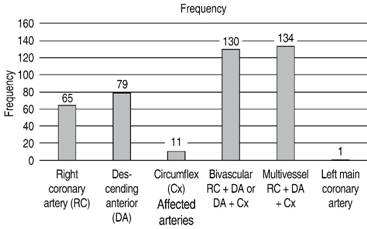
The electrocardiographic localization of ACS was: inferior 158 (37.6%), anteroseptal 109 (26%), and extensive anterior 66 (15.7%). ACS of inferior and anteroseptal localization showed a RR for CIN of 1.11, CI: 95% 0.72-1.71 (p = 0.608) and RR: 1.11, CI: 95% 0.69-1.80, (p = 0.650) respectively. Of these patients, 253 (60.2%) received thrombolysis, and 167 (39%) did not, with an average door-to-needle time of 2 hours with CI: 95% 1.92-2.01, (p = 0.011). Angiographically, the results were as follows: multivessel disease 134 (31.9%), bivascular 130 (31%), anterior descendent 79 (18.8%). RR: 1.52, IC:95% 1.0-2.3, (p = 0.05) (Table 3andFigure 1).
Table 3: Clinical, electrocardiographic and angiographic data, patients with and without contrast induced nephropathy.
| CIN n = 72 n (%) |
Without CIN n = 348 n (%) |
RR | CI | p | |
|---|---|---|---|---|---|
| Sex | M: 53 (73.6) | M: 270 (77.6) | 1.000 | 0.63-1.61 | 0.9680 |
| W: 19 (26.4) | W: 78 (22.4) | 1.930 | 0.69-2.21 | 0.4660 | |
| Type 2 DM | 49 (68.0) | 181 (52.0) | 1.966 | 1.14-3.36 | 0.0130* |
| Metabolic syndrome | 43 (59.7) | 133 (38.2) | 2.050 | 1.33-3.15 | 0.0012* |
| Without metabolic syndrome | 29 (40.2) | 215 (61.7) | 0.486 | 0.31-0.74 | 0.0800 |
| ACS inferior | 29 (40.3) | 129 (37.1) | 1.110 | 0.72-1.71 | 0.6080 |
| ACS A/S | 20 (27.8) | 89 (25.6) | 1.110 | 0.69-1.80 | 0.6500 |
| # Affected vessels | |||||
| 1 | 15 (20.8) | 141 (40.5) | 0.440 | 0.26-0.75 | 0.0010* |
| 2 | 27 (37.5) | 103 (29.6) | 1.330 | 0.87-2.05 | 0.1860 |
| 3 | 30 (41.7) | 104 (29.9) | 1.520 | 1.0-2.3 | 0.0500* |
CIN = Contrast induced nephropathy, DM2 = Type 2 diabetes mellitus, ACS = Acute coronary syndrome, A/S = Anteroseptal, RR = Relative risk, CI = Confidence interval 95%.
*p < 0.05
The average time since arrival from a referral hospital to the hemodynamics room was 10 hours IR: 8-12 hours. Patients admitted with ACS in Killip Kimball class I (KK I): were 393 (43.6%), KK II: 17 (4%), KK III: 10 (2.4%). Of these, CIN occurred en KK I: 66 (16%), KK II: 4 (5.5%), KK III: 2 (2.7%), p = 0.824. The duration of the procedure was 45 average-minutes, IR: 40-60 min. The amount of CM (Omnipaque, a hydro soluble, non-ionic, contrast material) employed had a median of 120 mL, IR: 100-153 mL (p = 0.868). No association was observed between the amount of CM used and the development of CIN.
Discussion
In this study it was found that patients with ACS plus MetS, who underwent PCI presented twice as much the risk for CIN as those without MetS. Likewise, it was found that patients with bivascular and multivessel disease, showed a higher risk for CIN compared with the remaining angiographic findings.
CIN is a frequent complication in patients who undergo PCI. In the present study, patients with prior renal damage, which is an unmistakable RF for CIN were not included.14,25,29 The already known RF inherent to the patient like type 2 DM were similar to those reported in the literature.3,10 Furthermore, there are several studies in the literature of patients with previous renal damage or an elective population for the performance of a diagnostic PCI, where they found that prior renal damage was a RF for the development of CIN as established by the study of Mehran.8 Another study reported that MetS is a RF for CIN in a cohort of 219 patients studied during three years, where only patients over 60 years of age and with mild to moderate impairment of renal function were included.3,8,16 However, in or study we included patients with a mean age of 63 years, with ACS that did not present alteration of the renal function prior to PCI and in this way, it was decreased the bias caused by the previous alteration of renal function and thus showing the association between MetS and the development of CIN.12,16
The risk age for CIN in our population was10 years less than that reported in the literature and no statistically significant difference between genders was found for the presence of CIN. This contrast with other reports in that there is a higher risk in a population over 70 years of age with a greater prevalence in men.9,10,16
As expected, combined hyperlipidemia, simple hypercholesterolemia, MetS, and low HDL-c have been associated with multivessel coronary artery disease independent of other CVD risk factors.25,26,30 According to our results we also found that in multivessel coronary artery disease was associated to MetS and CIN.
ACS with inferior and anteroseptal localization proved to be a RF, although without statistically significant difference. Of the total of patients admitted with ACS, the greatest percentage was seen in KK I prior to PCI, and only 2.4% was in stage III which improved after the performance of PCI. No association was observed between the KK class III and the development of CIN. This could be due to the fact that there were only10 patients in KK III.
CIN is a diagnosis that connotes a great responsibility to the clinician, thus it is of utmost importance to know that patients with metabolic syndrome have a risk for CIN. This knowledge will allow us to employ the necessary therapeutic strategies in order to protect the patient and decrease the incidence of CIN.
Therefore, we suggest the following: 1. Every patient should have a sCr determination prior to exposure to a contrast medium. 2. The patient should be adequately hydrated prior to PCI. 3. Use an isoosmolar CM and 4. Do not use more than 120 mL of CM. One last suggestion is to monitor sCr and urinary output every 24 hours.
In case of detecting CIN, the following are proposed: optimize patient’s hydration; prepare management for acute renal failure and optimize hemodynamic stability in order to keep satisfactory tissue organ perfusion, as well as to bear in mind that MetS is a RF for the occurrence of CIN.
Among the limitations of our study, it is important to mention that we did not have a follow up of the patients after discharge from the hospital where they spent three days. Therefore, we consider it necessary to conduct a study following these patients during the whole hospitalization period and to know whether CIN remitted or progressed to renal function replacement therapy.











 nueva página del texto (beta)
nueva página del texto (beta)