Introduction
A simultaneous occurrence of acute coronary events and anaphylactic allergic reactions was described by Kounis and Zavras in 1991. Possible etiologies of Kounis syndrome (KS) have been recognized as food, environmental, and drug reactions associated or not with previous cardiovascular risk factors.1-3
According with the 2010 Acute Myocardial Infarction Delay study cut, which includes more than 120 Spanish hospitals, acute myocardial infarction with transient ST-segment elevation represents 4.6% of all cases that are admitted to the Intensive Care Unit, where the most KS cases are, representing a small part of this etiology.4
The KS has been divided into 3 subtypes: Type I (without coronary disease), characterized by chest pain during allergic reactions in patients without risk factors, with secondary electrocardiographic changes and normal cardiac enzymes, or progression to acute myocardial infarction. Type II (with coronary disease): it starts with chest pain during an allergic reaction, in patients with atheromatous disease who present plaque rupture and release of activated mediators, yielding to the development of acute myocardial infarction.2,5 Type III. Recently described as thrombosis of drug-eluting stent, due to the infiltration of mast cells and eosinophils identified by Giemsa and hematoxylin-eosin staining.6,7
Although any drug can trigger an allergic reaction, the most frequently signaled are beta-lactams antibiotics, non-steroidal anti-inflammatory medications (NSAIDs), general anesthetics and iodinated contrast agents.8
Case report
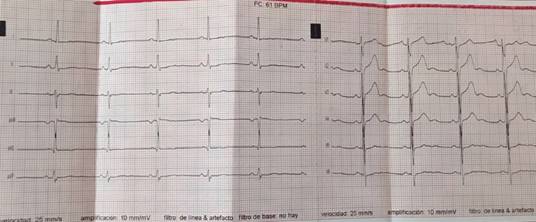
We present the case of a 47 year-old male patient, public employee, born in Mera, resident in Puyo City (Pastaza-Ecuador), with a history of atopic dermatitis since childhood and sulfonamides drug-related fixed erythema 10 years ago. Three months prior to admission the patient presented acute pharyngitis, which was treated with ibuprofen prescribed by primary care physician. Subsequently, he had pruritus on his elbows and knees with periods of exacerbation and spontaneous remission. Two days prior to admission he reported having suffered generalized headache, so he ingested ibuprofen in an auto-medicated way, after which he had precordial pain of moderate intensity, that not improved with rest and was accompanied by palpitations. He was admitted to the emergency room, where a blood pressure of 100/60 mmHg, a heart rate of 120 beats per minute and body temperature of 36.2 oC were found. ECG showed sinus rhythm and ischemic changes (Figure 1). Cardiac enzymes were normal. Treatment was established by protocol for non-ST elevation acute coronary syndrome (NSTEACS). During the hospitalization, pruritus at the level of elbows, buttocks and abdomen recurred associated with scaly erythematous lesion converging in plaques. A skin biopsy was performed which reported superficial and deep perivascular dermatitis with eosinophilic infiltrate compatible with drug reaction and atopic dermatitis; allergic test was performed which was positive for NSAIDs. The risk of ischemia subsequent of NSTEACS was stratified with an ergometric test with Bruce protocol, reaching 98% of the estimated heart rate for the age without presenting symptoms or electrocardiographic alterations. CT scan did not reveal any coronary lesions (Figure 2).

Figure 1: 12-lead electrocardiogram on admission with chest pain, symmetric inverted T wave in DI, aVL, V5 and V6 leads.
It was concluded, in view of NSTEACS associated to a manifest allergic process, that the patient had a type I of KS. Prednisone was prescribed in tapering doses while loratadine; clopidogrel, bisoprolol, simvastatin, acetylsalicylic acid were suspended. The evolution has been favorable and until now the patient has remained asymptomatic. No significant changes were observed in the control electrocardiogram (Figure 3).
Discussion
KS is a condition, frequently underdiagnosed and with poorly understood epidemiology. Diagnosis can be done from clinical suspicion, when allergic signs and symptoms are accompanied with coronary events.
In the analysis of an international database of pharmacovigilance, 51 cases of KS were identified, occurring more often in male subjects (prevalence 63%) between 22 and 46 years. The drugs more commonly found involved were NSAIDs (31 cases reported).9
The treatment of KS should counteract allergy and cardiac symptoms: corticosteroids with H1 and H2 inhibitors, are the most useful antihistamines since drugs such as vasodilators, nitrates or calcium channels blockers may worsen the condition, reversing their cardiovascular effect and producing hypotension and tachycardia. According to the Galaxy guideline, adrenaline is a drug of first choice in anaphylaxis but its use in Kounis syndrome is risky because it can provoke arrhythmias, prolongation of QT interval, aggravate myocardial ischemia or cause vasospasm. For all these reasons its use is restricted.8-10
When we are facing a KS type I, treating the allergic symptoms may be a priority whereas, when treating a patient with previous coronary disease, a simultaneous treatment is necessary. The utility of acetylsalicylic acid is unknown in KS since it can aggravate anaphylaxis or even be a cause of an allergic reaction, but when its use is essential must be administered in the intensive care unit. Patients with KS type II and known allergy to aspirin may be candidates for desensitization.6
Conclusions
The KS is an underdiagnosed entity due to a lack of knowledge of its pathophysiology. So far, this case is the second reported in Ecuador11 and the first one associated with NSAIDs. Finally, as in the international literature there is no guide for the management of KS, it has crucial importance that clinicians, cardiologists, emergency room specialists and primary care physicians know how to recognize the association of allergic reactions with acute coronary syndromes, to establish the earliest and more accurate treatment, according to the needs of the patient.











 nueva página del texto (beta)
nueva página del texto (beta)