Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista mexicana de cardiología
versión impresa ISSN 0188-2198
Rev. Mex. Cardiol vol.27 no.1 México ene./mar. 2016
Original Research
Impact of gender on short- and long-term morbidity and mortality after carotid stent angioplasty in a third-level hospital in Mexico
Impacto del género en la morbilidad y la mortalidad a corto y largo plazo después de la angioplastia carotídea en un hospital de tercer nivel en México
Miguel Ángel Salinas-Aragón,* Juan Manuel Palacios-Rodríguez,** Juan Carlos García-Gutiérrez,* Jorge García-Bonilla,* Carlos Alberto Becerra-Laguna,* Horacio Córdova-Correa,* Hugo Alexander López-López*
* Dirección del Departamento de Hemodinamia.
** Departamento de Hemodinamia.
Unidad Médica de Alta Especialidad No. 34, Instituto Mexicano del Seguro Social, Monterrey, N.L.
Correspondence to:
MD. Juan Manuel Palacios-Rodríguez
Minnesota Núm. 300,
Rincón de las Puentes, 66460,
San Nicolás de los Garza,
Mty., N.L., México.
Phone: (52) 80574286 and 87
E-mail: palaciosrj@prodigy.net.mx
Received: 17/09/2015
Accepted: 17/11/2015
ABSTRACT
Objective: To describe gender differences in adult patients undergoing carotid angioplasty and its relation to morbidity and mortality at 30 days and 6 months. Material and methods: An observational study from the WHO database comprehending all patients underwent carotid angioplasty in the Department of Hemodynamics Coronary and Peripheral Artery Intervention, Cardiology Hospital 34, IMSS, Monterrey, was conducted in order to ASSESS the differences between genders and their relationship to primary end points within 30 days after the intervention, which were defined as the presence of death related to the procedure, major cerebrovascular event, or myocardial infarction. Results: 279/341 patients/lesions were included for analysis. Within baseline characteristics, women had significantly higher prevalence of type 2 diabetes mellitus (61.4 versus 45.4%, p = 0.006), prior renal angioplasty (21.9 versus 11.5%, p = 0.015), right carotid condition (65.8 versus 53.7%, p = 0.03), prior stroke (20.2 versus 34.4%, p = 0.007) and higher EuroSCORE (3.13 ± 1.72 versus 2.4 ± 1.26, p < 0.001). The masculine gender was only associated with smoking (69.2 versus 35.1%, p < 0.001). In univariate analysis, the female gender was associated with major fatal and non-fatal stroke (4.4 versus 0.9%, p = 0.031). According to symptomatology and subgroups, we found a significant association between women with asymptomatic Increased risk of major cardiovascular events when compared to asymptomatic diseases (9.5 versus 1.4%, p = 0.004). Conclusions: In our center, women who underwent carotid angioplasty present more comorbidities and higher risk in comparison with the male gender. However, these differences do not impact on most adverse cardiovascular events (MACVE) at 30 days. In the subgroup of asymptomatic patients, the risk of major cardiovascular events is significantly higher in the female gender.
Key words: Carotid angioplasty, carotid stenting, gender, stroke.
Resumen
Objetivo: Describir las diferencias de género en pacientes adultos sometidos a angioplastia carotídea y su relación con la morbimortalidad a 30 días y seis meses. Material y métodos: Estudio observacional de la base de datos que comprende los casos sometidos a angioplastia carotídea en el Departamento de Hemodinámica e Intervención Coronaria Periférica del Hospital de Cardiología No. 34, IMSS, Monterrey. Se analizaron las diferencias entre géneros y su relación con los puntos finales primarios dentro de los 30 días posteriores a la intervención, los cuales fueron definidos como la presencia de muerte relacionada con procedimiento, evento vascular cerebral o infarto agudo de miocardio. Resultados: Se incluyeron 279/341 pacientes/lesiones. Dentro de las características basales se encontró que las mujeres presentaban una mayor prevalencia de diabetes mellitus tipo 2 (61.4 versus 45.4%, p = 0.006), angioplastia renal previa (21.9 versus 11.5%, p = 0.015), afección de carótida derecha (65.8 versus 53.7%, p = 0.03), evento vascular cerebral (EVC) previo (34.4 versus 20.2%, p = 0.007) y EuroSCORE más alto (3.13 ± 1.72 versus 2.4 ± 1.26, p < 0.001). El género masculino sólo se asoció con mayor tabaquismo (69.2 versus 35.1%, p < 0.001). En el análisis univariado, el género femenino se asoció significativamente con EVC (fatal y no fatal) (4.4 versus 0.9%, p = 0.031). Al dividir en subgrupos de acuerdo con la sintomatología, se encontró una fuerte asociación entre las mujeres asintomáticas con más elevado riesgo de eventos cardiovasculares mayores en comparación con el grupo masculino asintomático (9.5 versus 1.4%, p = 0.004). Conclusiones: En nuestro centro, las mujeres sometidas a angioplastia carotídea presentan más comorbilidades y se encuentran en un riesgo mayor en comparación con el género masculino. Sin embargo, estas diferencias no impactan en la incidencia de eventos adversos cardiovasculares mayores (EACVM) a 30 días. En el subgrupo de pacientes asintomáticos el riesgo de eventos cardiovasculares mayores es significativamente más alto en el género femenino.
Palabras clave: Angioplastia carotídea, stent carotídeo, género, cerebral vascular event.
INTRODUCTION
Endovascular treatment of carotid disease is a potentially safer and less invasive therapeutic alternative to carotid endarterectomy (CEA).1 Nevertheless, the value of carotid angioplasty and stenting has been questioned for some specific subgroups of patients,2,3 e.g., according to gender. Previous reports comparing the outcomes of CEA versus have not been angioplasty conclusive in demonstrating gender influence.4 Although the treatment of carotid stenosis seems to achieve greater benefits in men. In symptomatic patients underwent CEA WHO, ECST and NASCET5 within the studies, the benefit was in greater evils especially in those with stenosis > 50%. The necessary number to treat (NNT) in order to prevent an ipsilateral stroke was 9 in men, whilst in women, 36. Similarly, in symptomatic patients included within the NASCET study, to perisurgical significantly higher mortality was found in women when compared to men (2.3 versus 0.8%, p = 0.002).6 In fact, a metaanalysis -including the ACST and ACAS studies- with asymptomatic carotid with disease patients, did not found benefit of CEA in women in terms of 5-years or stroke prevention perisurgical mortality (OR = 0.96; 95% CI: 0.63-1.45); in contrast, a statistically significant risk reduction was found in men (OR = 0.49; 95% CI: 0.36 to 0.66).7 Given thus that ACS has emerged as an option within the treatment of carotid artery disease, it is mandatory to determine the outcomes in different subgroups of patients with such pathology. Some studies have reported that may be greater perisurgical risk in women,8-11 however, this been has not proven in our strata.
The objective of the present study was, therefore, to describe the outcomes according to gender and the statistical relation to 30-days and 6-months morbidity and mortality in patients who underwent CAS.
MATERIAL AND METHODS
We conducted a cohort study, from a database comprising all cases -from February 1998 to December 2013- who underwent CAS in the Hemodynamics and Coronary Intervention Department of Cardiology at Hospital 34, IMSS, Monterrey NL.
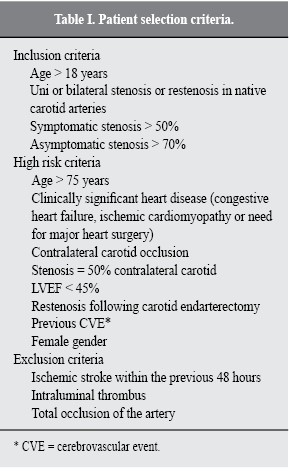
Subjects were considered as eligible to CAS when one of the following high-risk criteria was present: 1) age > 75 years, 2) bilateral disease, 3) contralateral occlusion, 4) injury ostial, 5) multi vessel coronary disease to unstable angina associated, 6) left ventricle ejection fraction (LVEF) < 45%, 7) syntomatic injury with > 50% stenosis and/or > 70% asymptomatic lesion. The patient was considered as "high-risk" when three or more of the aforementioned criteria were present. Selection criteria are shown in table I. All patients signed an informed consent prior to any procedure.
Differences between genders and their relationship to the primary endpoints (defined as death related to procedure, major stroke or acute myocardial infarction) were analyzed within 30 days after the procedure; cardiovascular mortality was analyzed at six months after the intervention procedure. Secondary endpoints were angiographic success, clinical success, presence of TIA, minor stroke, cardiovascular surgery performed within 30 days of the intervention, as well as restenosis diagnosed by Doppler and re-intervention within six months after primary intervention. Angiographic success was defined as an arterial stenosis post minor procedure 30% by quantitative angiography. The clinical success as a stenosis ≤ 30% without major complications (major stroke, death, surgery or acute myocardial infarction) periprocedure. Considered transient ischemic attack to the neurological event with complete recovery within 24 hours of happened. Minor cerebral vascular event is a neurological event that causes mild nerve damage (≤ 3 in the NIH stroke scale), with recovery in less than 30 days. Major cerebral vascular event as a neurological injury that persists for more than 30 days and are severity > 4 according the NIH stroke scale.12
Technique
All patients underwent a clinical neurological evaluation and Doppler study. Vascular Doppler study was performed prior to each procedure by personnel accredited by the Mexican Society of Radiology. Prior to the ACS a charge of clopidogrel 300-600 and 325 mg of aspirin were administered; once the femoral arterial sheath was placed, 70 U/kg of heparin IV were administered. The arterial puncture site was the femoral in the vast majority of cases, local anesthetic type 2% lidocaine was used without epinephrine, no sedation was used in order to maintain a constant neurological condition on the patient; both blood pressure and O2 saturation were monitored during the procedure. A description of our endovascular technique was published previously.13
Statistical analysis
An analysis of the variables of the study and its distribution was performed with measures of central tendency and dispersion. Continuous variables are presented as means with standard deviation (SD) or medium with minimum and maximum according to their distribution. Categorical variables are presented as frequencies and percentages. Continuous variables were assessed using the Kolmogorov-Smirnov test for normality and Levene's for homogeneity of variances. Subsequently, a comparative analysis of each of the variables grouped according to gender and the presence or absence of the primary and secondary endpoints was performed; the latter were also compared in subgroups of symptomatic and asymptomatic patients according to gender. Student's T test or Mann-Whitney U test were performed depending on the distribution of the groups for continuous variables and chi square for categorical variables. A p-value < 0.05 was considered as statistically significant. SPSS 20.0 was used as statistical package.
RESULTS
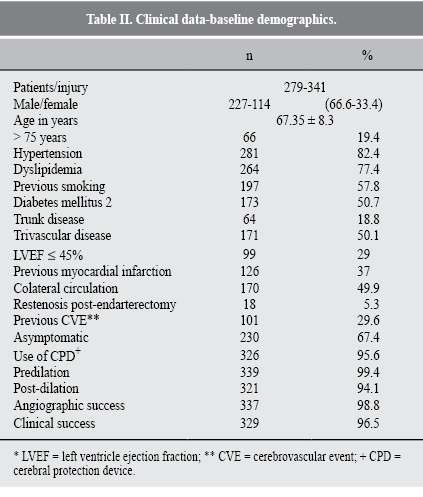
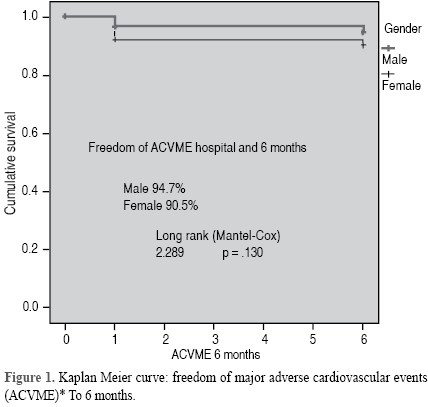
In total, 279 patients/341 injuries were treated. Table II describes the baseline demographic characteristics. A predominance of male gender with 227 (66.6%) injuries treated in this group was found. The average age was 67.35 ± 8.3 years. Systemic arterial hypertension was the most frequent comorbidity in 82.4%, followed by the presence of dyslipidemia in 264 (77.4%) cases. Most injuries were treated in asymptomatic patients with 230 (67.4%). Practically, in all lesions the pre dilation was forced carried it in 339 (99.4%) a cerebral protection device (CPD) was used in 326 (95.6%) of treated lesions. The clinical success was obtained in 329 (96.5%) lesions. At baseline, in relation to gender it was found that women had significantly higher frequency of diabetes mellitus type 2 (DM2) (61.4 versus 45.4%, p = 0.006), greater history of previous renal angioplasty (21.9 versus 11.5% p = 0.015), right carotid disease (65.8 versus 53.7%, p = 0.03), previous stroke (20.2 versus 34.4%, p = 0.007) and higher EuroSCORE (3.13 ± 1.73 versus 2.4 ± 1.27 p < 0.001). Male gender, for its side, was associated with higher frequency of smoking (69.2 versus 35.1%, p < 0.001). Table III summarizes the differences widely according to gender. The result of the univariate analysis of primary and secondary endpoints according to gender at 30 days follow-up are shown in table IV: the female gender was significantly associated with higher stroke (fatal and non-fatal) (4.4 versus 0.9%, p = 0.031) to 30 days. When dividing into subgroups according to symptomatology, a strong association between asymptomatic women with increased risk of major cardiovascular events (stroke, death or myocardial infarction) compared to the asymptomatic male group (9.5 versus 1.4% p = 0.004) was found. A six months follow-up was performed (Table V) in 324 (95%) cases, excluding patients who died within the first 30 days. It was found that within six months after the intervention there were three deaths (1.4%) of cardiovascular origin in the male gender, and none in the female gender, however, no statistical significance in eight cases of the female gender (7.5%) was required to perform coronary artery bypass surgery and in 14 cases (6.5%) of the male gender (p = 0.763). A total of nine lesions with re stenosis by Doppler were documented, however, there was no significant difference in relation to gender. Only three patients required percutaneous carotid re intervention. The global EACVM accumulated by injury at six months was 5.9%. Figure 1 shows the Kaplan Meier curve (KM): the difference between genders of the free evolution of EACVM in the six months following the intervention was evaluated with the curve of Mantel-Cox: 94.7% for men and 90.5% for women, p = 0.13.
DISCUSSION
Worldwide, the cerebral vascular event (EVC) is the second most common cause of death and the third leading cause of disability. 68% of these are ischemic etiology.14 In the United States, it is estimated that the EVC affects approximately 800,000 people per year, 87% of them are of ischemic origin. The latest statistical reports of the American Heart Association indicate that it is the leading cause of disability and cognitive deficits and the fourth leading cause of death. In addition to that it generated in the year 2012 costs of 71.5 billion dollars. The incidence of stroke is 1.5 times higher in men than in women; however, in adults over 75 years this ratio is reversed, with the slightly higher incidence in women. It is estimated that 10-20% of all ischemic stroke are related to significant stenosis of the carotid artery interna.15-17 In Mexico, an observational study found that approximately 25-30% of patients with transient ischemic attack (TIA) may be carriers of significant carotid stenosis18 and RENAMEVASC registration found that 14.7% of ischemic stroke were attributed to atherosclerosis of large arterias.19 For this reason is important in the prevention of the EVC prompt treatment of the significant carotid disease.
As far as it is known, this is the only study in Mexico and Latin America that includes more than 250 patients who underwent ACS. In fact, in our country are few tertiary centers that perform this procedure.
This shown series of patients found that women have significantly higher comorbidities than men like DM2, prior EVC, prior renal angioplasty, as well as a highest EuroSCORE; this partially findings contrast with those found in the NASCET and ASA in patients undergoing CEA studies where the male gender was significantly associated with a higher incidence of prior stroke, previous AMI, and intermittent claudication, although women had a significantly higher incidence of dyslipidemia and hypertension.20 Studies comparing CEA versus ACS only in a sub-analysis of the CREST study were compared by gender baseline characteristics and although in the latter a higher prevalence of hypertension was found in women, no other significant differences in comorbidities in both genders were found, including the length of the injury was significantly lower in women.9
In relation to comparative randomized studies EAC versus ACS, you can see a low representation of women, in the SPACE study only 28% of 1,186 participants were women and 30% of the ICSS study 30% of 1,710 participants.21,22 The rest of the other major randomized trials such as SAPPHIRE, CAVATAS and EVA-3S included less than fewer than 100 women.23 The present study included 114 (33.4%) women, this figure is similar to the percentage of female patients in CREST where one of the pre-specified secondary objectives was to examine gender differences, so that one of the goals of this study was the inclusion of at least 40% of women to give power and validity to detect potential differences of treatment between the sexes, however, in this study 2,502 patients were included, of whom 34.9% were women.
Historically and in several studies has been attributed to the female gender as a risk factor for prognosis in patients undergoing CEA or ACS. In this study no significant differences between genders in relation to EACVM was shown, not so in the greater incidence of stroke fatal and nonfatal where the female gender was significantly associated, this finding differs with two records in the US; one of them which included 54,658 procedures (EAC 94.2% and 5.8% APCS) found that women and men undergoing ACS had equivalent rates of perioperative stroke (2.7 versus 2%, p = 0.2)8 so similar in another database that included 2,074 women and 3,326 men undergoing ACS there were no significant differences in EVC and among both genders.11 This discrepancy could be related to the number of patients studied and other biases inherent in the retrospective nature. In the sub-analysis of the CREST study according to gender the rate of EVC in the ACS group for women was 5.5% and the male gender of 3.3%9 which are slightly higher than those found in this study (4.4% for women and 0.9% for men). In this subanalysis a higher rate of EACVM was found in the group of women undergoing ACS compared to those submitted to EAC which had statistical significance (6.8 versus 3.8%, HR 1.84, 95% CI 1.01-3.37, p = 0.047), in our study EACVM rate at 30 days was 7.9% in women and 3.5% in men HR 0.426 0.160 95% CI-1.14 p = 0.080.
Regarding symptomatic patients, the ECST study found a significant increase in the risk periprocedure in women undergoing EAC compared to men (11.1 versus 6.4% p = 0.002).24 In a subanalysis of the ECST and NASCET of symptomatic patients undergoing CEA studies found that due to the increased surgical risk in women and a lower risk of stroke without surgery, CEA for symptomatic carotid stenosis is less beneficial in women than in men with stenosis between 70-99% and that there is no benefit in women with carotid stenosis between 50-69% compared with medical treatment.25 However, in our case series found that the rate of EACVM to 30 days in symptomatic patients was 7.4% in men and 3.3% in women (p = 0.433) OR 2.32 95% CI (0.268-20.11) indicating a similar benefit for both genders with percutaneous treatment in our population with the presence of symptoms (Table VI). In a metaanalysis that included the SPACE, EVA-3S ICSS studies and safety outcomes were analyzed to 120 days in various subgroups of symptomatic patients, but researchers did not detect a significant interaction among 2,462 men and 971 women (p = 0.24), the relative risk of stroke or death in patients assigned to ACS compared with those assigned to EAC seems to be higher in men (1.68, 95% CI 1.25-2.25) than women (1.22, 0.79-1.89).25 These data contrast with the findings of the ECST and NASCET (IAM not included) where the rate of adverse events (death or stroke) at 30 days was 6.8% in men (67/997) and 8.7% in women (39/453) as well as with the findings of symptomatic patients enrolled in the NASCET (873 women, 2,012 men) and ASA studies (335 women, 813 men) where it was found that the risk of 30-day mortality was higher in women than men (2.3 versus 0.8%, p = 0.002) showing a profit for the male gender.26,27 We can observe that in the population we studied the rate of EACVM to 30 days in symptomatic patients is similar to that found in studies of EAC so the percutaneous treatment could be a less invasive and safer option for patients who have features high surgical risk.
With regard to asymptomatic patients we found a strong association between female gender and increased risk of EACVM compared to males (9.5 versus 1.4% p = 0.004) OR 95% CI 0.132 (0027-0637) or more fatal and non-fatal stroke (4.8 versus 0.0%, p = 0.008) 95% CI 0.354 OR (0297-0422) compared to male, as shown in table VII, these findings show a higher rate of adverse events compared to the study ACAS asymptomatic patients undergoing CEA where the rate of perioperative death and stroke in women was 3.6% (10 of 281) and 1.7% (9 of 544) in men (p = 0.12) 28, as well as CREST study subanalysis where EACVM rate in asymptomatic patients undergoing ACS was 4.2% for females and 3.2% for males and asymptomatic EAC carried EACVM rate was 3.7% in women and 3.5% in men.9 In a metaanalysis including the ACAS and ACST studies of asymptomatic patients do not benefit from the EAC was found in women with respect to the prevention of stroke to five years or perioperative mortality (OR 0.96, 95% CI 0.63-1.45).22 According to these observations it seems to be no benefit of treatment in the subgroup of asymptomatic women with either CAD or ACS in significant carotid disease. In the record of 54,658 patients mentioned previously asymptomatic women who were treated with CAD had a perioperative stroke rate significantly lower than those who underwent ACS (0.9 versus 2.1%, p < 0.001),8 in contrast, in our study a higher rate of EVC fatal and nonfatal (4.8%) was found in the group of asymptomatic women. In the database that included 2,074 women and 3,326 men undergoing ACS group of asymptomatic women had a higher incidence of AMI compared to males (0.96 versus 0.28%, p = 0.01), however, in the symptomatic group of patients no significant differences in stroke, death and/or myocardial between genders was not found, in another database that included 16,576 asymptomatic women undergoing EAC and 1,943 asymptomatic women implanted with ACS a risk of stroke or death was found 3.4 times higher in asymptomatic women in the ACS group compared with the group of CAD.10 These observations support what is described above. The increased risk of stroke or death in women could be attributed to the technical difficulties related to the fact that they have smaller internal carotid arteries than men, on average 40% less,28 in addition women tend to have atherosclerotic disease mainly distributed in the common carotid artery rather than the proximal internal carotid where usually occurs in men, this may cause changes when lesions are crossed during the ACS.29
Limitations of this study include its retrospective nature, the results are from a single center and may not be playable to the general population, monitoring is only six months and the sample size by dividing by gender in symptomatic and asymptomatic is very small. Still, this study shows a panorama under ACS Mexican population and the differences between genders.
CONCLUSION
In our center women undergoing carotid angioplasty have more comorbidities and are at a higher risk compared to the male gender, however, these differences do not impact the whole EACVM (mortality, cerebral vascular event or myocardial infarction) 30 days. In the subgroup of asymptomatic patients the risk of major cardiovascular events is significantly higher in females which could influence the selection and exclusion of patients who will be brought to ACS. In addition, our data suggest that endovascular treatment of carotid disease can be a good alternative to surgical treatment, especially in patients with significant risk factors, however, women with asymptomatic carotid disease conservative medical management could be a most appropriate option.
REFERENCIAS
1. Ricotta JJ, Aburahma A, Ascher E, Eskandari M, Faries P, Lal BK. Updated society for vascular surgery guidelines for management of extracranial carotid disease. J Vasc Surg. 2011; 54: e1-31. [ Links ]
2. Carotid Stenting Trialists' Collaboration, Bonati LH, Dobson J, Algra A, Branchereau A, Chatellier G et al. Short-term outcome after stenting versus endarterectomy for symptomatic carotid stenosis: a preplanned metaanalysis of individual patient data. Lancet. 2010; 376: 1062-1073. [ Links ]
3. Eckstein HH, Ringleb P, Allenberg JR, Berger J, Fraedrich G, Hacke W et al. Results of the stent-protected angioplasty versus carotid endarterectomy (SPACE) study to treat symptomatic stenoses at 2 years: a multinational, prospective, randomized trial. Lancet Neurol. 2008; 7: 893-902. [ Links ]
4. Goldstein LJ, Khan HU, Sambol EB, Kent KC, Faries PL, Vouyouka AG. Carotid artery stenting is safe and associated with comparable outcomes in men and women. J Vasc Surg. 2009; 49: 315-324. [ Links ]
5. Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ; Carotid Endarterectomy Trialists Collaboration. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet. 2004; 363: 915-924. [ Links ]
6. Alamowitch S, Eliasziw M, Barnett HJ et al. The risk and benefit of endarterectomy in women with symptomatic internal carotid artery disease. Stroke. 2005; 36: 27-31. [ Links ]
7. Rothwell PM, Goldstein LB. Carotid endarterectomy for asymptomatic carotid stenosis: asymptomatic carotid surgery trial. Stroke. 2004; 35: 2425-2427. [ Links ]
8. Rockman CB, Garg K, Jacobowitz GR et al. Outcome of carotid artery interventions among female patients, 2004 to 2005. J Vasc Surg. 2011; 53 (6): 1457-1464. [ Links ]
9. Howard VJ, Lutsep HL, Mackey A et al. Influence of sex on outcomes of stenting versus endarterectomy: a subgroup analysis of the carotid revascularization endarterectomy versus stenting trial (CREST). Lancet Neurol. 2011; 10 (6): 530-537. [ Links ]
10. Vouyouka AG, Egorova NN, Sosunov EA et al. Analysis of Florida and New York state hospital discharges suggests that carotid stenting in symptomatic women is associated with significant increase in mortality and perioperative morbidity compared with carotid endarterectomy. J Vasc Surg. 2012; 56 (2): 334-342. [ Links ]
11. Bisdas T, Egorova N, Moskowitz AJ et al. The impact of gender on in-hospital outcomes after carotid endarterectomy or stenting. Eur J Vasc Endovasc Surg. 2012; 44 (3): 244-250. [ Links ]
12. Kasner SE. Clinical interpretation of use of stroke scales. Lancet Neurol. 2006; 5: 603-612. [ Links ]
13. Palacios-Rodríguez JM, Bazzoni-Ruiz A, Torres-Hernández M et al. Stentcarotídeo en pacientes de alto riesgo: seguimiento a largo plazo. Rev Mex Cardiol. 2004; 15: 5-13. [ Links ]
14. Lozano R, Naghavi M, Foreman K et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380: 2095-2128. [ Links ]
15. Go AS, Mozaffarian D, Roger VL et al. Heart disease and stroke statistics 2013 update: a report from the American Heart Association. Circulation. 2013; 127: e6-e245. [ Links ]
16. Ovbiagele B, Goldstein LB, Howard VJ et al. Forecasting the future of stroke in the United States a policy statement from the American Heart Association and American Stroke Association. Stroke. 2013; 44: 2361-2375. [ Links ]
17. Roger VL, Go AS, Lloyd-Jones DM. Heart disease and stroke statistics 2012 update: a report from the American Heart Association. Circulation. 2012; 125: e2-e220. [ Links ]
18. Cantú C, Ruiz JL, Arauz A et al. Prevalencia de estenosis carotídea en pacientes con isquemia cerebral transitoria en México. Rev Mex Neuroci. 2010; 11 (5): 343-348. [ Links ]
19. Cantú C, Ruiz JL, Arauz A et al. Factores de riesgo, causas y pronóstico de los tipos de enfermedad vascular cerebral en México: estudio RENAMEVASC. Rev Mex Neuroci. 2011; 12 (5): 224-234. [ Links ]
20. Young B, Moore WS, Robertson JT, Toole JF, Ernst CB, Cohen SN et al An analysis of perioperative surgical mortality and morbidity in the asymptomatic carotid atherosclerosis study. ACAS Investigators. Asymptomatic Carotid Atherosclerosis Study. Stroke. 1996; 27: 2216-2224 [ Links ]
21. Stingele R, Berger J, Alfke K, Eckstein HH, Fraedrich G, Allenberg J et al. Clinical and angiographic risk factors for stroke and death within 30 days after carotid endarterectomy and stent-protected angioplasty: a subanalysis of the SPACE study. Lancet Neurol. 2008; 7: 216-222. [ Links ]
22. International Carotid Stenting Study investigators, Ederle J, Dobson J, Featherstone RL, Bonati LH, van der Worp HB et al. Carotid artery stenting compared with endarterectomy in patients with symptomatic carotid stenosis (International Carotid Stenting Study): an interim analysis of a randomised controlled trial. Lancet. 2010; 375: 985-997. [ Links ]
23. Howard VJ, Voeks JH, Lutsep HL et al. Does sex matter? Thirty-day stroke and death rates after carotid artery stenting in women versus men: results from the carotid revascularization endarterectomy versus stenting trial (CREST) lead-in phase. Stroke. 2009; 40: 1140-1147. [ Links ]
24. Messé SR, Kasner SE, Mehta Z, Warlow CP, Rothwell PM; European Carotid Surgery Trialists. Effect of body size on operative risk of carotid endarterectomy. J Neurol Neurosurg Psychiatry. 2004; 75: 1759-1761. [ Links ]
25. Bond R, Rerkasem K, Cuffe R, Rothwell PM. A systematic review of the associations between age and sex and the operatives risks of carotid endarterectomy. Cerebrovasc Dis. 2005; 20: 69-77. [ Links ]
26. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991; 325: 445-453. [ Links ]
27. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998; 351: 1379-1387. [ Links ]
28. Rothwell PM, Slattery J, Warlow CP. Clinical and angiographic predictors of stroke and death due to carotid endarterectomy. BMJ. 1997; 315: 1571-1577. [ Links ]
29. Hellings WE, Pasterkamp G, Verhoeven BA, De Kleijn DP, De Vries JP, Seldenrijk KA et al. Gender-associated differences in plaque phenotype of patients undergoing carotid endarterectomy. J Vasc Surg. 2007; 45: 289-296. [ Links ]
Nota
Este artículo puede ser consultado en versión completa en: http://www.medigraphic.com/revmexcardiol














