Introduction
Evaluation of cardiac structures and function with images and recordings produced by ultrasound is known like echocardiography (E).(1) Currently, E provides essential clinical information;(2) in cardiology it is the second most frequently performed diagnostic procedure.(3) Echocardiographic study is becoming an extension of clinician's physical examination. The appreciation of cardiac anatomy and hemodynamics by E makes the physician's clinical evaluation more relevant to the patient care.(4) Cardiovascular disease is the leading cause of mortality worldwide; in developing countries contributed to 80% of deaths. In both conditions E is an important evaluation tool. Habitually E is mostly restricted to cardiologists, however other specialists frequently refer patients for E evaluation. Common E findings may vary depending on cardiac diseases.(5) It may be different in private clinic or in cardiac center in comparison to general hospital with multiple disciplines. So in this study, the aim was to find out the E profile of findings.
Material and methods
A retrospective and observational study during a three year period from January 1st 2011 to December 31st 2013 was done. Studies were performed by a physician board certified in cardiology and echocardiography. E were done using either a Philips Ecocardiograph model iE33 or a Philips Sonus echocardiograph 5500; a total of 1,468 resting transthoracic echocardiograms were done in the three year period, conventional measurements in M-mode echocardiography, two-dimensional, pulsed, continuous, color and tissue Doppler reports were performed and all were included in the study. Demographic profiles and findings were recorded. A single patient could have had more than one finding. Data analysis was done using SPSS 17, students t test was applied wherever applicable.
Results
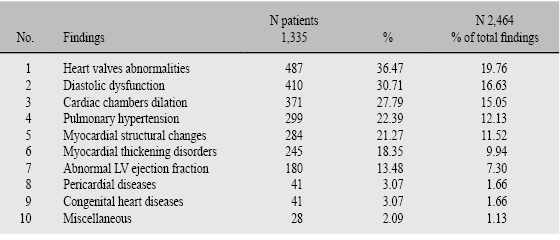
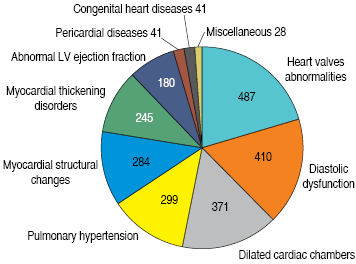
Age range of patients was from 1 day to 94 years with mean (SD) age 51 ± 7.2 years. Of the 1,468 patients, 52.9% were female (n = 776); and 47.1% were males (n = 692) (p = 0.4). Normal echocardiograms were found in 9.05% (n = 133), the remaining 1,335 patients had an average of 1.8 findings/patient. A Total of 2,464 findings were found and classified in ten different categories (Table I and Figure 1). As disclosed in Table I, the most frequent finding was heart valve abnormalities in 36.47% of patients (n = 487), of these, tricuspid regurgitation was the most common in 35.31% of cases (n = 172); in second place mitral valve regurgitation in 24.64% (n = 120), and finally aortic regurgitation in 11.08% (n = 54) (Table II).
Diastolic dysfunction was the second most common findings, in 410 patients (30.71%) (Table I).
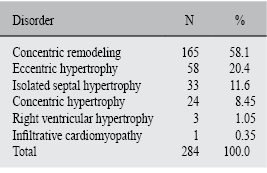
Cardiac chambers dilation were identified in 371 cases (27.79%); left atrial enlargement was seen in 242 cases (65.13%) (Figure 2). Pulmonary hypertension (PH) with 299 cases (22.39%), PH mild or moderate in 249 cases (83.27%); and severe PH 50 cases (16.72%) (Table I). Structural changes of the myocardium were present in 284 patients (21.27%), left ventricle concentric remodeling was the most common structural change found in 165 cases (58.09%) (Table III).
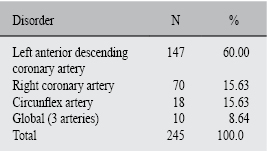
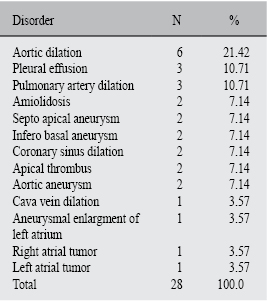
Cardiac muscle thickening disorders were detected in 245 patients (18.35%) and they were classified according to alterations of each coronary artery territory: left anterior descending artery 147 cases (60%), right coronary artery 70 cases (28.57%), circunflex artery 18 cases (7.34%) and global hypokinesis 10 cases (4.08%) (Table IV). Left ventricle ejection fraction (LVEF) was classified as normal when it was ≥ 55% and it was found in 1,288 patients (87.73%); abnormal LVEF was in 180 patients (13.48%), including 45 cases (3.06%) who had severe LVEF < 35% (Table I). Pericardial anomalies, 41 patients (3.07%) of them, pericardial effusion was the most in 37 patients (90.24%) (Table I). Congenital heart diseases were observed in 41 patients (3.07%), atrial septal defect and ventricular septal defect were the most common with 9 cases (21.95%) of each respectively, followed by aortic coarctation and persistent arterial duct with 6 cases of each respectively (14.63%); Fallot tetralogy, Eustachian valve and hypoplastic left heart syndrome were isolated findings (Figure 3). Tenth place corresponded to miscellaneous findings, with a total of 28 cases (2.09%) corresponding to 1.9% of all patients (Table V).
Discussion
Echocardiography is the single most useful test in the diagnosis of heart failure, because structural abnormalities, valvulopathies, systolic and diastolic dysfunction, pulmonar hypertension, or a combination of these traits have to be explored and documented in order to establish the definitive diagnosis in patients with resting or/and exertional symptoms of heart failiure.
It is important to demonstrate an objective evidence of structural or functional abnormalities to explain patient's symptoms of heart failure, because symptoms of heart failure are not specific and more than a third of patients with a clinical diagnosis of heart failure may not actually have it. It is also interesting to note from the SHAPE(6) study that only 3% of more than 7,000 subjects surveyed from nine European countries recognized breathlessness, fatigue, and edema as symptoms of heart failure. Moreover, even when someone presents with typical symptoms of heart failure, a diagnostic test, most frequently an echocardiography examination, is required to establish the underlying etiology for an optimal management strategy.
An important issue is about the four different geometric patrons of the left ventricle which have been described, and these are based on two parameters: a) the presence or absence of increased left ventricular mass (hypertrophy), and b) wall thickness/left ventricular cavity ratio (relative wall thickness). Considering these four different groups of left ventricle geometry are determined: normal geometry, concentric remodeling, concentric hypertrophy and eccentric hypertrophy.(7)
The prognostic value of the different geometric patterns is immense, but, unfortunately, this is not well recognized in daily clinical practice. This prognostic value has been mainly demonstrated in hypertensive patients, but also in other groups at high cardiovascular risk. In hypertensive patients, left ventricular hypertrophy is an index of cardiovascular complications and greater mortality than blood pressure itself.(8) Hypertrophy in hypertensive patients entails a risk of cardiovascular events 20 times greater than when left ventricular geometry is normal.(7)
The risk of mortality or non-fatal complications increases between 2 and 4 times in the presence of left ventricular hypertrophy in patients with coronary disease or noncomplicated myocardial infarction. For example, Liao et al(9) studied 1,089 patients with coronary disease who had undergone cardiac catheterization. Naturally, the factors that were significantly associated with prognosis after stepwise multiple regression analysis were ejection fraction (relative risk [RR] = 2) and the number of vessels with stenosis (RR = 1.6), but the factor that had the greatest impact was left ventricular hypertrophy (RR = 2.4).
In this study structural changes of the myocardium were present in 284 patients (21.27%), and left ventricle concentric remodeling was the most common structural change, followed by eccentric hypertrophy; concentric hypertrophy occupied the third position. Accordingly with the previously mentioned is very important to identify and recognize these morphological alterations.
It has been reported previously the frequency and severity of pulmonary arterial hypertension in a mexican population.(10) In the current report the disease was found in 20.36% of all the echocardiograms performed, which confirms the importance of assessing pulmonary arterial pressure in all cases.
The two-dimensional echoscope of echocardiography was developed by Wild and Reid in 1952. In the past half century, echocardiography has become an established science with a vast literature. Current research appears in peer-reviewed journals. The ability of Doppler echocardiography to provide unique noninvasive information with minimal discomfort or risk without using contrast material or ionizing radiation, coupled with its portability, immediate availability, and repeatability, accounts for its use in virtually all categories of cardiovascular disease. However, two-dimensional Doppler echocardiography is best used after a careful history, physical examination, appropriate electrocardiogram (ECG), and chest radiograph have been obtained so that the appropriate questions can be asked. Echocardiography is a basic tool for diagnosis and follow-up of heart disease. Items of interest in reports can be categorized. In clinical practice, the findings(11),(12) are best interpreted with a view to underlying cardiac physiology and the patient clinical status. Knowing the inherent limitations of echocardiography will help referring physicians to interpret results(13) and to avoid misdiagnoses based on false assumptions about the procedure.14
Conclusions
One imaging test cannot substitute history taking and physical examination. In conjunction with clinical knowledge about the patient and a basic understanding of cardiac physiology, however, echocardiography study is essential for cardiovascular evaluation and follow up. Echocardiography is rapidly evolving. Future development of innovative techniques and consequent changes and improvements in the reports that referring physicians receive from E procedures are sure to come.











 text new page (beta)
text new page (beta)