Introduction
According to data reported by the World Health Organization (WHO), during 2008, coronary heart disease was the leading cause of death in the world unreachable, being a public health problem in developed countries and increasing significantly in developing countries.1-2
Studies have found that artery stenoses can cause serious adverse cardiac events that could be avoided with 2 types of treatment, one invasive and one conservative.3 RITA-3 study showed that invasive therapy reduced by 50% the incidence of unstable angina without effects on mortality.4
The general suggestion is to make an early invasive treatment to reduce the area of infarct size and thus the mortality of patients as early treatment with improved rates of revascularization.5,6 However studies show that mortality of patients does not differ significantly to a strategy of immediate intervention compared with deferred therapy intervention.7
Unstable angina is a clinical syndrome that is characterized by acute coronary syndrome (ACS), characterized by oppressive or arthritic pain, with or without irradiation that occurs during rest.2,8,9 The SCA is caused by an imbalance between the supply and consumption of oxygen to the myocardial fiber, the most common cause thrombus formation on a pre-existing atherosclerotic plaque presented by erosion and is associated with vasoconstriction.1,10
When an endothelial lesion occurs on the plaque, the subendothelial connective tissue is exposed allowing platelet adhesion and forming a thrombus in the lumen of the vessel, this initiates a complex chain of events that form a hemostatic web that propagates the thrombus in the light occluding the Total partially affected vessel (AI) or (IAM), which in turn produces the above described symptoms.11-13
Clinically diagnosed by the presence of retrosternal burning or squeezing with or without irradiation chest pain and can be accompanied by palpitations, breathlessness, vagal or dysautonomic symptoms, referred pain to the jaw, back or epigastric, starting at rest and the absence of myocardial injury markers in blood.10,14
The treatment of AI focuses on the immediate management of myocardial ischemia and the prevention of adverse outcomes; you can choose between two strategies: invasive strategy (direct catheterization) and conservative (initial stabilization with medical treatment and in case of new recurrences of angina or positive tests for ischemia, performing catheterization).11,15
This treatment uses three types of agents: anti-ischemic: seeking to reduce the lack of oxygen in the heart muscle (oxygen, nitrates, morphine, beta blockers, calcium channel blockers, ACE inhibitor);16,17 antiplatelet: they seek to reduce the formation and propagation of the thrombus blocking platelet activation and aggregation (aspirin, glycoprotein IIb/IIIa receptor antagonists ADP);18 and antithrombotic: preventing thrombus propagation (unfractionated heparin, low molecular weight heparin).19,20
Acute myocardial without ST elevation and unstable angina infarction, continues to generate controversy over whether to diagnose and treat invasively.11,21
Invasive treatments include revascularization with percutaneous coronary procedures (PCI) or coronary bypass surgery.
Today, non-ST segment elevation acute coronary syndrome (NSTE-ACS) is the treatment of choice for coronary angiography, and if revascularization is feasible by percutaneous coronary intervention.12 There is some gender uncertainty due to insufficient statistics; However both women and men should be treated equally.2,22
This treatment has a success rate greater than 90%, improving survival and left ventricular function being the therapy of choice during the first 12 hours of having started the symptoms.23 It is important to improve the post-intervention prognosis, regarding changes in lifestyle and pharmacological treatment, individualizing the risk factors.12,24
Angioplasty is a minimally invasive, safe and effective procedure for the treatment of ischemic heart disease, a disease of high prevalence, which today has a great impact on the morbidity and mortality of the population. The procedure consists in the use of imaging techniques with the objective of guiding a catheter containing a balloon in the distal part of the coronary vessel with stenosis and avoiding myocardial ischemia.25-28
This procedure, in patients suffering from angina of effort, improves the symptoms (pain, dyspnea).11 In patients with acute coronary syndrome (ACS), reduces the risk of heart damage and at the same time prevents the occlusion of the coronary vessel avoiding a heart attack.7,29
Currently, there are several alternative arterial ways such as: brachial, transradial and ulnar; However, femoral arterial access is the most common route of choice, since it facilitates greater rapidity and easy localization because it is a larger caliber vessel.1,3
Like all procedures, complications occur, which in most cases are associated with factors related to both the clinical conditions of the patient and those related to the procedure and materials used.26 In order of frequency, vascular complications, which are associated with calcification of the punctured artery are obesity, sex, age, Hypertension (HTA) and the use of anticoagulants, giving as results hemorrhages, hematomas, fistulas, pseudoaneurysms and ischemia At the puncture site.25,29
Material and methods
From January 2012 to August 2015, an observational, descriptive cross-sectional prevalence study was conducted. This study was performed through the review of clinical records according to the records of the Department of Hemodynamics of the Hospital «Teodoro Maldonado Carbo».
The data were collected from a Table that established the variables taken into account for this study: sex, risk factors, clinical picture, medication use and presence of complications at one month, six months and one year after the process.
With a universe of 283 patients, 99 patients were included according to the inclusion criteria and 184 patients were excluded; 40 (STEMI), 120 (stable angina), 24 (IAMCSST).
Inclusion criteria: clinical diagnosis of unstable angina of more than 12 hours of evolution.
The variables that were taken into account for this study were: gender, is the genetically conditioned genotypic state and determines the gender to which the individual belongs, which may be male or female. The risk factor is defined as the exposure of an individual that increases the likelihood of suffering from a disease. The clinical picture, we define as the set of signs and symptoms that presents an individual and constitute a syndrome. The complication, is a disease or injury that appears during the treatment of a previous disease, which alters the prognosis.
Statistical analysis was performed using Microsoft Word Excel 2007 and SPSS software; we compared the clinical outcomes and complications of patients undergoing this procedure. A basic statistic was performed, analyzing quantitative variables such as age by means of standard deviation. In the case of qualitative variables such as gender, risk factors, clinical picture, medication use and the presence of complications at the month, at six months and in the year; relative frequencies and their respective percentages were obtained.
Chi square (χ2) test was used by Fisher’s test; to determine the relationship between the dependent variable (symptomatic patients) and the variables involved (age, gender, risk factors, clinical picture and medication use) to corroborate the relationship between them, by establishing the statistical significance if it were to exist.
Results
Analyzing sociodemographic and clinical characteristics, with a total of 99 patients, the age of the population was between 30 and 84 years with an average of 60.7 years standard deviation (±) 10.4; Where it was found that the female patients were 24 (24.2%); Compared with the male gender 75 (75.8%).
A pathological history was analyzed, where 79 (79.8%) presented hypertension; 32 (32.3%) had DM 2; 54 (54.5%) presented dyslipidemia, 8 (8.1%) had CRF; 3 (3.0%) had CVD; 78 (78.8%) presented previous AMI and 16 (16.2%) presented smoking (Table I).
Table I: Clinical characteristics of the study population.
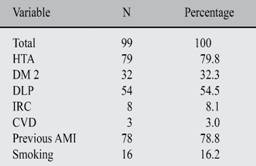
Hypertension = Hypertension. DM 2 = 2 Diabetes mellitus. DLP = Dyslipidemia. IRC = Chronic renal failure.
CVD = Cerebrovascular event. Source = Database research.
Within the study, the use of medication of the 99 patients was analyzed, reporting that; 43 (43.9%) used ACE inhibitors; 42 (42.9%) used ARBs; 73 (74.5%) used Beta Blockers; 91 (92.9%) used ASA; 76 (77.6%) used Tienopyridines and 23 (23.2%) used Ticagrelor (Table II).
Table II: Distribution of patients according to the consumed medication.
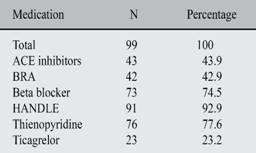
ACE = ACE inhibitor. BRA = Blockers of angiotensin II. ASA = Aspirin. Source = Database research.
All patients who presented with unstable angina of more than 12 hours after angioplasty were operated on in the hospital to rule out any complications of the procedure; Giving as results that of the 99 patients under study; 90 (90.9%) were asymptomatic; 5 (5.1%) had hematoma; 2 (2.0%) death; 1 (1.0%) presented bleeding; 1 (1.0%) presented cardiac shock; While 0 (0%) did not present AMI (Table III).
Table III: Evolution of hospital patients studied.
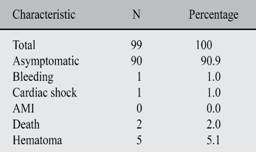
AMI = Acute myocardial infarction. Source = Database research.
Once patients were discharged, their post-intervention evolution at 1 month, at 6 months and at one year was studied. To determine the efficacy of angioplasty.1
Complications were analyzed in order of frequency and time; giving as results: at the month of the intervention it was observed that; 91 (91.9%) were asymptomatic; compared to symptomatic 8 (8.1%); Being dyspnea or angor the only complication in this group. At six months of the intervention it was observed that; 89 (89.9%) were asymptomatic; compared to symptomatic 10 (10.1%); being dyspnea or angor the most frequent complication 6 (6.1%); followed by death 2 (2.0%); SCA 1 (1.0%) and NRV 1 (1.0%). At the year of the intervention it was observed that; 73 (90.1%) were asymptomatic; compared with symptomatic 8 (9.9%), with dyspnea or angor being the only complication (Table IV).
Table IV: Evolution of the population after 1, 6 and 12 months after angioplasty.
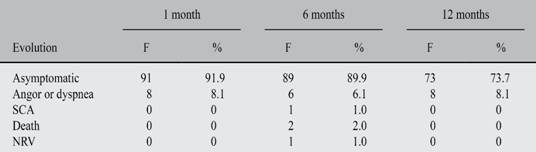
F = Frequency. SCA = Acute coronary syndrome. Source = Database research.
Among the qualitative variables that were analyzed, the presence of complications of these were associated in an intrahospital and out-of-hospital way.
Complications during hospital stay associated with sociodemographic and clinical characteristics; Reported that; within the age group < 60 years 41 were asymptomatic, and one symptomatic attic compared with > 60 years, 49 were asymptomatic and 8 symptomatic giving a p = 0.046; with respect to gender, the female gender presented more complications 6, being 18 asymptomatic; compared to the male 3 which had complications while 18 were asymptomatic, giving a p = 0.002.
Within the pathological antecedents, it was reported that; of all patients with AHT 20 were asymptomatic compared to those without AHT 70 were asymptomatic, and 9 symptomatic patients giving a p = 0.113; Patients with DM2 28 were asymptomatic and 4 symptomatic compared to those without DM2 62 were asymptomatic and 5 were symptomatic, giving a p = 0.415; Patients with dyslipidemia 49 were asymptomatic and 5.
Symptomatic, compared with those who did not present 41 were asymptomatic and 4 symptomatic giving p = 0.949; Patients with CKD 7 were asymptomatic and 1 asymptomatic compared to those who did not have 83 asymptomatic and 8 symptomatic patients giving a p = 0.726; Patients with previous AMI 72 were asymptomatic and 6 were symptomatic compared to that they did not present 18 were asymptomatic and 3 were symptomatic giving a p = 0.351 and patients with a history of smoking 15 were asymptomatic and 1 symptomatic compared with those who did not present 75 were asymptomatic And 8 were symptomatic giving a p = 0.666.
In short-term complications, it was reported that; in relation to age, < 60 years: 32 were asymptomatic and 10 symptomatic, compared with ≥ 60 years: 43 were asymptomatic and 14 symptomatic giving a p = 0.931; male gender: 56 were asymptomatic and 19 symptomatic compared to the female gender: 19 were asymptomatic and symptomatic dand 5 or p = 0.654; patients with hypertension: 62 were asymptomatic and 17 symptomatic compared with those who did not present 13 were asymptomatic and 7 were symptomatic, giving a p = 0.209; Patients with DM2: 25 were asymptomatic and 7 were symptomatic compared to those who did not present 50 were asymptomatic and 17 were symptomatic giving a p = 0.704; Patients with dyslipidemia 42 were asymptomatic and 12 symptomatic compared to what they did not have 33 were asymptomatic and 12 symptomatic giving a p = 0.607; Patients with CRF: 6 were asymptomatic and 2 symptomatic compared to those who did not have 69 were asymptomatic and 22 symptomatic giving a p = 0.958; Patients with CVD 1 were asymptomatic and 2 symptomatic compared to those who did not present 74 were asymptomatic and 22 symptomatic giving a p = 0.082; Patients with previous AMI: 59 were asymptomatic and 19 symptomatic compared to those who did not present 16 were asymptomatic and 5 were symptomatic giving a p = 0.958 and patients with a history of smoking 12 were asymptomatic and 4 were symptomatic in comparison with those who did not present 63 were asymptomatic and 20 symptomatic giving a p = 0.938 (Table V).
Table V: Clinical and sociodemographic variables associated with the presence of hospital and late complications.

Hypertension = Hypertension. DM 2 = Diabetes mellitus 2. DLP = Dyslipidemia.
IRC = Chronic renal failure. CVD = Cerebrovascular event. Source = Database research.
Depending on the use of medication, complications were studied during hospital and late stay; giving as a result: During the hospital stay of the 99 patients who used ACE inhibitors, 41 were asymptomatic and 2 were symptomatic compared to those who did not use 49 were asymptomatic and 6 were symptomatic giving p = 0.262; Those who used BRA, 38 were asymptomatic and 4 were symptomatic compared to those who did not use 52 were asymptomatic and 4 were symptomatic, giving a p = 0.670; Those who used BB 67 were asymptomatic and 6 were symptomatic compared to those who did not use 23 were asymptomatic and 2 were symptomatic giving p = 0.972; Those who used ASA 85 were asymptomatic and 6 were symptomatic compared to those who did not use 5 were asymptomatic and 2 were symptomatic giving p = 0.041; those who used tienopiridinas 70 were asymptomatic and 6 were symptomatic compared to those who did not use 20 were asymptomatic and 2 were symptomatic giving a p = 0.857 and with ticagrelor 20 they were asymptomatic and 3 were symptomatic compared to those who did not use 70 asymptomatic and 6 symptomatic giving A p = 0.452 (Table VI).
Table VI: Drugs associated with the presence or absence of hospital and late complications.
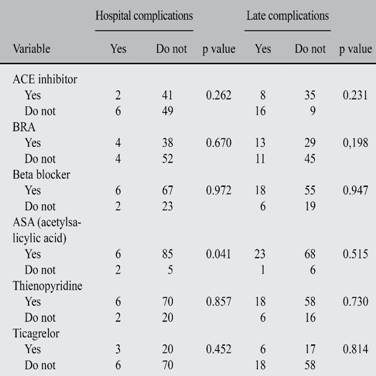
Source = Database research.
Short-term complications reported that patients who used ACE inhibitors 35 were asymptomatic and 8 were symptomatic compared to those who did not use 9 were asymptomatic and 16 were symptomatic, giving a p = 0.231; Those who used BRA 29 were asymptomatic and 13 symptomatic compared to those who did not use 45 were asymptomatic and 11 were symptomatic, giving a p = 0.198; Those who used BB 55 were asymptomatic and 18 were symptomatic compared to those who did not use 19. Were asymptomatic and 6 were symptomatic, giving a p = 0.947; Those who used ASA 68 were asymptomatic and 23 were symptomatic compared to those who did not use 6 were asymptomatic and 1 were symptomatic giving p = 0.515; those who used tienopiridinas 58 were asymptomatic and 18 were asymptomatic compared to those who did not use 16 were asymptomatic and 6 were symptomatic giving p = 0.730 and those who used ticagrelor, 17 were asymptomatic and 6 were symptomatic with those who did not use 58 were asymptomatic and 18 symptomatic patients giving a p = 0.814 (Table VI).
Discussion
From the demographic point of view the results of this study, which began with 99 patients; giving an average age of 60.7, is related to other previously performed tests like MASK, CONAREC that reveal average ages of 60 to 69 ± 11 years, the male gender being dominant 75.8%.21,25
It was corroborated that acute coronary syndrome without elevation of the ST Segment (SCSSEST); As evidenced in the literature is more frequent in male patients with the majority of the population with 75.8%.21 Likewise, it was observed that in terms of the most predominant factors were hypertension risk with 79.8%, previous AMI: 78.8% and 54.5% dyslipidemia, similar data are consistent with research Nilson Lopez et al, in their study clinical characteristics and prognosis of patients with acute coronary syndrome without ST segment elevation and healthy arteries, when reporting; HTA 54.8% and dyslipidemia with 59.3%.12
The presence of intrahospital complications occurred in 10% of the patients. According to the evolution of these patients, 8.1% presented complications at one month, 10.1% at 6 months, and 9.9% at one year after the procedure, dyspnea or angoria being the most frequent complication in The 3 follow-up times. The mortality of patients with unstable angina of more than 12 hours of evolution undergoing angioplasty was nil.
Regarding the general objective of the study, which was to evaluate the efficacy of angioplasty as a treatment in patients with angor of more than 12 hours of evolution; it was found that asymptomatic patients predominated the first.
Sixth and twelfth month after the intervention with an average of 75.76%; Compared with 24.24% of symptomatic patients, whose most frequent complication was angor or dyspnea with 24.1%.
To establish a reference that allows us to verify the efficacy of angioplasty as treatment in patients with unstable angina of more than 12 hours of evolution, we proceeded to calculate the percentages of the main complications, the same ones studied in other analyzes, that report the 41.7% of complications such as bleeding, hematomas, 58.3% were asymptomatic, results that coincide with the present study with an average of 90.0% of asymptomatic patients compared to symptomatic patients with 8.3%.7,24
Within the limitations presented in this study, it can be mentioned that because the collection of data was performed retrospectively through a database, there may be a certain information bias. Similarly, the effects of drugs can not be conclusively measured because 100% of patients consume more than one drug; not to mention the breach it had with it, is a risk factor for future complications.
There is no statistical significance, the comparative results are > 0.05 between clinical and sociodemographic variables associated with the presence of intrahospital and late complications.
Conclusions
After obtaining the results in this study, it can be concluded that invasive therapy with angioplasty in the symptomatology of more than 12 hours of evolution is effective, keeping the largest number of patients asymptomatic without the need for new interventions.
In patients with unstable angina, the most frequent risk factors were hypertension, anterior myocardial infarction and dyslipidemia, evidencing the points on which greater emphasis should be placed on preventing ACS in patients or diagnosing it at an earlier stage to avoid The progression of the same, and in turn the complications that could present. Also, more attention should be paid to male patients, being a risk factor that can not be modified, and of relevance in this syndrome.
Angioplasty is a safe treatment as evidenced, since in spite of having performed it 12 hours after starting the symptomatology, the mortality rate was 0%. It should be noted that there were complications both in hospital and during the time of follow-up, being the most frequent, dyspnea or angor.
Angioplasty is recommended as a treatment for unstable angina even after 12 hours of clinical evolution. The effects of each of the drugs used by patients should be analyzed to better understand their effects on complications.
In gratitude to all who made this publication possible, my colleagues and my beloved institution whom I respect and thank.











 nova página do texto(beta)
nova página do texto(beta)


