Introduction
The main objective in the treatment of ST segment elevation (STE) myocardial infarction (STEMI) is the prompt restoration of coronary flow and microvasculature.1 The presence of T-wave inversion (TWI) in leads with ST-segment elevation (STE) is classicaly considered as the natural progression of non-perfunded STEMI.2 The presence of TWI after reperfusion therapy has been considered as a sign of succesful therapy.1,3-5 The presence of early TWI (before the reperfusion strategy) has not been well established. Previous studies have reported that the presence of an early TWI in leads with STE before primary percutaneous coronary intervention (pPCI) is associated with a patent infarct-related artery (IRA).6,7 We analyzed the prevalence of early TWI in leads with STE in a group of patients admitted with a diagnosis of STEMI who arrived within three hours of symptoms onset and underwent pPCI.
Methods
Study population
We did a retrospective cohort study, with 622 consecutive patients admitted at the emergency department of the National Cardiology Institute in Mexico City with a diagnosis of STEMI who arrived within three hours of symptoms onset and underwent primary percutaneous coronary intervention (p-PCI) from October 2005 to November 2015. We excluded 190 patients (161 for having an incomplete file, 28 for having left or right bundle branch block and one for being in a idioventricular rhythm).
Electrocardiographic analysis
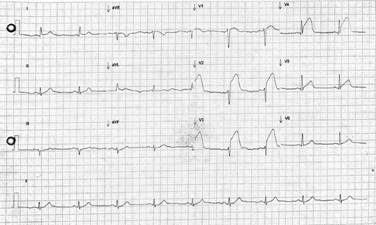
As described elsewhere6,7 patients were divided into two groups: those with TWI (≥0.5 mm below the isoelectric line) in two or more adjacent leads with STE (Figure 1) and those with positive T waves (PTW) in two or more adjacent leads with STE (Figure 2). If a patient had a biphasic T wave it was considered negative if the terminal portion was ≥ 0.5 mm below the isolectric line.
Angiographic analysis
Patients were taken to the catheterization laboratory as fast as possible (all of them had a time of onset of symptoms-angiogram of less than 12 hours), and were divided in two groups: non patent IRA, with a TIMI flow grade 0-1; and patent IRA with a TIMI flow 2-3. This analysis was made by blinded expert in interventional cardiology.
Statistical analysis
Categorical variables were compared using χ2 and continous variables with Wilcoxon rank sum test. Sensibility, Specificity, positive predictive value and negative predictive value were obtained using a 2 x 2 Table including true positives, true negatives, false positives and false negatives. The software used was SPSS version 15.0 (SPSS, Inc, Chicago, Illinois) a p ≤ 0.05 was considered statistically significant.
Results
432 consecutive patients who presented with STEMI and underwent pPCI were included in the study. Baseline characteristics of the two groups are presented in Table 1. 386 (89.3%) patients presented with PTW and 46 (10.6%) with TWI.
Table 1: Baseline characteristics.
| Characteristics | T-wave inversion (n = 46) |
Positive T-wave (n = 386) |
p-value |
|---|---|---|---|
| Age ± SD (years) | 61.5 ± 11.8 | 58.2 ± 11.7 | 0.078 |
| Males n (%) | 38 (82.6) | 343 (88.9) | 0.226 |
| Smokers n (%) | 9 (19.6) | 144 (37.3) | 0.017 |
| Dyslipidemia n (%) | 22 (47.8) | 149 (38.6) | 0.227 |
| Hypertension n (%) | 24 (52.2) | 202 (52.3) | 0.984 |
| Diabetes mellitus n (%) | 17 (37.0) | 102 (26.4) | 0.131 |
| Previous infarction n (%) | 16 (34.8) | 88 (22.8) | 0.072 |
| Previous PCI n (%) | 10 (21.7) | 55 (14.2) | 0.179 |
| Previous CABG n (%) | 4 (8.7) | 7 (1.8) | 0.005 |
| Previous use of aspirin n (%) | 17 (37.0) | 98 (25.4) | 0.093 |
| Previous use of statin n (%) | 12 (26.1) | 78 (20.2) | 0.353 |
| Previous stable angina n (%) | 11 (23.9) | 59 (15.3) | 0.133 |
| Creatinine clearance < 60 mL/min n (%) | 15 (32.6) | 69 (17.9) | 0.017 |
| Killip-Kimball | 0.863 | ||
| I | 38 (82.6) | 318 (83.0) | |
| II | 6 (13.0) | 56 (14.6) | |
| III | 1 (2.2) | 4 (1.0) | |
| IV | 1 (2.2) | 5 (1.3) | |
| TIMI risk | 0.133 | ||
| 0-4 | 35 (76.1) | 327 (84.7) | |
| 5 | 11 (23.9) | 59 (15.3) | |
| TIMI flow | 0.006 | ||
| 0 | 21 (45.7) | 255 (66.8) | |
| 1 | 4 (8.7) | 42 (11.0) | |
| 2 | 15 (32.6) | 56 (14.7) | |
| 3 | 6 (13.0) | 29 (7.6) | |
| Death | 4 (8.7) | 17 (4.4) | 0.260 |
Baseline characteristics including gender, age, dyslipidemia, hypertension, diabetes mellitus, previous PCI, previous use of aspirin and statin, stable angina and death were comprabale between the groups. There were more current smokers in the PTW group than in the TWI group (19.6% vs 37.3% p = 0.017), there were more patients with previous CABG (8.7% vs 1.8% p = 0.005) and more patients with diminished creatinine clearance, defined as a creatinine clearance less than 60 mL/min using the MDRD formula (32.6% vs 17.9% p = 0.017) in the TWI group than in the PTW. We found more patent IRA in the TWI group than in the PTW group (32.6% vs 17.9% p = 0.017). The most frequent IRA was the left anterior descending (LAD) accounting for 198 (45.8%) patients in the overall sample and 26 (56.5%) in patients with TWI (Table 2).
Table 2: Infarct-related artery and the presence of TWI and PTW.
| Infarct-related artery p = 0.28 for both groups |
T-wave inversion (n = 46) | Positive T-wave (n = 386) |
|---|---|---|
| Anterior descending n (%) | 26 (56.5) | 172 (44.6) |
| Left circumflex n (%) | 1 (2.2) | 41 (10.6) |
| Right coronary n (%) | 17 (37.0) | 151 (39.1) |
| Diagonal n (%) | 0 (0.0) | 6 (1.6) |
| Obtuse marginal n (%) | 0 (0.0) | 9 (2.3) |
| Posterolateral n (%) | 0 (0.0) | 1 (0.3) |
| Posterior descending n (%) | 1 (2.2) | 2 (0.5) |
| Venous bypass n (%) | 1 (2.2) | 2 (0.5) |
| Ramus intermedius n (%) | 0 (0.0) | 2 (0.5) |
The presence of early TWI in anterior leads were associated with patency of the anterior descending artery (LAD) (18 [69.2%] vs 41 [24%]; p < 0.001) but not in other arteries (Table 3). Thus, the sensitivity of TWI to predict spontaneous reperfusion in anterior STEMI was 30.5%, specificity was 94.2%, positive predictive value was 69.2% and negative predictive value was 76.1%.
Table 3: Infarct-related artery and patency.
| Infarct-related artery | TIMI flow | TWI (n = 46) | PTW (n = 386) | p-value |
|---|---|---|---|---|
| LAD n (%) | 0 | 6 (23.1) | 109 (63.3) | < 0.001 |
| 1 | 2 (7.7) | 22 (12.7) | ||
| 2 | 13 (50.0) | 25 (14.5) | ||
| 3 | 5 (19.2) | 16 (9.3) | ||
| Left circumflex n (%) | 0 | 1 (100.0) | 23 (56.1) | 0.857 |
| 1 | 0 (0.0) | 6 (14.6) | ||
| 2 | 0 (0.0) | 8 (19.5) | ||
| 3 | 0 (0.0) | 4 (9.8) | ||
| Right coronary n (%) | 0 | 13 (76.5) | 108 (73.0) | 0.648 |
| 1 | 2 (11.8) | 10 (6.8) | ||
| 2 | 2 (11.8) | 21 (14.2) | ||
| 3 | 0 (0.0) | 9 (6.1) | ||
| Diagonal n (%) | 0 | 0 (0.0) | 5 (83.3) | NV |
| 1 | 0 (0.0) | 1 (16.7) | ||
| 2 | 0 (0.0) | 0 (0.0) | ||
| 3 | 0 (0.0) | 0 (0.0) | ||
| Obtuse marginal n (%) | 0 | 0 (0.0) | 5 (55.6) | NV |
| 1 | 0 (0.0) | 3 (33.3) | ||
| 2 | 0 (0.0) | 1 (11.1) | ||
| 3 | 0 (0.0) | 0 (0.0) | ||
| Posterolateral n (%) | 0 | 0 (0.0) | 1 (100.0) | NV |
| 1 | 0 (0.0) | 0 (0.0) | ||
| 2 | 0 (0.0) | 0 (0.0) | ||
| 3 | 0 (0.0) | 0 (0.0) | ||
| Posterior descending n (%) | 0 | 1 (100.0) | 1 (50.0) | 0.386 |
| 1 | 0 (0.0) | 0 (0.0) | ||
| 2 | 0 (0.0) | 1 (50.0) | ||
| 3 | 0 (0.0) | 0 (0.0) | ||
| Venous bypass n (%) | 0 | 0 (0.0) | 2 (100.0) | 0.083 |
| 1 | 0 (0.0) | 0 (0.0) | ||
| 2 | 0 (0.0) | 0 (0.0) | ||
| 3 | 1 (100.0) | 0 (0.0) | ||
| Ramus intermedius n (%) | 0 | 0 (0.0) | 2 (100.0) | NV |
| 1 | 0 (0.0) | 0 (0.0) | ||
| 2 | 0 (0.0) | 0 (0.0) | ||
| 3 | 0 (0.0) | 0 (0.0) |
NV = not valid.
Discussion
The current AHA and ESC guidelines recommend early reperfusion therapy (less than 12 hours from symptom onset) in patients presenting with STEMI.1,8 The electrocardiographic evolution of a non-treated STEMI includes apparition of Q-waves and T-wave inversion.9 The reason we excluded the patients who presented with more than three hours of symptom onset is that the TWI may be due to the normal progression of a non-reperfunded STEMI.
In the context of reperfusion (pPCI or thrombolysis) TWI has been shown to predict a succesful reperfusion.3-5,10 Theoretically the same phenomena could be seen in patients with spontaneous reperfusion. Alsaab and Hira showed that early TWI in patients with anterior STEMI predicted a patent IRA. Our analysis showed similar results. The presence of a patent IRA at the moment of the angiogram is correlated with less mortality, heart failure, need for intubation and less length of stay.11,12
There were little differences between the two groups, there were more current smokers with a PTW than TWI. Smoking has been associatied with endotelial disfunction and coronary artery disease.13 Several endotelial disfunction predictors of a non-patent IRA have been described such as elevated uric acid levels, neutrophil/lymphocyte index,14 platelet/lymphocyte,15 and low levels of endotelin-1;16 also, patients presenting with spontaneous reperfusion have less oxidative stress.17 All of this evidence may explain the difference between both groups in our study.
There were more patients with renal failure and previous CABG in the TWI group, which may be due to the fact that these patients already had TWI prior to the STEMI event because of pre-existing ischemia.
A hypothesis of why this novel electrocardiographical sign is only present in the LAD-related STEMI is because the lateral and inferior infarcts have more collateral circulation from the LAD, not the other way round when this artery is occluded; the LAD is the artery that supplies more irrigation to the left ventricular mass, which may explain more ECG changes when more ventricular mass is involved. Other possible hypothesis includes preconditioning because a oclusion-recanalization phenomena.
Limitations
The limitations in our study are its retrospective, one-center design; the vast majority of the patients didn’t have a previous ECG for comparisons; we measured TIMI flow grade, however, It has been shown that the TIMI myocardial blush grade is a more sensitive predictor of outcomes. It will be important to make a prospective study with echocardiographic studies, blush grade and grade of collaterals and see the long-term prognosis of this presentation.











 nueva página del texto (beta)
nueva página del texto (beta)