Introduction
Carotid sinus hypersensitivity (CSH) is included within the reflex or neurally-mediated syncopes.1 It is defined as a reduction of 50 mmHg or more in arterial blood pressure, the presence of 3 seconds or more asystole (Figure 1) or a combination of both, when carotid sinus massage is applied for ten seconds.2
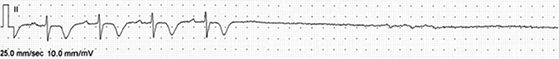
Figure 1: Patient with carotid sinus syndrome. Massage is applied in the right carotid sinus for five seconds in decubitus and a pause of more than 12 seconds with dizziness and fainting is caused.
If the patient has spontaneous syncope and the symptoms are reproduced during carotid sinus massage (CSM), then the patient has a «carotid sinus syndrome» (CSS).
Epidemiology
The incidence of the syndrome (35-40:1 000 000 population per year) has been calculated from the data obtained in several studies performed in the first eighties of the last century.2 The CSS has a prevalence lower than 4% among people younger than 40 years, but it might be as high as 40% in subjects in their ninth decade of life that attend a syncope unit.
Up to 8.8% of the patients with unknown origin syncope have carotid sinus hypersensitivity, mainly of the cardioinhibitory sub-type (81%).3
The syndrome is predominant in men (2:1 ratio) and in most studies, the patients have a mean age of 75 years.
Among patients with syncope, it is common to have several co-existing dys-autonomic reflexes. A study by the group of Brignole in one-hundred patients, found that 79 of them had a positive response to some of the different provocative maneuvers (tilt testing, carotid sinus massage, eye compression).4 They found that from a group of 44 patients (24 with positive CSM, 20 with positive tilt test), nineteen had both positive CSM and tilt test.
Our group has found 22 subjects in the last six years that had symptoms associated to changes in the heart rate or blood pressure induced by carotid sinus massage. Only eleven patients had the diagnostic criteria defined by the guidelines (reduction in systolic BP higher than 50 mmHg and or sinus pauses longer than three seconds).
Among these eleven patients, the average age is 77.7 ± 8.4 years, there are four male subjects and seven women.
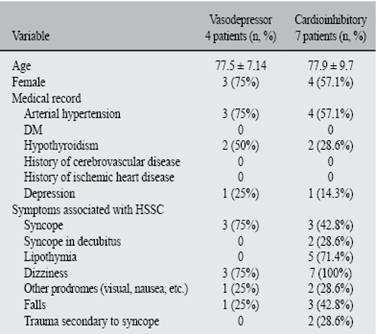
The eleven patients had a mixed variety of CSH, nonetheless, seven patients showed a predominant cardioinhibitory behavior (VASIS 2B) and four the vasodepressor one (VASIS 2ª). Table I shows the main demographic and clinical characteristics of the patients.
Pathophysiology
The pathology of the carotid sinus syndrome/hypersensitivity (CSS/H) is not completely understood, although it has several common points with neurocardiogenic or vasovagal syncope, and that is why it is included within the causes for neurally mediated syncope.1
The main autonomic components are a sympathetic withdrawal that induces vasodepression -hypotension- and a vagal reflex responsible for the cardioinhibitory response. Apparently these phenomena are related with an abnormal function of the baroreceptors and to degenerative changes in the spinal medulla.2,5-7
The chain of events seems to initiate with a drop of the cardiac output induced by bradycardia that is followed by a reduction of the total peripheral vascular resistance, even if the sympathetic withdrawal is immediate to the carotid sinus massage, regardless if it is performed in decubitus or standing up.8
Another group has found that the cerebral «autorregulation» is lost during the CSH-mediated syncope. This implies an incapacity to maintain the brain blood flow in face of a hypotensive challenge and it manifests itself as a higher frequency of syncope spells or falls.9
Clinical presentation
The first descriptions of the carotid sinus hypersensitivity come from Ibn Sina (Avicenna) in the 11th century,10 nonetheless, the correlation between the heart rate or blood pressure changes with the carotid sinus massage was made in 1866. In that year, J.N. Czermack used E.J. Marey’s wrist sphigmographer to demonstrate that the CSM induced bradycardia and hypotension.11
In 1914, a comment about a work from Wenckebach, related the use of tight collars with syncope. The main cases described were clergy men that had syncope when leaning forward or doing other movements with those high tight collars. The syndrome was even named as the «minister’s disease».11
Usually the patients have syncope spells without warning or with minimum previous symptoms. Many times it is related to some action that stimulates the carotid sinus such as turning the head, lift the chin, shave or adjust a tie.12
A significant amount of patients mention falls rather than syncope, as their main symptom, and it is common that the drop attacks are actually a form of CSH.13,14 This is why the clinician must intentionally look for CSH or CSS in those groups of patients.
Diagnosis
The diagnosis of the CSS is clinical and is supported by the reproduction of the signs and symptoms when carotid sinus massage is applied to the patient.
Methodology of the carotid sinus massage
The massage has to be applied in the supine position on both sides of the neck. After that, it has to be repeated in the standing position, with continuous monitoring of the heart rate and blood pressure,1 since up to 30% of the subjects only present the abnormal reflex in the standing position.
Ideally, the CSM should be made in a hospital or in a medical facility capable of solving any possible complication of the test. In this regard, some countries ask for an informed consent form that depicts the possible complications, especially the risk for stroke or the side effects of atropine if it has to be used in the context of the «symptoms method» that will be described further on.
Many syncope units perform the CSM in the same space allocated to the tilt test, since they have a readily available EKG and continuous blood pressure monitoring system.
It is recommended to locate the carotid sinus at the anterior margin of the sternocleidomastoid muscle and the cricoid cartilage (where the carotid pulse is usually felt, under the mandible’s angle). There a firm but gentle pressure has to be applied to avoid any occlusion of the carotid artery. Both sides of the neck have to be stimulated for ten seconds.
Brignole’s group was the first one to clinically use the «symptoms method», described by Thomas in 1969 to evaluate the real contribution of the vasodepressor component of the syndrome in patients with asystole.2,15,16 The method consists in the administration of one milligram or 0,02 mg/kg of body weight of atropine and apply again the CSM. Since the bradycardia component is eliminated, the contribution of the blood pressure fall to the symptoms can be measured more accurately.
Carotid sinus massage has some relative contraindications, as the presence of carotid murmurs, and absolute ones such as ischemic transient attacks, stroke or myocardial infarction the three months prior to the evaluation. According to Sutton, the contraindication is probably more related to the changes in autonomic function induced by those conditions (that can induce false results of the test) than to a real danger of the CSM.2,17
In our series, in the cardioinhibitory group, the average pause duration was 5.1 ± 3.2 seconds (range from 3 to 12 seconds). In four patients the pause was induced while applying massage to the right side of the neck, which is the first stimulated side. In two subjects the pause was induced while massaging the left side and in one patient it was induced while massaging the right side of the neck in a standing position. Only one of the patients with the vasodepressor variety showed it in the standing position.
Management
Carotid sinus hypersensitivity with cardioinhibition
In this form of the syndrome, a double chamber pacemaker seems the most straightforward option. During the first years of the last century’s 80’s decade it was the best treatment option although it had not a generalized acceptation. Apparently, the first cause for this skepticism was the fear to practice a carotid sinus massage as a diagnostic maneuver, and in second place, the recurrence rate.
There is still some controversy about the pacemaker indication,18-21 but nonetheless, it appears in the recent pacing European guidelines as a class I indication with a B level of evidence.22 The recurrence rates are still high and that is related to the co-existence of the vasodepressor and cardioinhibitory components. The physician must discuss this matter with the patient in order to optimize the treatment in every case.
In the eighties of the XXth century, the recurrence rates went from 9% in patients with dual chamber devices to 18% in subjects with ventricular single chamber pacemakers. More recent studies have shown that the recurrences might go up to 20% during a five-year follow-up.2 The work by Solari3 shows that the patients with pure cardioinhibitory CSS have better responses to the pacemaker stimulation, but, as could be expected, the recurrence rate is higher among the other categories.
of the vasodepressor component
As is common among patients with the vasodepressor variant of the neurocardiogenic syncope, the patients with CSS have less treatment options. This is a serious limitation since it is an older population with higher risk of trauma associated to syncope or falls.23
A general recommendation is to increase the ingestion of fluids (approximately two liters per day), and if possible, also increase salt in the diet. Unfortunately, many of these patients also have coexisting arterial hypertension or other co-morbidities that might preclude an increased salt intake or might contra-indicate some of the medications that will be mentioned further on. Other general measures such as exercise have not proven any benefit.24
It is important to reach equilibrium between the drugs that reduce blood pressure and those that increase it, and in many cases, it will be necessary to adjust the anti-hypertensive treatment. Some authors suggest that the blood pressure control might be even more permissive than the one suggested in the guidelines to avoid the hypotension episodes.2
Some studies have used fludrocortisone or midodrine to avoid hypotension among these patients, but the main problem remains hypertension.
A recent study has used droxydopa, a synthetic aminoacid that converts to norepinephrine, as a treatment option in the neurologic orthostatic hypotension syndromes.25 The medication has not been approved specifically for CSS. Its use for short periods has been authorized for multisystem atrophy, Parkinson’s disease and other neurally-mediated orthostatic hypotension syndromes.
In our series, all the patients received general measures (keep an adequate hydration, restrict the use of drugs that were not absolutely necessary, the anti-hypertensive drugs’ dosage was adjusted. mainly diuretics and dehidropyridinic calcium channel blockers) and in two patients we implanted a double chamber pacemaker. These two patients had the longest pauses (Twelve seconds and 5.6 seconds respectively). The other patients with predominant cardioinhibition rejected the device when we made clear to them that it would only avoid the bradycardia-mediated events but not the hypotension-mediated ones.
During the current mean follow-up period (19.5 ± 7.6 months) there have not been any syncope recurrences, but other symptoms such as pre-syncope, dizziness or falls have been present (Among the predominant cardioinhibitory patients it has been 42.8%, three subjects, and in the vasodepressor group it is 50%, two subjects).
Conclusions
The carotid sinus hypersentivity/syndrome is a common form of dys-autonomic reflex in the elderly that is associated with unexplained falls.
The clinical presentation might be confusing, and even if many times the cardinal symptom is syncope, there are cases in which it is not present. The clinician must exert a high suspicion and consider it within the causes for falls or «drop attacks».
Once the diagnosis is confirmed by the carotid sinus massage, the treatment must be directed towards a reduction of its possible consequences. Regarding the patients with the cardioinhibitory variety, pacing is useful although there is a high recurrence rate due to the co-existence of the vasodepressor component.
In the patients with a predominant vasodepressor variety, the treatment aims to keep the blood pressure values within «safe» limits to avoid falls or syncope. The pharmacological options are limited by a lack of experience and by other co-morbidities, the most common, arterial hypertension.
Our series shares the general characteristics described by other authors, but it is worthy to have more national information in order to define if there are local differences.
It is also important to consider that this pathology is an important factor that compromises quality of life among elderly adults and that it can be associated or confounded with other forms of dysautonomic reflexes known in elderly Mexicans.26-28











 nueva página del texto (beta)
nueva página del texto (beta)