Introduction
Hypertension (HT) is one of the major public health problems worldwide. In 2015, the prevalence of HT in adults worldwide was 22.1%.1 It is a risk factor for developing cardiovascular diseases such as coronary heart disease, peripheral vascular disease, stroke, and kidney failure.2,3 Together with cardiovascular abnormalities associated with HT, they are considered the leading cause of death and responsible for 13% of all deaths globally.4 In Mexico, the latest report from the National Health and Nutrition Survey Half Way 2016 (ENSANUT MC 2016; for its acronym in Spanish) reported that the prevalence of HT was 25.5%, meaning 1 in 4 adults have the disease.5
Unfortunately, in most countries around the world, indigenous communities have social, economic and health services disadvantages, compared to the general population.6 The Yaqui indigenous are an ethnic group living in the State of Sonora in several well-connected communities, distributed in rural and urban areas, where they have been gradually assuming westernized lifestyles, and acquiring the Spanish language.7
According to a study conducted in 2008, the prevalence of obesity and type 2 diabetes among the Yaqui indigenous were 48.1 and 18.3%. In addition, the community was characterized by high rates of alcohol consumption and smoking. On the other hand, the lifestyle (diet and physical activity) adopted by this tribe contributes to greater caloric intake and more sedentary physical activities. These determinants are well known risk factors for the development of cardiovascular disease. In fact, the prevalence of total hypertension was 6.3% in the adult population,8 but the percentage of people with HT may have increased in recent years. Therefore, the objective of this study was to describe factors associated with a previous diagnosis of HT in a group of Yaqui adults from Sonora, Mexico.
Material and methods
We conducted a cross-sectional epidemiological study to evaluate the prevalence of previous diagnosis of HT and its associated factors in the Yaqui indigenous population. This indigenous group is in the south-central region of the state of Sonora, Mexico, located between the municipalities of Guaymas, Bácum, and Cajeme (Figure 1). All villages that are part of the Yaqui indigenous area were included. The study was conducted from July to August 2016 and was approved by the Ethics Committee of the Centro de Investigación en Alimentación y Desarrollo, A. C. (Figure 1).
A non-probabilistic sample of 108 subjects was included in this study. Subjects from each village were selected proportional to the number of their inhabitants based in the last census reported by INEGI [Vícam Switch (41 subjects), Pótam (25), Loma de Bácum (10), Loma de Guamúchil (8), Vícam Pueblo (6), Tórim (5), Rahum (5), Huiribis (4) and Belem (4)]. Recruitment was completed in the homes of participants after a complete explanation of the study protocol. All participants signed the informed consent form before participation in this study. The inclusion criteria were age ≥ 18 years and signing the informed consent form. We excluded pregnant women and subjects who did not wish to participate in the study.
HT was considered a prior diagnosis based on whether or not the subject self-reported they had the disease. Subjects were asked, «Do you know if you have hypertension or high blood pressure?». The prevalence of a previous diagnosis of HT adjusted for age and sex in the overall population was estimated along with the age-adjusted prevalence by sex. Anthropometric assessment, medical history and sociodemographic questionnaires were also administered.
The medical history questionnaire administered to participants asked for information about a previous diagnosis of HT and diabetes, and the use of medication for HT and diabetes. Information on other illnesses, health services, and smoking status was also collected. The sociodemographic questionnaire asked for information on the characteristics of the subject including age, sex, occupation, civil status and educational level.9
The anthropometric assessments were body weight, height, and waist circumference. Body weight (kg) was measured with the participant in a standing position, without shoes or personal belongings, and with the least amount of clothing or light clothing. A digital electronic scale with a capacity of 200 kg ± 100 g (Seca 813) was used for this measurement. Height (cm) was measured to the Frankfurt plane while the subject was standing (without shoes). We used a portable stadiometer (Seca 213) with an error range of approximately 0.05 mm. Body Mass Index (BMI) was calculated with body weight in kilograms (kg) divided by height in meters squared (m2).9 The criteria of the World Health Organization (WHO) were used to categorize BMI as normal (18.5-24.9 kg/m2), overweight (≥ 25 kg/m2) and obese (≥ 30 kg/m2). Waist circumference (cm) was measured with a fiberglass tape graduated in millimeters (Gulick, with scale from 0 to 150 cm), based on the technique proposed by The International Society for the Advancement of Kinanthropometry. The subject was standing, and the tape was placed at the narrowest part between the edge of the lower rib and the iliac crest. The diagnosis of central obesity was ≥ 90 cm for men and ≥ 80 cm for women, according the classification proposed by the International Diabetes Federation (IDF).10
Statistical analysis
Statistical analysis was performed with STATA software version 14 (StataCorp LP, College Station, Texas, USA). The averages were expressed as the mean ± S.D. Student’s t-test was used for comparison between groups for continuous variables, and χ2 and Fisher exact tests were used to compare proportions between groups. The sex- and age-adjusted prevalence of a previous diagnosis of HT in the overall population and age-adjusted prevalence by sex were estimated by the direct method of standardization using the analyzed sample as the standard population. Factors associated with a previous diagnosis of HT were determined using multiple logistic regression analysis. The response variable was previous diagnosis of hypertension, and the predictor variables were age, sex, previous diagnosis of diabetes, waist circumference, locality, reading and writing skills, use of tobacco, marital status, educational level and health services.
In order to build the preliminary model, we first performed univariate analysis (p ≤ 0.2 and biological plausibility) followed by stepwise model selection (p ≤ 0.05). Finally, the preliminary model was evaluated for interaction (p ≤ 0.1), collinearity (r > 0.7) and multiple logistic regression assumptions (linearity).
Results
A total of 108 subjects (80 women and 28 men) belonging to the Yaqui community in the State of Sonora participated in the study. The mean age in the whole population was 41.5 ± 13.9 years, with no differences between men and women (p > 0.05). Table I shows the anthropometric characteristics of the population, in which there was a significant difference in BMI by sex (29.7 ± 5.7 kg/m2 for women and 25.7 ± 4.4 kg/m2 for men, p = 0.001). There was a similar finding when BMI was categorized, with women having a larger percentage of overweight and obese subjects than men (29.1 vs. 14.2% for overweight and 46.8 vs. 32.1% for obesity). For central obesity, women also had a higher percentage of central obesity than men (83.7 vs. 60.7%, p = 0.0120). The other variables were not different between the two groups (p > 0.05). For HT, 12.0% of the population reported having a previous diagnosis of HT. Similarly, 14.8% of subjects had a previous diagnosis of diabetes. Table I also summarizes the characteristics including smoking status, education and civil status of the participants.
Table I: Anthropometric, sociodemographic, and clinical characteristics of the study participants.
| Characteristics | Total (n = 108) | Women (n = 80) | Men (n = 28) | P-value |
|---|---|---|---|---|
| Age (years)† | 41.5 ± 13.9 | 41.3 ± 13.9 | 42.1 ± 14.1 | 0.7784 |
| Body weight (kg)† | 74.2 ± 14.9 | 73.3 ± 15.0 | 76.6 ± 14.5 | 0.3150 |
| Height (cm)† | 160.8 ± 8.6 | 156.8 ± 4.9 | 172.3 ± 5.9 | < 0.0001* |
| BMI (kg/m2)† | 28.7 ± 5.6 | 29.7 ± 5.7 | 25.7 ± 4.4 | 0.0010* |
| Waist circumference (cm)† | 94.5 ± 13.0 | 95.2 ± 12.5 | 92.6 ± 14.4 | 0.3672 |
| Categorical BMI‡ | 0.0190* | |||
| Normal BMI | 34 (31.7) | 19 (24.0) | 15 (53.5) | |
| Overweight | 27 (25.2) | 23 (29.1) | 4 (14.2) | |
| Obesity | 46 (42.9) | 37 (46.8) | 9 (32.1) | |
| Central obesity‡ | 84 (77.7) | 67 (83.7) | 17 (60.7) | 0.0120* |
| Previous hypertension‡ | 13 (12.0) | 11 (13.7) | 2 (7.1) | 0.5070 |
| Previous diabetes‡ | 16 (14.8) | 14 (17.5) | 2 (7.1) | 0.2310 |
| Smoking status‡ | < 0.0001* | |||
| No smoker | 85 (78.7) | 71 (88.7) | 14 (50.0) | |
| Occasional smoker or frequent smoker | 23 (21.3) | 9 (11.2) | 14 (50.0) | |
| Schooling‡ | 1.0000 | |||
| No formal school or primary school | 35 (34.3) | 26 (34.6) | 9 (33.3) | |
| Secondary school | 42 (41.1) | 31 (41.3) | 11 (40.7) | |
| High school or university | 25 (24.5) | 18 (24.0) | 7 (25.9) | |
| Civil status‡ | 0.1410 | |||
| Single, widower or separate | 51 (47.6) | 41 (51.9) | 10 (35.7) | |
| Married, cohabiting or other | 56 (52.3) | 38 (48.1) | 18 (64.2) |
BMI = Body Mass Index; P-value = comparison by t-test, χ2 and Fisher exact tests between genders (for numeric variables and categorical variables).
1: Significant differences (p ≤ 0.05).
†: reported as the mean ± SD (standard deviation).
‡: reported as n (%).
Moreover, of the 13 subjects with HT, only 61.5% (8 subjects) mentioned receiving treatment with prescribed drugs. Among those who reported having diabetes, only 37.5% (6 subjects) mentioned taking medication to control it.
In the Yaqui community, the crude prevalence of a previous diagnosis of HT (self-reported) was 12.0% (95% CI 5.8-18.2) for the total population, 7.1% (95% CI -3.0-17.3) for men and 13.7% (IC 95% 6.0-21.4) for women. Figure 2 shows the adjusted prevalence of a previous diagnosis of HT. The sex- and age-adjusted prevalence was 12.0% (95% CI 6.3-17.6) in the overall population. The age-adjusted prevalence in men was 7.1% (95% CI 0.00-16.0), and it was 14.0% (95% CI 6.9-21.1) for women. There was no significant difference when comparing the prevalence of a previous diagnosis of HT by sex (p = 0.355).
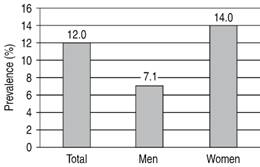
Figure 2: Sex- and age-adjusted prevalence of a previous diagnosis of HT in the overall population and age-adjusted prevalence by sex.
Table II shows the result of the multiple logistic regression analysis using previous diagnosis of HT as the dependent variable. Factors associated with a previous diagnosis of HT among the Yaqui indigenous were waist circumference (cm) and a previous diagnosis of diabetes (p ≤ 0.05), each of which was adjusted by each other and by sex.
In the Yaqui community, higher waist circumference was independently associated with an increased possibility of being diagnosed with HT (OR 1.07; 95% CI 1.01-1.14). Having been diagnosed with diabetes was also independently associated (OR 4.14; 95% CI 1.03-16.61) with an increased possibility of being diagnosed with HT than those subjects who did not have a previous diagnosis of diabetes (Table II).
Table II: Multiple logistic regression analysis using a previous diagnosis of HT as the dependent variable.
| Variable | Final multivariate model | |
|---|---|---|
| Odds ratio (95% CI) | P-value | |
| Waist circumference (cm) | 1.07 (1.01-1.14) | 0.010 |
| Previous diabetes (yes) | 4.14 (1.03-16.61) | 0.045 |
CI = confidence interval (95%). Variables in the model were adjusted by each other and by sex.
Discussion
The sex- and age-adjusted prevalence of a previous diagnosis of HT was 12.0% in the overall population. This number (12.0%) exceeded that reported in a study done in 2008 in the Yaqui community in a sample of 158 subjects, which had reported a prevalence of HT of 6.3% in its inhabitants.8 The prevalence found in our study was nearly twice that found in this previous study.
There is a possibility that the real prevalence, which includes previous diagnoses and new cases, will be higher. It has been reported in other studies that most people do not know they have this disease because it is asymptomatic.11,12 The previous diagnosis of HT can be seen as also indicating timely medical attention, effective diagnostic programs and/or good health service protocols.13 Strong health services programs provide medical attention and thus promote increased diagnostic coverage, particularly for HT. As previously mentioned, the percentage of subjects who had treatment for this disease was 61.5%. Unfortunately, we cannot report the percentage of individuals with control of the disease, as blood pressure was not measured.
According to the data released by the National Health and Nutrition Survey 2012 (ENSANUT, 2012), the prevalence of a previous diagnosis of HT was 16.6% nationwide. The prevalence of new cases of HT was 14.9%. Therefore, the total prevalence of HT was 31.5% among Mexicans adults in 2012.13 It can be clearly seen that the prevalence of a previous diagnosis of HT was roughly half of total HT prevalence in 2012. In addition, it was reported that 73.9% of people with a previous diagnosis of HT had drug treatment.13 Four years later, in the ENSANUT MC 2016, the prevalence of a previous diagnosis of HT was 15.3%, and the prevalence of new cases was 10.2%,5 changing the ratio of previous to new diagnoses of HT from 1 to 1.5. This report shows an increase in the percentage of people with pharmacological treatment of 79.3%.5 In both cases (ENSANUT 2012 and 2016) the percentage of subjects with treatment was higher than that reported in the Yaqui community (61.5%). Therefore, the differences in medical care for this indigenous group can be observed with respect to the rest of the national population. Using information from the ENSANUT 2012 and 2016, regarding the relations between previous and new diagnoses of HT (1-1 and 1-1.5, respectively), we can estimate that the total prevalence of HT in the Yaqui indigenous would be approximately 18-24%. The variations between the previous diagnoses of HT speak to the opportune diagnoses being carried out by the health sector at national level. At the state level, in 2012, Sonora reported 13.5% of new cases of HT, and while the prevalence of a previous diagnosis of HT was not mentioned, the total prevalence was 38.0%. Thus, Sonora was placed between the five states of the Mexican Republic as having a higher prevalence of HT. It is noteworthy that these states are in the north of Mexico.13,14
A study conducted in Malaysian adults reported a prevalence of previous diagnosis of HT of 25.4%, with 72.3% of those diagnosed under pharmacological treatment for this disease.15 Both the people who knew they had HT and those who were taking medication were higher compared to the indigenous Yaquis. The higher prevalence of previous diagnosis of HT and the higher proportion of people under treatment may be due to the improvement of public health and primary care mediations by the health sector that have been undertaken in this population.15
Another study conducted in an indigenous population in Fulani, Cameroon reported a prevalence of total HT of 26.6%. The proportion of people classified with previous diagnosis were 4.4%, and only 2.4% used medication to control it.16 This indigenous community lacks health services for better detection of this type of disease and have low socioeconomic standing, as reflected in the data presented.16 On the other hand, countries such as the U.S.A. have a higher percentage of previous diagnosis of HT since 82.9% of men and 80.3% of women know that they have HT. The high percentage of adults who have received a diagnosis speaks to an increased availability of health care in the U.S.A.17 In Mexico, it has been reported that subjects who have medical service are more likely to have a previous diagnosis of HT and diabetes compared to subjects without medical service affiliation.18 In the Yaqui community, a social program is currently being carried out to help low-income families belonging to the ethnic group. This social program provides support for the feeding of people through food pantries and it also provides medical services, improving the diagnosis of chronic diseases. However, not all families have the support of this program.
We found that waist circumference (cm) and a previous diagnosis of diabetes (self-reported) were independently associated with receiving a previous diagnosis of HT. Some studies have found the same associated factors.19,20 According to the results obtained in the study, a higher waist circumference was associated with an increased possibility of being diagnosed with HT (OR 1.07; 95% CI 1.01-1.14) in the Yaqui indigenous population. Similar results were reported in a cross-sectional study in Brazilian women for whom waist circumference was associated with higher HT (OR 1.02; 95% CI 1.00-1.05).21 According to an analysis derived from the ENSANUT 2012, people with higher BMI (dose response) are more likely to have had a previous diagnosis of HT. Women with obesity were 3.31 times as likely to have had a previous diagnosis of HT as women with low BMI (OR 3.31, 95% CI 1.48-7.44). While men with obesity were 3.41 times as likely to have had a previous diagnosis of HT as men with low BMI (OR 3.41, 95% CI 1.42-8.17).18 Similarly, in adults in Southern China it was found that overweight and obese subjects were more likely to have a previous diagnosis of HT (OR 1.7, 95% CI 1.4-1.9 and OR 1.8, 95% CI 1.5-2.3, respectively).22
Diabetes was associated with 4.14 times the odds of being diagnosed with HT compared with subjects who did not have diabetes (OR 4.14; 95% CI 1.03-16.61). The higher HT for people with diabetes in the Yaquis indigenous population is similar to that found in other studies. In the same study cited above (the ICMR-INDIAB study), an association between diabetes and HT was also found. Subjects with diabetes were 1.56 times as likely to have been diagnosed with HT as subjects who did not have diabetes (OR 1.56; 95% CI 1.35-1.80).23 Another cross-sectional study in a population of adults in Gondar, Northwest Ethiopia revealed that subjects who had diabetes (self-reported) were 4.15 times as likely to have had HT than subjects who did not (OR 4.15; 95% CI 1.77-9.72).24 This result was very similar to that found in our study, though it is curious that previous diabetes prevalence in the Yaquis indigenous population was 14.8%, while in the study population in Gondar, it was only 6.3%. Both communities have similar lifestyles and high prevalence of obesity and diabetes in its inhabitants.
Both the increase in waist circumference (abdominal obesity) and diabetes were associated with HT. This relationship can be seen from a biological point of view where both diseases affect the Sympathetic Nervous System (SNS) and the Renin Angiotensin Aldosterone System (RAAS), thus contributing to the development of the disease (HT).25 People with these conditions (obesity and diabetes) usually visit the doctor more often for attention and control. Therefore, they are exposed to more routine revisions, for which a timely diagnosis of HT is possible. A study reported that people with high blood pressure were more aware of having diabetes due to the monitoring of their disease (HT).26 In Mexico it was reported that 93.8% of people with diabetes monitored their blood pressure at least once a month when they went to the health center.27 Also, as previously mentioned in the Yaqui community, a social program is being implemented that provides health services to people, including a routine medical check-up. On the other hand, there may be barriers to people not attending health services, such as acceptability, accessibility, contact, and availability.28 A study conducted on indigenous people in Guatemala reported geographical (distance), economic (consultation and medication prices) and cultural (language and other beliefs) barriers preventing people from seeking medical services.29
Yaqui Indians live in conditions of low socioeconomic status, which can hinder good medical care. Health centers are necessary to provide care, and while the new social program for low-income families is a good source of support, not all people have access to this program. It is important to implement similar social support programs of greater magnitude for increased opportune diagnosis of chronic diseases.
Some limitations of this study should be mentioned. In this work only data of previous diagnosis of hypertension were included in the analysis. Due to the non-probabilistic sampling used and the relative small sample size, this work is not intended to be representative of the Yaqui population. However, the information reported may be important and it is not contradictory with that found in similar studies. Future studies in this community should be more representative and, with sufficient sample sizes, include additional information related to sociodemographic, dietary, physical activity, and some biomarker variables related to hypertension.
Conclusions
In conclusion, the prevalence of a previous diagnosis of HT was high, and it could be higher after confirmation of new cases in the population. Higher waist circumference and diabetes were factors associated for HT. The identification of factors associated with HT may be useful for creating programs to prevent chronic diseases in this ethnic group.











 nueva página del texto (beta)
nueva página del texto (beta)



