Introduction
Aortic stenosis (AS) is the most frequent valvular heart disease. As the population is aging, its incidence is further increasing about 2% to 9% in elderly patients. Aortic sclerosis, the precursor of AS is found in 29% of patients older than 65 years. Currently, echocardiography has become the most important examination technique for diagnosis and quantification of AS. It also permits the assessment of left ventricular (LV) structure, function, and associated valve lesions, systolic and diastolic dysfunction, LV hypertrophy like others associated valve lesions.1
In clinical practice, it is important to assess the degree of LV outflow obstruction due to valve narrowing. The differentiation between severe and non-severe stenosis has particular importance because it bears significant consequences for patient management.
As the severity of stenosis increases, concentric LV hypertrophy develops in response to the chronic elevation in LV systolic pressure. In general, the time course of LV hypertrophy development parallels the course of stenosis severity in most patients. As demonstrated by a reduced coronary vasodilator reserve, LV hypertrophy in patients with AS is associated with abnormalities in coronary microcirculatory function.2
The classic symptoms of severe AS include angina, syncope, and dyspnea.3 The current guidelines recommend aortic valve replacement for severe AS in symptomatic or asymptomatic patients when there is impairment of LV function, defined as an ejection fraction < 50%.4,5 Reduction in LV ejection fraction occurs late in the natural history of AS and most patients with severe AS have a normal LV ejection fraction even when symptoms are present. Conversely, LV hypertrophy and abnormal non-invasive measures of LV diastolic function are common in these patients.6,7
Left atrial (LA) size is a recognized marker of increased left ventricular filling pressure and is increased in patients with severe AS.8,9 Because the LA is an asymmetrical cavity, LA size is more accurately reflected by a measurement of volume rather than area or linear dimension.10
Because these information is recognizing that patients with AS less than severe could have important changes in LV morphology, left atrial size and LV diastolic flow patterns, enough to be the cause of severe physical limitations and dyspnea.
The aim of this study was to determine if structural changes in left ventricle, left atrial enlargement, tissue Doppler and pulsed Doppler diastolic flow alterations in patients with aortic stenosis correlate with the degree of the disease and might be associated to indirect signs of increased left ventricle filling pressures.
This study reports the experience with 42 patients with aortic valve stenosis of different magnitudes diagnosed by echocardiography, correlating the LV morphology, LA size and the E/e’ wave ratio.
Methods
The present study comprised 42 patients in a prospective and observational study during a five year period (January 1st 2011 to December 31st 2015). All patients had aortic stenosis in any degree of severity: mild, moderate or severe.
Echocardiographic studies were performed by a cardiologist board certified in echocardiography. Conventional measurements in M-mode echocardiography, two-dimensional, pulsed, continuous, color and tissue Doppler reports were performed using either a Philips echocardiograph model iE33 or a Philips Sonos echocardiograph 5500, using 1-3 MHZ multifrequency transducer, with special emphasis on structure and function of aortic valve. All patients were included in the study. Demographic profiles, findings and measurement were recorded. Variables obtained were: age, sex, left ventricle diastolic diameter (LVDD), left ventricle systolic diameter (LVSD), end-diastole interventricular septum thickness (IVST), end-diastole posterior wall thickness (PWT), LV ejection fraction (LVEF).
Specific measurements were: LV end-diastole thickness/radius ratio (T/R), which was obtained with formula in M mode: posterior wall thickness × 2/diastolic diameter; normal value was established in < 0.42. Left ventricular mass, calculated in M mode using the following equation11: (0.8 × 1.04 ([LVDD + IVST + PWT]3 - [LVDD]3)) + 0.6; normal value was considered < 95 g/m2sc in women and < 115 g/m2sc in men. According to this, four different ventricular geometry were considered: a) normal (normal mass and normal T/R ratio); b) concentric remodeling (normal mass and increased T/R ratio); c) concentric hypertrophy (increased mass and increased T/R ratio) and d) eccentric hypertrophy (increased mass and normal T/R ratio).11,12
Left atrial volume, which was obtained by the biplane Simpson method in apical 2- and 4-chamber views using the built-in software of the machine. For this purpose, LA areas were manually traced at end-systole in apical four- and two-chamber views, ensuring that there was no foreshortening of the atrium. Automatic volume calculation was performed using the software for the modified Simpson’s disc summation method resident in the echo machine. LA volume was indexed to body surface area and expressed as LA volume index (mL/m2). Normal value of left atrium volume was < 29 mL/m2sc.10
Severity of aortic valve stenosis was classified in three categories consistent with accepted criteria: mild, moderate or severe, according to: peak systolic aortic jet velocity, peak and mean systolic aortic gradient and aortic valve area, calculated by continuity equation.4
In the apical four chamber view, using a 1-2 mm sample volume, pulse wave (PW) Doppler cursor is placed between the mitral leaflet tips during diastole. From the mitral inflow profile the E wave was measured.13 The average of early septal and lateral diastolic velocities (e’) were measured by tissue Doppler imaging from the apical four-chamber view. The E/e’ ratio was calculated and a value ≥ 15 was considered as indicative of high LV filling pressures.14
Data analysis was done using SPSS 17, students t test was applied whenever applicable.
Results
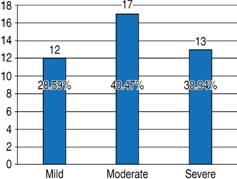
Age mean was 69.76 ± 16.55 years with a range of 31-93 years. Analyzing the age distribution, it was found that 55% of the cases occurred between 60 and 79 years. There was no statistically significant difference between genders when all cases are observed, but there is a statistically significant difference between the groups of 60 and 79 years of age, in which the female gender had a 2:1 preponderance (p < 0.05). A statistically significant difference was also found at age of 80 years or more in which the preponderance of the male gender showed a 4.5:1 relation (p < 0.05) (Table I,Figure 1).
Table I: Demographic data by decades in 42 patients with stenosis of aortic valve.
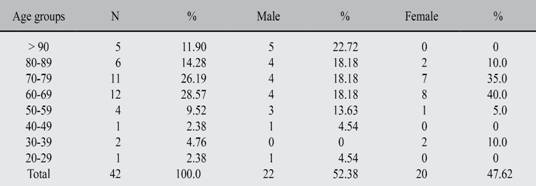
Age mean 69.76 ± 16.55. Range 31-93.
Aortic valve stenosis severity showed 12 cases (28.5%) with mild stenosis, 17 patients (40.5%) presented moderate stenosis and 13 cases (31%) with severe degree (Table II,Figure 2). Specific echocardiographic characteristics among the three groups are listed in Table III.
Table III: Severity of aortic valve stenosis distribution and variables studied by echocardiography.

No statistically significant difference in left ventricular ejection fraction was found in any of the three groups (Table III).
Comparing left ventricular diastolic diameter (LVDD), moderate stenosis presented a greater proportion of dilation than severe ones, when both were compared with cases of mild stenosis (p = 0.05); considering left ventricular systolic diameter (LVSD), the largest increase was observed in moderate stenosis (mean of 5 mm) when it was compared with the mild ones, and decreasing these differences between mild and severe with an average of 3 mm (p = 0.05) (Table III).
Thickness/radius ratio increased by 3 tenths of a point, on average, as the degree of stenosis became more severe with statistically significant difference (p < 0.05). There was a significant increase in left ventricular mass between moderate and severe stenosis when compared to mild stenosis measurements (p < 0.05); however, there was no statistically significant difference between the moderate and severe ones (Table III). Considering the left ventricular geometry, the presence of concentric hypertrophy was found in 11 cases (26.2%), with a similar distribution in the three degrees of severity with no statistically significant difference. The LV concentric remodeling was detected in 15 cases (35.7%), its presence was 3 times more in cases of moderate and severe stenosis (p < 0.05). Eccentric hypertrophy was only detected in two cases (4.8%), one in a patient with mild stenosis and another with moderate stenosis. Finally, LV geometry was classified as normal in 14 patients (33.3%), with the lowest number of normal cases in patients with severe stenosis (p < 0.05) and a similar relationship between mild and moderate stenosis, with no statistically significant difference (Table IV).
Left atrial end-systolic volume increased in 32% in moderate stenosis and 33% in severe cases when compared to mild stenosis; however, the difference was smaller between mild and severe than between mild and moderate, since in moderate stenosis the largest volume of the left atrial was present, which tended to decrease in cases of severe stenosis in 14.5% in relation to moderate ones; the same relation was observed in the volume index of the AI, which corroborates that the calculations are correct (Table III,Figures 3 and 4).
The E/e’ wave ratio provided an index, which was increased as the severity of the stenosis was greater, resulting in 33% higher in moderate stenosis compared to mild stenosis (p < 0.05) and 56% higher in severe compared to mild stenosis (p < 0.05), either both had significant difference (p < 0.05). Left ventricular end-diastolic pressure also showed a linear increase in the three degrees of severity, with an average increase of 26% between mild and moderate, and 38% between mild and severe, both of which were statistically significant (p < 0.05) but there was no significant difference between moderate and severe stenosis (Table III,Figure 5).
Discussion
Aortic stenosis (AE) is the most common valvulopathy in the Western World, in people under 30 years is considered due to congenital valvular abnormality, between 30 and 60 years to a bicuspid valve, whereas in adults over 70 years is due to idiopathic calcification and is denominated senile or degenerative stenosis; currently it is estimated that 5% of the elderly population presents it. The progressive increased afterload in aortic stenosis causes a compensatory left ventricular hypertrophy (LVH) that according to Laplace Law abates parietal stress as mechanism to preserve left ventricular function. About its pathophysiological, the main mechanism of compensation in the increment of the left afterload is the LV concentric hypertrophy seeking to increase its contractility, so that there is a progressive increase of the trans-valvular gradient to maintain the cardiac output.1
The LVH is in part responsible for the relaxation abnormalities and late diastolic left ventricle dysfunction with its inherent increased filling pressures so that the atrial contribution to ventricular filling becomes important. These modifications are associated with LV diastolic dysfunction, so the contribution of atrial contraction to ventricular filling is transcendent. LV diastolic failure increases the pressure in the LV and in the pulmonary vascular bed, which can lead to failure of the right heart and, on the other hand, the LV ejection period is prolonged, trying to compensate the obstruction caused by the aortic valve stenosis.2
From the echocardiographic point of view, the mobility and morphology of the aortic valve can be detected. Using Doppler modalities the systolic gradient can be calculated and the valvular area can be estimated. In addition, it allows assessing the LV function and quantify the aortic valve stenosis severity, it is considered as severe when the valvular area is less than 0.6 cm2/m2 body surface area (less than 1 cm2 in adults). In the presence of normal cardiac output, the LV ejection fraction is conserved, with a mean trans-valvular gradient greater than 40-50 mmHg estimated by Doppler.8
If cardiac output is decreased, caused by ventricular systolic dysfunction with LV ejection fraction < 40%, it is difficult to assess if the valvular area is diminished by the ventricle inability to open the valve completely (pseudo-several stenosis), or there is a true severe stenosis with LV contractile insufficiency producing pressure gradients lower than 40 mmHg. It is important to know the echocardiographic parameters of aortic valve stenosis, because it has a bad prognosis in a short-term (2 to 3 years) when the gradients rise significantly (increase in flow velocity greater than 0.3 m/s). Currently, there are imprecise means of estimation because the Doppler method through which it is assessed may be prone to measurement errors (underestimation of LV outflow tract diameter, misplacement of pulsed-wave Doppler sample in the outflow tract, underestimation of peak gradient by misalignment with flow direction or very eccentric jets).15,16
It has been established three cardinal symptoms as indicative for surgery in severe AS: angina, syncope and heart failure (low left ventricle ejection fraction). Many patients can have dyspnea associated to increased left ventricle filling pressure even with normal ejection fraction and usually is accompanied by left atrial enlargement and increased E/e’ ratio in pulsed wave Doppler (both evaluated in echocardiogram study). In patients with severe AS has been demonstrated that left atrial volume index was significantly higher in symptomatic versus asympromatic patients (41.94 ± 1.98 versus 37.11 ± 2.99 mL/m2sc) and the cutoff point as a predictor of symptoms was stablished in 39.5 mL/m2sc. Likewise E/e’ ratio was significantly higher in symptomatic vs asymptomatic severe AS.17
In this study we found no differences in left atrial size and E/e’ ratio in patients with moderate and severe AS, which suggests that both groups of disease severity should have similar symptoms (dyspnea). Nevertheless patients with moderate stenosis are not considered for surgery, those who have changes in the size of left atrium and the velocity of E and e’ wave, should receive special attention in their treatment in order to improve symptoms.
According to ESC Guidelines and AHA/ACC Guidelines for classification of AS severity18 set out in Table V, it would be possible to add at least 2 more markers like: a) The end-systolic left atrial volume index increased; b) The E/e’ wave ratio index greater than 10 in mild cases, greater than 15 in moderate cases and greater than 18 in severe cases. Finally, the odds about observing left ventricle concentric remodeling increases along with the degree of severity, however it is the parameter with the lowest statistically significant difference.
Table V: Recommendations for classification of AS severity*.
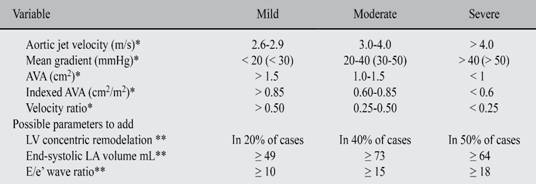
* ESC Guidelines and AHA/ACC Guidelines.
** Parameters studied in this communication.
Main defect of this communication is the small sample studied, but although small, is demonstrative of at least two markers: end-systole LA volume index and the E/e’ wave ratio, because either increased in parallel with aortic stenosis severity degrees. However a larger study is necessary to assert what is found in this work.
Conclusions
Echocardiographic findings in mild and moderate aortic stenosis are in fact compensatory mechanisms, which in long term causes tissue damage with the subsequent left ventricle fibrosis, originating progressive stiffness. Because of these morphological changes can sometimes lead to significant symptoms, the results of the present study might help on the decision making in order to provide myocardial tissue protection through an appropiate and specific treatment.











 nueva página del texto (beta)
nueva página del texto (beta)