Introduction
Diabetes is a major health problem with the numbers of diabetics increasing both in Mexico and globally. Cardiovascular disease is the leading cause of mortality and morbidity in the diabetic population.1 When compared with non diabetics, diabetics have a worse outcome after cardiovascular therapeutic interventions.2-4 Diabetes is a major risk factor for stroke5 and diabetics make up 11-40% of patients undergoing carotid endarterectomy (CEA).4 Further, diabetes appears to be a major predictor of adverse in this population.6 Recently carotid artery stenting (CAS) has emerged as a viable alternative to CEA.7 The impact of diabetes on outcome of patients undergoing CAS remains unknown. We accordingly evaluated the short and long term outcome of diabetic patients undergoing CAS at our institution.
Material and methods
Observational, retrospective, comparative and descriptive study. We included 279 patients/341 lesions with significant carotid artery stenosis; in all cases, an informed written consent was obtained before the procedure. Monitoring was conducted by clinical record in the outpatient and telephone follow-up at 30 days, 6 months. Eligible patients were considered for carotid angioplasty with stent (CAS) if any of the following high-risk variables was present: 1) age > 75, 2) bilateral disease, 3) contralateral occlusion, 4) high or low ostial lesion, 5) multivessel coronary disease associated with unstable angina, 6) left ventricular ejection fraction (LVEF) < 45%, and 7) symptomatic lesion with stenosis > 50% and/or asymptomatic injury > 70%. Patients were considered high risk when they had three or more of the aforementioned risk factors (Fx).
Technique
All patients underwent a clinical neurological evaluation and Doppler study. The vascular Doppler study was performed before each procedure by personnel accredited by the Mexican Society of Radiology. Prior to the CAS, a load of 300-600 mg clopidogrel was administered under the judgment of the operator, and 325 mg of aspirin; once the femoral arterial sheath was placed, 70 U/kg of IV heparin were applied; the arterial puncture site was femoral in the vast majority of cases; lidocaine 2% without epinephrine was used as a local anesthetic; sedation was not used in order to maintain a constant neurological condition; both blood pressure and O2 saturation were monitored during the procedure. A description of our endovascular technique has been published previously.8 All carotid percutaneous procedures were performed by the group of interventional cardiologys assigned to the hemodinamyc department.
Definitions in angioplasty/carotid stent
Angiographic success: stenosis postprocedure less that 30% through quantitative angiography.
Clinical success: to get a stenosis ≤ 30% without major complications (stroke, death, surgery or acute myocardial infarction) at 30 days.
Transitory ischemic attack: (hemispheric) neurological event with full recovery within 24 hours of its occurrence.
Minor cerebral vascular event: slight neurological event that causes neurological damage (≤ 3 in the National Institute Health Stroke Scale [NIHSS] scale), with recovery
Major cerebral vascular event: neurological injury that persists for more than 30 days and increases its severity to > 4 according the NIHSS scale.9
Statistical analysis
An analysis of the study variables and their distribution with measures of central tendency and dispersion was performed. Continuous variables are presented as means with standard deviation (SD) or medians with minimum and maximum according to their distribution. Categorical variables are presented as frequencies and percentages. Continuous variables were assessed using the Kolmogórov-Smirnov test for normality and Levene’s for homogeneity of variances. Subsequently, a comparative analysis of each of the variables grouped according to gender and the presence or absence of the primary and secondary endpoints was performed; the latter were also compared in subgroups of symptomatic and asymptomatic patients according to gender with the Student t test or Mann-Whitney U test -depending on the distribution of the groups- for continuous variables and chi square for categorical variables. The analysis of event-free survival was performed by Kaplan-Meier curve. All this was done with the SPSS 20.0 statistical package.
Results
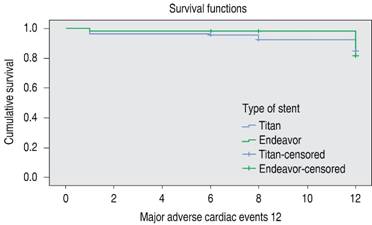
A total of 279/341 patients/arterial stenosis injuries who underwent carotid stenting were evaluated. Of these, 173 (50.7%) were diabetic and 168 (49.3%) were non-diabetic. In Table I, the demographic variables analyzed and compared in both groups are shown. As for the group of diabetic patients, there were more men (59.5%) than women (40.5%). Twenty-four (13.9%) were older than 75 years and a large percentage (84.4%) had hypertension (HAS) and hypercolesterolemia (79.8%). A small percentage of these patients had a left ventricular ejection fraction < 45% (37.3%), in contrast with the number of coronary arteries affected: 54.3% had at least three diseased vessels, and 43.9% of the cases had been previously intervened for coronary angioplasty; 30.6% had a history of prior CVE and 68.2% (118 patients) were asymptomatic. In addition, about 50% were classed as «high risk» and therefore had a high EuroSCORE. In all patients, the features of the procedure, the approach, previous carotid Doppler, use of distal protection devices, presence of thrombotic material extracted, type of stent used, and the clinical and angiographic procedural success were evaluated, among others (Table II). A high percentage of diabetic patients (77.5%) were previously assessed through carotid Doppler. The procedure took place through a femoral approach in most cases (96.5%); only six of them were approached radially because of the presence of bovine bow. In most injuries (91.9%), embolic protection filters were used, obtaining atherothrombotic material in 53.2% of the cases. Closed-cell stents (Carotid WALLSTENT-Boston Scientific Corp.) were the most commonly used (73.4%), compared to open-cell stents (Precise JJ, Inc.) (26.6%). As for the features of the stent, the diameter ranged from 7.96 ± 1.078 mm and the length from 35.95 ± 6.08 mm. The percentage of stenosis was assessed using criteria of NASCET,10 with a preprocedure stenosis percent of 79.1 ± 12.27% and postprocedure of 9.9 ± 11.07%. The reference diameter for angiography preprocedure was 6.14 ± 1.32 mm, and postprocedure, 1.34 ± 6.34 mm. Finally, in almost all patients the lesion was predilated and the stent postdilated, obtaining clinical and angiographic success in 95% of the cases. Angiographic success was considered when an arterial stenosis postprocedure was less than 30% (by quantitative angiography or QCA), and clinical success was obtained when a stenosis of less than 30% without major complications (stroke, death, surgery or AMI [acute myocardial infarction]) was achieved within 30 days of the study. Finally, the in-hospital MACE are shown in Table III, and are detailed below. In the group of diabetic patients, a cardiovascular morbidity (fatal and non-fatal AMI) of four individuals (2.3%) and a neurologic morbidity (fatal and non-fatal stroke) of four people (2.3%) was registered. Among those diabetics who underwent cardiovascular surgery, there was a hospital mortality of 4.6%, higher compared to non-diabetics (0.6%), with p = 0.02. The diabetic versus non-diabetic patient who underwent coronary artery bypass surgery had more coronary and multivessel disease as well as previous myocardial infarction; 57.8 vs 42.2%, 57.1 vs 42.9%, and 60.5 vs 39.5% respectively p = 0.049; so also those who died have lower LVEF 44.1 + 10.1% vs 56.1 + 6.09% p = 0.002 . No cases of reangiographic stenosis occurred in the diabetic group, while the non-diabetics had a restenosis rate of 1.9%, with p = 0.077. As for the clinical six-month follow-up (Table IV), cardiovascular mortality was similar in both groups p = NS; of the diabetic patients, 14 underwent cardiovascular surgery (8.8%), with an operative mortality of 1.4% at six months, without a statistically significant difference compared to non-diabetics. Finally, in terms of major clinical events, we observed a higher percentage of transient ischemic attack in the diabetic group (8.7%) compared to the non-diabetics (3.6%), with p = 0.05. There was no significant difference between the groups in terms of greater or lesser CVA (p = 0.732 and 0.329, respectively). In Figure 1 we present, through the Kaplan-Meier (KM) curve, the difference between both groups in free development of adverse events (MACE) within six months after the intervention, assessed with the Mantel-Cox curve: 94.7% for DM and 91.7% for non-DM, p = 0.249 OR (95% CI) 0.604 (0.254-1.435).
Table I: Demographic variables.
| Variable | Non-diabetics 168 (49.3%) |
Diabetics 173 (50.7%) |
p value |
|---|---|---|---|
| Masculine gender | 124 (73.8%) | 103 (59.5%) | 0.005* |
| Feminine gender | 44 (26.2%) | 70 (40.5%) | 0.005* |
| Age > 75 years | 42 (25%) | 24 (13.9%) | 0.009* |
| SH | 135 (80%) | 146 (84.4%) | 0.328 |
| Smoker | 99 (58.9%) | 98 (56.6%) | 0.670 |
| Hypercholesterolemia | 126 (75%) | 138 (79.8%) | 0.292 |
| Previous AMI | 55 (32.7%) | 71 (41%) | 0.112 |
| LVEF < 45% | 37 (24.2%) | 62 (37.3%) | 0.011* |
| No. of diseased vessels | 36 (21.4%) | 25 (14.5%) | 0.227 |
| 1 | 32 (19%) | 27 (15.6%) | |
| 2 | 23 (13.7%) | 27 (15.6%) | |
| 3 | 77 (45.8%) | 94 (54.3%) | |
| Previous PCI | 73 (43.5%) | 76 (43.9%) | 0.929 |
| Previous CVE | 48 (28.6%) | 53 (30.6%) | 0.676 |
| Asymptomatic | 112 (66.7%) | 118 (68.2%) | 0.761 |
| Symptomatic | 56 (33.3%) | 55 (31.8%) | 0.761 |
| Low risk | 97 (57.7%) | 88 (50.9%) | 0.203 |
| High risk | 71 (42.3%) | 85 (49.1%) | 0.203 |
| Low EuroSCORE | 132 (78.6%) | 90 (52%) | 0.000* |
| EuroSCORE > 3 | 36 (21.4%) | 83 (46%) | 0.000* |
| RIC | 98 (58.3%) | 99 (57.2%) | 0.836 |
| LIC | 100 (59.5%) | 106 (61.3%) | 0.741 |
SH = systemic hypertension, AMI = acute myocardial infarction, PCI = percutaneous coronary intervention, CVE = cerebral vascular event, LVEF = left ventricular ejection fraction, LIC = left internal carotid, RIC = right internal carotid.
*Statistically significant.
Table II: Outcomes of the procedure.
| Variable | Non-diabetics 168 (49.3%) |
Diabetics 173 (50.7%) |
p value |
|---|---|---|---|
| Previous Doppler | 133 (79.2%) | 134 (77.5%) | 0.823 |
| Distal protection | 0.392 | ||
| Filter | 158 (94%) | 159 (91.9%) | |
| Distal balloon | 3 (1.8%) | 3 (1.7%) | |
| Proximal balloon | 0 (0%) | 3 (1.7%) | |
| Extracted thrombus | 80 (47.6%) | 92 (53.2%) | 0.305 |
| Access | 0.552 | ||
| Femoral | 164 (97.6%) | 167 (96.5%) | |
| Radial | 4 (2.4%) | 6 (3.5%) | |
| Stent type | 0.395 | ||
| Closed cell | 130 (77.4%) | 127 (73.4%) | |
| Open cell | 38 (22.6%) | 46 (26.6%) | |
| Predilation | 167 (99.4%) | 172 (99.4%) | 0.983 |
| Postdilation | 161 (95.8%) | 160 (92.5%) | 0.188 |
Table III: Results and periprocedural complications (30 days).
| 30-day follow-up | Non-diabetics 168 (49.3%) |
Diabetics 173 (50.7%) |
OR (95% CI) | p* |
|---|---|---|---|---|
| MACE | 9 (5.4%) | 8 (4.6%) | 0.057 (0.322-2.27) | 0.756 |
| CVE major, non-fatal | 2 (1.2%) | 2 (1.2%) | 0.971 (0.0135-6.97) | 0.076 |
| AMI | 4 (2.4%) | 1 (0.6%) | 0.238 (0.026-2.15) | 0.166 |
| Minor CVE | 1 (0.6%) | 3 (1.7%) | 2.08 (0.303-29.7) | 0.329 |
| TIA | 6 (3.6%) | 15 (8.7%) | 2.503 (0.970-6.77) | 0.050 |
| Cardiovascular mortality (fatal AMI) | 2 (1.2%) | 3 (1.7%) | 1.465 (0.242-8.87) | 0.676 |
| Fatal major CVE | 1 (0.6%) | 2 (1.2%) | 1.953 (0.175-21.8) | 0.579 |
| IH cardiovascular surgery performed | 10 (6.0%) | 18 (10.4%) | 1.995 (0.921-1.10) | 0.134 |
| IH surgical mortality | 1 (0.6%) | 9 (4.6%) | 8.097 (1.00-65.5) | 0.020 |
| Major CVE (fatal and non-fatal) | 3 (1.8%) | 4 (2.3%) | 1.902 (0.287-5.90) | 0.732 |
| AMI (fatal and non-fatal) | 6 (3.6%) | 4 (2.3%) | 0.804 (0.241-2.68) | 0.722 |
| Clinical success | 163 (97.0%) | 166 (96.0%) | 0.727 (0.220-2.34) | 0.592 |
| Angiographic success | 197 (99.4%) | 173 (98.3%) | 0.339 (0.035-3.26) | 0.329 |
MACE = major adverse cardiovascular event, CVE = cerebral vascular event, AMI = acute myocardial infarction, TIA = transient ischemic attack, IH = intrahospitalary.
*Statistically significant.
Table IV: Six-month follow-up.
| Six month follow-up | Non-DM: 162 | DM: 158 | OR (95% CI) | p |
|---|---|---|---|---|
| Cardiovascular mortality | 2 (1.23%) | 1 (0.63%) | 0.483 (0.043-5.372) | 0.545 |
| Cardiovascular surgery performed | 8 (4.9%) | 14 (8.8%) | 0.871 (0.354-2.14) | 0.211 |
| Surgical mortality | 0 (0%) | 2 (1.4%) | 0.504 (0.454-0.561) | 0.162 |
| Doppler restenosis | 4 (2.5%) | 5 (3.16%) | 1.220 (0.322-4.62) | 0.789 |
| Percutaneous carotid reintervention | 3 (1.9%) | 0 (0.0%) | 0.488 (0.438-0.544) | 0.077 |
| Accumulated MACE (IH and 6 months) | 14 (8.3%) | 9 (5.3%) | 0.604 (0.254-1.435) | 0.249 |
Non-DM = non-diabetes mellitus, DM = diabetes mellitus, MACE = major adverse cardiovascular events, IH = intrahospitalary.
Discussion
The risk of CVA increases with age, coronary artery disease (CAD), systemic hypertension (SH), hypercholesterolemia, smoking, atrial fibrillation (AF) and other cardiac conditions (cardiomyopathies, valvular disease, congenital heart disease). Specifically, stenosis of the internal carotid artery causes up to 20% of all ischemic strokes, and atherosclerosis remains the main etiology in most cases.11 Diabetes and other major risk factors, have also been associated with significant carotid stenosis. In a study of 1,058 patients evaluated with carotid Doppler, significant stenosis of 70 to 99% was found in 89 patients, moderate stenosis (40-69%) in 85 patients, and mild stenosis (less than 39%) in 884 patients. The risk factors considered were age, gender, alcohol consumption, smoking, CAD, hypertension and DM. Multivariate logistic regression analysis were made, where the three groups were compared. In the significant stenosis group, the gender distribution was 34.8% female and 65.2% male, with a mean age of 64.48 ± 10.19 years. In the second and third groups, these distributions were 51.8% female and 48.2% male, with a mean age of 65.15 ± 9.66 years, and 54.30% female and 45.70% male, with a mean age of 59.56 ± 12.37 years, respectively. DM (OR = 2.77), CAD (OR = 1.67), age (OR = 1.02), and male gender (OR = 1.75) were associated with significant carotid stenosis.12
While the association between ischemic stroke and carotid stenosis is well established, the prevalence of asymptomatic carotid stenosis in patients with DM is uncertain. Nonetheless, De Angelis,13 in 2003, evaluated 365 individuals through carotid Doppler: 187 non-diabetic (89 men, 98 women ) and 178 diabetic (82 men, 96 women). The overall mean age was 67 ± 7.8 years; 66 ± 7.9 for non-diabetics and 67 ± 7.5 for diabetics. A percentage of 10-99% stenosis was determined in 143/365 patients (39.1%), 49/187 non-diabetics (26.2%) and 94/178 diabetics (52.8%). The differences were significant (p < 0.001). A significant percentage of stenosis was found in 17/143 subjects (12%); 12 of them were diabetic (70%) and five non-diabetic (30%). With these results, it was established that diabetics are three times more likely to develop significant carotid stenosis than non-diabetics (OR 3.152, 95% CI 2032-4889).
In another study by P. Lacroix in 2006, in addition to the prevalence of asymptomatic carotid atherosclerosis in a diabetic population, the presence of predictive factors for optimizing the diagnosis was evaluated. He analyzed a total of 300 diabetic subjects (166 men, 134 women) with carotid Doppler. The prevalence of carotid stenosis of 60% or more was 4.7%, and the prevalence of carotid atherosclerosis was 68.3%. Risk factors for carotid stenosis of 60% or more were the presence of diabetic retinopathy (OR = 3.62; 95% CI 1.12-11.73), ankle-brachial index (ABI) < 0.85 (OR = 3.94; 95% CI 1.21-12.84) and personal history of neurological diseases (OR = 4.54; 95% CI 1.16-17.81).14 He then concluded that the prevalence of carotid atherosclerotic disease in diabetics is high, and that in these patients, the probability of finding a significant stenosis is higher among men with a history of CAD and an ABI < 0.85; in the latter group of patients, it is also common to find silent myocardial ischemia, which makes them candidates for close surveillance.15
As for the risk of a CVA in relation to the presence of symptoms in patients with carotid stenosis, it has been determined in the NASCET study that the risk of recurrent ipsilateral stroke in individuals treated conservatively is 4.4% per year for a 50-69% stenosis and 13% per year for a 70% stenosis.16 In contrast, in asymptomatic patients with carotid stenosis of 60%, the risk of stroke is 1-2% per year. However, the risk increases to 3-4% per year in elderly patients, in those with bilateral carotid disease, in people with evidence of silent embolization in brain imaging studies, where there is a heterogeneous carotid plaque, poor collateral circulation, generalized inflammatory state or peripheral arterial disease.17
Among the most important data from our study, we found that 67.4% of the lesions were asymptomatic. Table V shows the results in major complications and death related to the procedure in both groups. We found a higher percentage of men with diabetes carriers of carotid stenosis, which concurs with what is described in the literature worldwide. Similarly, a high percentage of patients with hypertension and associated dyslipidemia was found. DM is a major risk factor for the development of atherosclerotic disease. The incidence per 1,000 people/year of thromboembolic stroke increases with the level of blood glucose. As mentioned previously, the relative risk of developing a stroke associated with DM is 1.4 to 1.7 times greater. Lowering blood sugar levels and controlling blood pressure in individuals with diabetes reduces the risk of stroke by 44%.18,19 It is worth mentioning that a high percentage of our patients were carriers of ischemic heart disease, even with prior PCI, as it was previously described by Kallikasaros,20 who showed that carotid disease (luminal diameter stenosis > 50%) was present in 24.5% of the people with three-vessel disease and 40% of those with left main coronary artery disease. Another important thing that stands out is that half of the cases were considered high risk, which significantly increases the surgical risk, reporting a rise in complications (death, MI, higher CVD, etcetera) between 8 and 15%. Regarding the MACE, no statistically significant difference was found in-hospital and in the six-month follow-up, nor in greater or lesser risk of CVD in both groups of patients (diabetic versus non-diabetic) undergoing carotid stent.
Table V: Results in the asymptomatic group at 30 days: major complications and death related with the procedure.
| Follow-up 30 days | Asymptomatic non-DM: 112 | Asymptomatic DM: 118 | OR (95% CI) | p* |
|---|---|---|---|---|
| TIA | 4 (3.6%) | 8 (6.8%) | 1.25 (0.598-2.61) | 0.577 |
| Major CVE (fatal and non-fatal) | 1 (0.9%) | 3 (2.5%) | 0.444 (0.81-2.42) | 0.270 |
| AMI (fatal and non-fatal) | 1 (0.9%) | 1 (0.84%) | 1.50 (0.181-12.5) | 0.709 |
Non-DM = non-diabetes mellitus, DM = diabetes mellitus, TIA = transient ischemic attack, CVE = cerebral vascular event, AMI = acute myocardial infarction.
It has already been demonstrated that carotid endarterectomy has an incidence of ipsilateral stroke in the medical branch of 11 and 5.1% in the surgical one, obtaining a reduction of 53.7% according to the ACAS (asymptomatic carotid atherosclerosis study), which was conducted on asymptomatic patients with noncritical carotid lesions; 1,662 were recruited and followed for five years.21 In contrast, the benefit in this group of individuals considered «high risk» was demonstrated in the study SAPPHIRE (stenting and angioplasty with protection in patients at high risk for endarterectomy), which included high-risk patients; the endpoints of death/stroke/MI at 30 days in patients randomized to stenting versus carotid endarterectomy were 5.8 vs 12.6%, p = 0.047, and at 12 months, 11.9 vs 19.9%, p = 0.048, favoring endovascular therapy,22 which is similar to our findings (2.9% of hospital mortality related to the procedure and 0.63% at six months in diabetic patients undergoing carotid stent). Only those diabetic patients treated with carotid stent who underwent cardiovascular surgery showed a higher hospital mortality (4.6%) compared with non-diabetics (0.6%), with p = 0.02. Even in non-diabetic patients, there was a higher rate of restenosis (1.8%) compared with diabetics (0%), with a p = 0.077. Finally, in diabetic patients treated with carotid stenting, compared with non-diabetics, increased incidence of cerebral transient ischemic attack (TIA) was observed (8.7 vs 3.6%, with p = 0.05).
Conclusions
According to our results, endovascular treatment of carotid stenosis can be a good alternative to surgical treatment, especially in diabetic and high-risk patients. There is still controversy regarding the choice of definitive treatment of these individuals, whether to perform an endovascular approach or take them to endarterectomy. A total of six large-scale clinical trials with more than 300 patients have been conducted to compare stenting versus carotid endarterectomy. The CAVATAS,23 EVA-3S,24 ICSS25 and SPACE26 studies enrolled only symptomatic individuals. The SAPPHIRE and CREST27 studies included symptomatic and asymptomatic patients at high and conventional risk for surgery, respectively. However, with the current evidence, we can conclude that the results are tipped with a tendency for endovascular therapy. A metaanalysis of 13 clinical trials where 7,484 patients were randomized, of whom 80% had symptomatic disease, showed that carotid stenting was associated with an increased risk of any type of stroke (RR 1.45; 95% CI 1.06-1.99), decreased risk of periprocedural myocardial infarction (RR 0.43; 95% CI 0.26 to 0.71), and no significant increase in mortality (RR 1.40; 95% CI 0.85-2.33).28 Recently were published the results of the CREST trial (long-term results of stenting versus endarterectomy for carotid-artery stenosis) to 10 years. In 2,502 treated patients, there was no significant difference in the rate of the primary composite end point between the stenting group (11.8%; 95% confidence interval [CI], 9.1 to 14.8) and the endarterectomy group (9.9%; 95% CI, 7.9 to 12.2) over 10 years of follow-up (hazard ratio, 1.10; 95% CI, 0.83 to 1.44).29 ACT I trial (randomized trial of stent versus surgery for asymptomatic carotid stenosis) compared carotid-artery stenting with embolic protection and carotid endarterectomy in patients 79 years of age or younger who had severe carotid stenosis and were asymptomatic and were not considered to be at high risk for surgical complications. This study showed that stenting was non inferior to endarterectomy with regard to the primary composite end point (event rate, 3.8 and 3.4%, respectively; p = 0.01 for non inferiority).30 In our study, we observed that despite the high comorbidity of diabetic patients (higher EuroSCORE, multivessel coronary disease, LVEF < 45%, older age), endovascular treatment of carotid stenosis is a good alternative to surgical treatment, especially in the subgroup of diabetic and high-risk patients.











 nueva página del texto (beta)
nueva página del texto (beta)