Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista mexicana de cardiología
Print version ISSN 0188-2198
Rev. Mex. Cardiol vol.27 n.1 México Jan./Mar. 2016
Original Research
Family, obesogenic environment, and cardiometabolic risk in mexican school-age children
Familia, medio ambiente obesogénico, y riesgo cardiometabólico en niños en edad escolar en México
Yolanda Bañuelos-Barrera,* Patricia Bañuelos-Barrera,* Alicia Álvarez-Aguirre,** Marco Vinicio Gómez-Meza,*** Eloína Ruiz-Sánchez*
* School of Nursing, Universidad Juárez del Estado de Durango.
** Universidad de Guanajuato.
*** School of Economy, Universidad Autónoma de Nuevo León.
Correspondence to:
Yolanda Bañuelos Barrera, MD
Av. Cuauhtémoc Núm. 223,
Col. Centro, 34000, Durango, Durango, México.
Phone: +52 618 8171197
E-mail: yobanuelos@gmail.com
Recibido: 02/09/2015
Aceptado: 16/11/2015
ABSTRACT
Introduction: Obesity in children is considered a risk factor for metabolic and cardiovascular disorders at an early age. Objective: To identify the relationship among environmental and family variables on cardiometabolic risk factors (CMRF) in school-age children, and to compare such CMRF by weight status. Material and methods: A cross-sectional design was used. A 228 children and their mothers were randomly selected from public and private elementary schools. Measurements in children included: body fat percentage (BFP), systolic and diastolic blood pressure (SBP, DBP), acanthosis, lipids, glucose, C-reactive protein (CRP), and self-care activities. Mothers were assessed for: BFP, sociodemographic, family history, mothering style. School environment variables were also evaluated. Results: Children and mother's mean ages were 8.5 and 36.8 years, respectively. Mother schooling mean was 12.4 years. Overweight or obese (Ow/OB) children (70.2%) showed higher values in SBP (p = 0. 040), low-density cholesterol (p = 0. 018), triglycerides (p = 0. 003), glucose (p = 0. 022) and CRP (p = 0. 001) and lower in high-density cholesterol (p = 0. 004). Age and child gender, mothering, and mother schooling influenced CMRF [Wilk's Lamda = 0.65, F = 21.71, p < 0.001]. Conclusions: Children with Ow/OB in a obesogenic environment are more likely to develop CMRF. It is necessary to promote the identification and treatment of CMRF at an early age as well as promote healthier family and school environments.
Key words: Obesogenic environment, family, cardiometabolic risk, mexican children.
RESUMEN
Introducción: La presencia de obesidad en niños se considera un factor de riesgo para enfermedades metabólicas y cardiovasculares a temprana edad. Objetivo: Identificar la influencia del ambiente/familia en los factores de riesgo cardiometabólico (FRCM) en escolares y compararlos con su condición de peso. Material y métodos: Diseño transversal explicativo. La muestra estuvo conformada por 228 pares madre-hijo seleccionados aleatoriamente de escuelas primarias públicas y privadas. Mediciones en Niños: porcentaje de grasa corporal (PGC), presión arterial sistólica (PAS) y diastólica (PAD), acantosis, lípidos, glucosa, proteína C reactiva (PCR) y autocuidado; Madres, PGC, datos sociodemográficos, historia familiar, crianza materna; y en escuelas: ambiente escolar. Resultados: Edad promedio: niños 8.5 años y madres 36.8 años. La escolaridad materna promedio fue 12.4 años. Los niños con sobrepeso u obesidad (SP/OB) (70.2%) mostraron valores más altos en la PAS (p = 0.040), colesterol baja densidad (p = 0.018), triglicéridos (p = 0.003), glucosa (p = 0.022) y PCR (p = 0.001) y más bajos en colesterol de alta densidad (p = 0.004). Tanto la edad y género del niño como la escolaridad y estilo de crianza materno influyeron en los FRCM [Lamda de Wilk = 0.65, F = 21.71, p < 0.001] Conclusiones: La presencia de SP/OB fue alta, y en conjunto con un ambiente familiar obesogénico favorecen la prevalencia de FRCM. Es necesario promover un diagnóstico y tratamiento de FRCM a temprana edad, así como favorecer ambientes familiares y escolares más saludables.
Palabras clave: Ambiente obesogénico, familia, riesgo cardiometabólico, niños mexicanos.
INTRODUCTION
Obesity is a multifactorial disease in which, amongst others, family and environmental factors interact in a complex way. Childhood obesity represents a serious problem around the world. According to estimations of the World Health Organization (WHO) by 2010 there were approximately 42 million children with some degree of overweight or obesity.1 In Mexico, the National Health and Nutrition Survey (ENSANUT 2012) estimates that the joint prevalence of overweight and obesity in school-age children reaches a 34.4%.2 Childhood obesity is considered a risk factor for the development of cardiometabolic diseases (e.g., hyperlipidemia, type 2 diabetes, hypertension, vascular damage function, atheroma, coronary artery disease, and inflammation)3-5 which altogether constitute the so-called cardiometabolic risk factors (CMRF).6
Some authors report high prevalence of metabolic and cardiovascular risk factors even among Mexican school-age children (hypertension, hypertriglyceridemia, hyperinsulinemia, hypercholesterolemia, insulin resistance, hyperglycemia, impaired C-reactive protein (CRP), decreased HDL) not showing overweight or obesity.7,8
The scientific literature reports the existence of family and environmental factors associated with the presence of obesity in children. Regarding family factors, it is known that the risk of obesity increases between 1 and 4 times when the mother is overweight or obese, when more than one family member has obesity, when one of them has dyslipidemia, or when the mother presented hyperglycemia during pregnancy.9-11
On the other hand, family behaviors play a decisive role in the development of obesity. Records indicate that the behaviors adopted by parents (e.g. parenting style) as well as their change in attitudes and strategies of parental care, have both positive and negative influences on the management and development of obesity.
Among the positive influences, it has been found that parental attitudes (perceived responsibility) and the monitoring of fats in the diet predict the decrease in BMI of low risk children (i.e. those with no family history of Ow/OB). Similarly, the presence of eating pressure predicts the decrease in BMI for these same children. The involvement of parents in reducing the weight of their children by participating in active play games and by encouraging water consumption, has shown positive effects that are reflected for up to two years after the intervention.12 In contrast, among the negative aspects, it has been found that an excessive concern for the child's weight, a parental perception of the child's weight, and the restriction of fatty foods predict an increase in BMI of high-risk children.12 Similarly, it has been observed that mothers with less sensitive attitudes (not stressed, respectful, non-intrusive) have preschool children that are overweight.13 Also, parents of children with obesity, set fewer limits and strategies to control food intake in obese children than parents with normal weight children.14
Regarding environmental factors, it is recognized that the environment at home and at school directly influence the problem of a children's obesity. Households with more than four members, medium or low income, access to high-calorie diets, three or more hours watching television, and irregular meal times are associated with the presence of overweight or obesity.15-18
Schools with greater availability of fried foods or desserts, as well as the existence of food vending machines in schools and other public places where children attend, irregular meal times, combined with the ads on television and on streets targeting children, are associated with a higher risk for developing obesity.19-21
However, the effect of the home environment, represented by the parental strategies and the school environment (for food and physical activity) on cardiometabolic risk factors has not been sufficiently studied. Likewise, there is a lack of research studies that value self-care activities performed by the child in relation to his diet and management of physical activity, therefore, the purpose of this study was to identify the effect of family and environmental variables on the CMRF among school age children, 7 to 10-years old and disaggregate them by weight values.
MATERIAL AND METHODS
We performed a cross-sectional study including dyads of school-age children attending public and private schools located in Durango, Mexico and their mothers. The sample was composed of 228 mother-child dyads, which were selected from 10 schools by cluster sampling. Considering the lists of school attendance and using the statistical package n-Query 4.0,22 the General Linear Model (GLM) was selected as the statistical test with five independent variables, 0.05 level of significance, 0.90 power, and size effect of 0.09, with a non-response rate of 9%.
Children aged between 7 and 10 years, apparently healthy, with maternal consent for their participation were included in the study. Mothers were literate and consented to their participation. Children with a previous diagnosis of endocrine or metabolic disease according to maternal report were excluded from the study, as well as mothers who were not the primary caregiver.
Measurements
Personal factors: For children we measured age, gender, birth weight, child number and history of receiving breastfeeding, obtained from the mother. They also answered the scale of physical activities on eating habits23 from which we only assessed 11 items related to eating habits (2, 3, 4, 5, 6, 7 and 8) and to physical activity (11, 15, 22 and 27).
Family factors: Mothers reported socio-demographic data, family history of cardiometabolic disease; they also responded to the scale of mothering on diet and children activity24 as part of family obesogenic environment; their BFP was also recorded.
School obesogenic environment: A list consisting of 12 statements was developed to assess nutrition and physical activity at school. Researchers observed and registered children food characteristics, and frequency of consumption, as well as presence and accessibility of sport fields or gyms to do exercise. Children also informed about minutes per day and per week that they engaged in physical activity or sports at school. Indexes were created using the scores, where higher values indicated healthier nutrition and physical activity in the school environment. Lower scores indicated a more obesogenic school environment.
Cardiometabolic Risk (CMRF): Anthropometric, clinical, biochemical and pencil & paper measurements were performed. For the anthropometric measurement, waist circumference was measured using a Seca® fiberglass measuring tape and classified according to age, gender, and ethnic group.25 Height was measured with a metal stadiometer. The weight and body fat percentage of mother and child, who were wearing light clothing and no shoes, were measured with a TANITA® scale, BC-558 Segmental Body Composition Monitor model. The BMI was calculated using the formula weight/height,2 and it was classified by age and gender,26 the children's Body Fat Percentage (BFP) was classified according to age and gender.27
Among clinical assessments, systolic and diastolic blood pressure (SBP, DBP) of children was measured at two points, with 10 and five-minute rests between each measurement. An Omron® pediatric mercury sphygmomanometer was used with bracelets according to the child's arm circumference (9 or 11 cm). The mean values were used to classify them by age, gender and height percentiles.28 The presence of acanthosis nigricans in children, in the neck, armpits, elbows, knuckles and knees was also assessed. The degree to which the area was affected was classified as mild, moderate, and severe, according to color, extent of area affected, and skin texture.29
The biochemical assays on capillary sample of children fasting for 12-hours was saved in capillary tubes of 30 μL to assess lipid profile and glucose and 50 mL for CRP. The samples were analyzed with the Cholestech LDX® which provides results in five minutes for glucose and lipid profile with units in mg/dL, and in seven minutes for CRP with units in mg/L. The corresponding classification was performed with the values obtained.30-32
This study was approved by the Institutional Ethics and Research Committee. All participants, parents or individuals responsible for the children signed an informed consent, and children gave their approval to participate in the study.
Descriptive statistics, parametric and non-parametric statistics (Kolmogorov-Smirnov, Mann Whitney, Spearman correlation, multiple linear regression, and generalized linear models) were performed to analyze the data using the SPSS 18.0 statistical package.
RESULTS
The sample consisted of 228 children and 211 mothers recruited from public (47.4%) and private (52.6%) schools in the city of Durango. The mean age of the children was 8.5 years (SD = 1.0), 96.8% of them reported family history of cardiometabolic disease (38% overweight or obesity, 55.2% high cholesterol, 62.4% diabetes and 62.9% hypertension).
Regarding the anthropometric characteristics, the mean weight and height of children participating in the sample was 33.9 kilos (SD = 9.6) and 1.32 m (SD = .08), with a mean calculated BMI of 18.8 kg/m2. The mean waist circumference was 63 cm (SD = 11.0), while the mean percentage of body fat was 27.8% (SD = 6.7). The weight status of children varied according to the measurement parameter. The waist circumference, the BMI and the body fat percentage, respectively, showed a 27.6%, a 45.3% and a 70.2% overweight level or some degree of obesity or abdominal obesity.
The most prevalent CMRF in school-age children were overweight (31.6%) or obesity (38.6%) according to the BFP which together represented 70.2%, inflammation and risk of coronary heart disease according to the CRP (37%), acanthosis nigricans as an indicator of insulin resistance (32.9%), and alteration of triglycerides (31.6%).
The individual difference of CMRF among children was verified by the presence or absence of overweight or obesity according to the percentage of body fat. The results showed mean differences in some parameters, children with overweight or obesity showed higher values in systolic blood pressure (p = 0.040), LDL (p = 0 .018), TRIG (p = 0.003), GLUC (p = 0.022) and CRP (p = 0.001) and lower in HDL (p = 0.004), as shown in table I
Moreover, the mean age value for mothers was 36.8 years (SD = 5.3) and 12.4 the years of schooling (SD = 2.3), it is noteworthy that the median value for this variable was higher for mothers of private schools (15.2 years ) than of public schools (9.6 years) and showed a significant difference (U = 1366, p = 0.001). On the other hand, the mean number of people per household was 4.6 members (SD = 1.59).
Regarding the anthropometric characteristics of mothers, the mean values obtained were: for weight, 70.3 kilograms (SD = 12.8); for height, 1.57 m (SD = 0.06); for the BMI calculated, 28.2 kg/m2 (SD = 5.1); for waist circumference, 86.8 cm (SD = 12.7), while the mean percentage of body fat was 37.5% (SD = 6.5). The weight status of mothers varied according to the measurement parameter used. According to waist circumference, BMI and body fat percentage, 45.2%, 69.7% and 76.3% of mothers, respectively, showed overweight or some degree of obesity.
Since not all variables showed a normal distribution, a bivariate correlation with Spearman nonparametric test was performed to analyze the relationship between variables. The results showed that maternal education was positively associated with the nutrition of the school environment (p < 0.05) and with the physical activity of the school environment (p < 0.01). Furthermore, an inverse correlation between the age of the child and the physical activity of the school environment (p < 0.05), and between the birth number of the child and the physical activity of the school environment (p < 0.01) was found. The child's management of nutrition and physical activity positively correlated with the nutrition in the school environment (p < 0.05) and the physical activity in the school environment (p < 0.01). No other significant correlations were found.
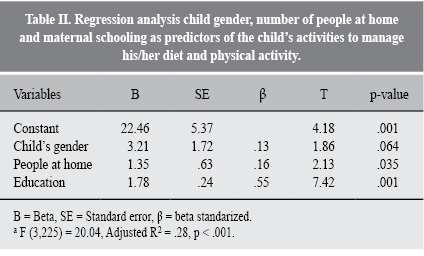
Furthermore, a multiple linear regression model was adjusted to verify the influence of the child's gender, the number of people at home, and the level of maternal education on the child eating and physical activities. The model was significant [F (3,225) = 20.04, p < 0.001] explaining 28.5% of the variance in a child's activities related to the management of nutrition and physical activity (Table II).
A generalized linear model (GLM) with full vector CMRF (systolic and diastolic blood pressure, acanthosis, TC, HDL, LDL, TRIG, glucose, protein C reactive and BFP), was adjusted to identify the influence of family and environmental variables on CMRF. A constant value of p <0.005 was used to identify those variables that correlated most strongly with each other. However, not all CMRF were significant, therefore, the 10-variable vector was modified using the technique of variable removal, until the final model was found where all variables were significant at p <0.005, reducing the vector to three variables. The percentage of body fat was considered the strongest effect since it showed statistical significance in all models.
Subsequently, a second MLG was adjusted, including HDL, LDL, CRP and children's body fat percentage as dependent variables, and, as independent variables, family history, age of child, child's gender, birth weight, adjusted child number, people at home, maternal womb, maternal age, education, occupation, paternal figure, maternal body fat, mothering, child activities for managing his nutritional and physical activities, nutrition and physical activity in the school environment. The analysis adjusted 16 models, of which the final model retained four variables (age and gender of the child, and education and mothering) to explain three CMRF (HDL, LDL and BFP) [Wilks Lamda = .658, F = 21.71, p < 0.001].
DISCUSSION
Among the results of the study, family history of cardiometabolic disease, which included a history of diabetes, elevated total cholesterol, high pressure, and heart disease was found. However, maternal obesity was the more frequent antecedent in the population studied. It is known that children whose mother has some degree of overweight or obesity, have higher risk of alteration these parameters.6,9,10,33,34
The most prevalent CMRF were hypertriglyceridemia, inflammation according to CRP, knees and neck acanthosis, and obesity according to the body fat percentage. Regarding the weight status of children, higher percentages of overweight and obesity were found among children attending public schools. The incidences reported in the literature are similar for both public and private schools,3,7,8,10,20 confirming that the epidemic of obesity can affect all children regardless of their socioeconomic status.
On this same regard, joint prevalence of overweight and obesity was similar (45.3%) to the incidences reported by other authors, which range between 20 to 56.4%, when diagnosed based on the body mass index.2,7,8,20 However, in our study, when classifying children based on body fat percentage, the prevalence exceeds 70%. This results agree with other authors35,36 who report higher prevalence of obesity when compared body fat percentage and BMI, indicating that BFP measurement should be considered when assessing the prevalence of weight status in children, given the latent risk of maintaining such status until adulthood.37
Statistically significant differences were found in overweight or obesity, systolic blood pressure, LDL, TRIG, glucose and CRP, and lower HDL in children with normal weight. Several authors found similar results on the prevalence of CMRF in school-age children, reporting higher levels of glucose, triglycerides, and higher figures in systolic blood pressure of children with higher percentiles in BMI.33,7,38-41 Some authors have noted, the risk factors for cardiovascular disease (inflammation and endothelial dysfunction) contribute to it even in people with normal levels of traditional risk factors for cardiovascular disease such as family history, physical inactivity, obesity, hypertension, hyperlipidemia levels, diabetes mellitus, and coronary artery disease.41,42 The values of such parameters in our sample suggest the urgency of implementing more efficient policies aimed at improving the availability of healthy foods and facilities for physical activity, both at home and in the school. This will increase the likelihood that children consume a balanced diet and exercise, which would result in improving their biochemical parameters.
One of the emerging markers of cardiovascular disease is CRP, which provides information on chronic subclinical systemic inflammation and in this study was considered as a coronary risk factor for its strong and consistent relationship with future cardiovascular events in adolescence or adulthood.42,43 In our study, an important percentage of children showed a moderate and high risk for coronary disease, with higher values especially among those children suffering OW/OB. In contrast, studies report similar prevalences in CRP as well as significant differences by weight status and correlation of CRP with HDL and systolic blood pressure in school age children.7,40,41,43-45 Also it is reported that weight status (overweight or obesity) is the best predictor of CRP elevation,43,46 suggesting that children at early stages in their life start with the development of inflammation, remaining subclinical for years until, in some cases, these symptoms are diagnosed in adolescence or adulthood, or when they present a coronary complication. This asymptomatic process demands the need to include studies in children that identify not only the traditional factors of coronary or metabolic risk, but also the emerging risk factors for coronary heart disease, among which is the CRP.
Regarding the obesogenic environment, the study found that the number of people at home, maternal education, age and gender have an influence in the child's nutrition and physical activity, both at home and at school. In this regard, it has been reported that children from large families (4 or more), as well as being an only child or having a sibling, represent risk factors for overweight or obesity.47,48 On the other side, there is evidence that the level of maternal education influences both the child's weight status and the quality of the food the child eats,48,49 which could explain the reason why although children from private schools had mothers with better schooling, there was no significant difference in the values of overweight and obesity compared to the children in public schools; although there was a significant difference in the levels of TC and HDL. This probably related to the greater consumption of high-calorie diets of low nutritional content given their availability, both at home and at school. It is likely that the acquisition of habits related to nutrition and physical activity by children in the home, justifies their practice in other contexts such as in school, even if those habits are unhealthy.
Finally, the study found that age, gender of the child, education and the family obesogenic environment (maternal parenting style) influenced the CMRF (HDL, LDL and BFP). In this regard, Londoño49 mentions that the levels of the biochemical profile of school-age children tend to increase as they approach the preteen years; specifically the HDL and LDL values, and especially in girls, as occurred in this study. Regarding parenting style, it has been reported that children who grow up in more authoritarian environments have habits for healthier eating, are more active, and have better BMI;50 while a positive association between parenting style (permissive) reported the presence of overweight and obesity in school-age children, coupled with high socioeconomic status.51 In our study, besides finding this relationship with body fat percentage, an association was established with the HDL and LDH, which could be explained by the fact that children with some degree of obesity tend to have alteration in these parameters.38,39
Conclusions
This study found that overweight or obese children had higher parameters in CMRF than underweight or normal weight children. The influence of environmental (school) and family (mothering) variables in developing CMRF was confirmed. The combined prevalence of overweight and obesity based on the body fat percentage (BFP) was higher (70%) than when BMI (45%) is used. BFP was considered the best predictor of CMRF.
Research on the influence of the environment in the formation of habits among school-age children is useful to help understand the complexity of the obesity development process. The results of our study should give healthcare professionals the opportunity of focusing on the promotion of healthy environments that increase the practice of better lifestyles and contribute to maintain or reduce the current prevalence of overweight and obesity, which should delay the onset of chronic diseases in adolescent and young population. Nursing Professionals should reinforce relevant educational aspects in vulnerable populations, particularly starting from early stages that integrate birth and preschool-age children.
REFERENCIAS
1. OMS (2013). Diez datos sobre la obesidad. Ginebra. Organización Mundial de la Salud. 2013. [ Links ]
2. Gutiérrez JP, Rivera-Dommarco J, Shamah-Levy T, Villalpando-Hernández S, Franco A, Cuevas-Nasu L, Romero-Martínez M y cols. Encuesta Nacional de Salud y Nutrición 2012. Resultados Nacionales. Cuernavaca, México: Instituto Nacional de Salud Pública (MX); 2012, p. 200. [ Links ]
3. Balas M, Villanueva A, Tawil S, Schiffman E, Suverza A, Vadillo F, Perichart O. Estudio piloto para la identificación de indicadores antropométricos asociados a marcadores de riesgo de síndrome metabólico en escolares mexicanos. Bol Med Hosp Infant Mex [Internet]. 2008 [cited 2014 May 20];65:100-109. Available from: http://www.coa-nutricion.com/descargas/nutricion/SM_escolares_mexicanos.pdf [ Links ]
4. Barness LA. Obesity in children. Fetal Pediatr Pathol. 2007; 26 (2): 75-85. [ Links ]
5. Walley JA, Blakemore A, Froguel P. Genetics of obesity and the prediction of risk for health. Hum Mol Genet. 2006; 15 (2): R124-130. [ Links ]
6. Drake JA, Reynolds MR. Impact of maternal obesity on offspring obesity and cardiometabolic disease risk. Reproduction. 2010; 140 (3): 387-398. [ Links ]
7. Perichart PO, Balas NM, Rodríguez CA, Muñoz MC, Monge UA, Vadillo OF. Correlates of dietary energy sources with cardiovascular disease risk markers on Mexican school-age children. J Am Diet Assoc. 2010; 110 (2): 253-260. [ Links ]
8. Perichart PO, Balas NM, Schiffman SE, Barbato DA, Vadillo OF. Obesity increases metabolic syndrome risk factors in school-aged children from an urban school on Mexico City. J Am Diet Assoc. 2007; 107 (1): 81-91. [ Links ]
9. De Novaes J, Franceschini C, Priore S. Comparison of the anthropometric and biochemical variables between children and their parents. Arch Latinoam Nutr [Internet]. 2007 [cited 2014 mar 15]; 57 (2): 137-145. Available from: http://www.alanrevista.org/ediciones/2007-2/pdf/anthropometric_and_biochemical_variables.pdf [ Links ]
10. Flores M, Carrión C, Barquera S. Sobrepeso materno y obesidad en escolares mexicanos. Encuesta nacional de nutrición, 1999. Salud Pública Mex [Internet]. 2005 [cited 2014 Abr 5]; 47 (6): 447-450. Available from: http://www.scielo.org.mx/pdf/spm/v47/a09v47n6.pdf [ Links ]
11. Hillier TA, Pedula KL, Schmidt MM, Mullen JA, Charles MA, Pettitt DJ. Childhood obesity and metabolic imprinting: the ongoing effects of maternal hyperglycemia. Diabetes Care. 2007; 30 (9): 2287-2292. [ Links ]
12. Faith MS, Berkowitz RI, Stallings VA, Kerns J, Storey M, Stunkard AJ. Parental feeding attitudes and styles and child body mass index: prospective analysis of a gene-environment interaction. Pediatrics. 2004; 114 (4): e429-436. [ Links ]
13. O'Brien M, Nader PR, Houts RM, Bradley R, Friedman SL, Belsky J, Susman E, NICHD. The NICHD early child care research network. The ecology of childhood overweight: a 12-year longitudinal analysis. Int J Obes (Lond). 2007; 3: 1469-1478. [ Links ]
14. Elder JP, Arredondo EM, Campbell N, Baquero B, Duerksen S, Ayala G et al. Individual, family, and community environmental correlates of obesity in Latino elementary school children. J Sch Health. 2010; 80 (1): 20-30. [ Links ]
15. Al-Saeed WY, Al-Dawood KM, Bukhari IA, Bahnassy A. Prevalence and socioeconomic risk factors of obesity among urban female students in Al-Khobar city, Eastern Saudi Arabia, 2003. Obes Rev. 2007; 8 (2): 93-99. [ Links ]
16. Campbell KJ, Crawford DA, Ball K. Family food environment and dietary behaviors likely to promote fatness in 5-6 year-old children. Int J Obes (Lond). 2006; 30 (8): 1272-1280. [ Links ]
17. Dowda M, Ainsworth BE, Addy CL, Saunders R, Riner W. Environmental influences, physical activity, and weight status in 8- to 16-year-olds. Arch Pediatr Adolesc Med. 2001; 55 (6): 711-717. [ Links ]
18. Hernández B, Gortmaker SL, Colditz GA, Peterson KE, Laird NM, Parra-Cabrera S. Association of obesity with physical activity, television programs and other forms of video viewing among children in Mexico City. Int J Obes Relat Metab Disord. 1999; 23 (8): 845-854. [ Links ]
19. Fox MK, Dodd AH, Wilson A, Gleason PM. Association between school food environment and practices and body mass index of US public school children. J Am Diet Assoc. 2009; 109 (2): S108-117. [ Links ]
20. Torres R, Serrano M, Perez CM, Palacios C. Physical environment, diet quality, and body weight in a group of 12-year-old children from four public school in Puerto Rico. P R Health Sci J [Internet]. 2014 [cited 2014 August 30];33(1):14-21. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4142497/ [ Links ]
21. Mâsse LC, de Niet-Fitzgerald JE, Watts AW, Naylor PJ, Saewyc EM. Associations between the school food environment, student consumption and body mass index of Canadian adolescents. Int J Behav Nutr Phys Act. 2014; 11 (1): 29. [ Links ]
22. Elashoff DJ, Dixon JW, Crede MK, Fothenringham N. N-Query Advisor version 4.0 user's guide. Los Angeles, CA: 2000. [ Links ]
23. Moore JB. Measuring the self-care practice of children and adolescents: instrument development. Matern Child Nurs J [Internet]. 1995 [cited 2013 May 24]; 23 (3): 101-108. Available from: http://www.researchgate.net/publication/15724428_M [ Links ]
24. Larios SE, Ayala GX, Arredondo EM, Baquero B, ELder JP. Development and validation of a scale to measure Latino parenting strategies related to children's obesogenic behaviors. The parenting strategies for eating and activity scale (PEAS). Appetite. 2009; 52 (1): 166-172. [ Links ]
25. Fernández JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr. 2004; 145 (4): 439-444. [ Links ]
26. Center for Disease Control and Prevention [CDC]. Overweight & Obesity. United States; 2009. Atlanta (GA): Centers for Disease Control and Prevention; 2009. [ Links ]
27. Odgen CL, Li Y, Freedman DS, Borrud LG, Flegal KM. Smoothed percentage body fat percentiles for U.S. children and adolescents, 1999-2004. Natl Health Stat Report [Internet]. 2011 [cited 2014 Jan 8];9(43):1-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22164513 [ Links ]
28. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004; 114 (S2); 555-576. [ Links ]
29. Burke JP, Hale DE, Hazuda HP, Stern MP. A quantitative scale of Acanthosis nigricans. Diabetes Care. 1999; 22 (10): 1655-1659. [ Links ]
30. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010; 33 (1): S62-69. [ Links ]
31. Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO 3rd, Criqui M et al; Centers for Disease Control and Prevention; American Heart Association. Markers of inflammation and cardiovascular disease application to clinical and public health practice: a statement for healthcare professionals from the centers for disease control and prevention and the American Heart Association. Circulation. 2003; 107 (3): 499-511. [ Links ]
32. Cook S, Auinger P, Huang TT. Grow curves for cardio-metabolic risk factors in children and adolescents. J Pediatr. 2009; 155 (3): S6.15-26. [ Links ]
33. Burke V. Obesity in childhood and cardiovascular risk. Clin Exp Pharmacol Physiol. 2006; 33 (9): 831-837. [ Links ]
34. Durand EF, Logan C, Carruth A. Association of maternal obesity and childhood obesity: implications for healthcare providers. J Community Health Nurs. 2007; 24 (3): 167-176. [ Links ]
35. Khadgawat R, Marwaha RK, Tandon N, Mehan N, Upadhyay AD, Sastry A, Bhadra K. Percentage body fat in apparently healthy school children from Northen India. Indian Pediatrics [Internet]. 2013 [cited 2015 Oct 19];50(9):859-866. Available from: http://medind.nic.in/ibv/t13/i9/ibvt13i9p859.pdf [ Links ]
36. Pandit D, Chiplonkar S, Khadilkar A, Khadilkar V, Ekbote V. Body fat percentage by dual-energy X-ray absorptiometry corresponding to body mass intex cutoffs for overweight and obesity in Indian children. Clin Med Pediatr [Internet]. 2009 [cited 2015 Oct 20];3:55-61. Available from: http://www.lncbi.nlm.nih.gov/pmc/articles/PMC3676297/ [ Links ]
37. Kaufer HM, Toussaint G. Indicadores antropométricos para evaluar sobrepeso y obesidad en pediatría. Bol Med Hosp Infant Mex [Internet]. 2008 [cited 2013 May 20];65(6):502-518. Available from: http://www.scielo.org.mx/scielo.php?script=arttex&pid=S1665 [ Links ]
38. Dalili S, Rezvani S, Dalili H, Amiri Z, Mohammadi H, Medghalchi A, Novin A. Gholamnezhad H. Cardio-metabolic risk factors in Iranian children: Where we are and the others?. Acta Med Iran [Internet]. 2014 [cited 2015 Aug 13];52(11):831-836. Available from: http://acta.tums.ac.ir/index.php/acta/article/view/4538 [ Links ]
39. Song L, Lu J, Song H, Liu H, Zhang W, Zhao H. Study on the relationship between obesity and lipid metabolism in children and adolescent in yinchuan. Wei Sheng Yan Jiu [Internet]. 2004 [cited 2015 Feb 26];43(5):779-783. Available from: ww.pubfacts.com/fulltext/25438534/Study-on-the-relationship-between-obesity-and-lipid-metabolism-in-children-and-adolescent-in-yinchuan [ Links ]
40. Dayal D, Jain H, Attri SV, Bharti B, Bhalla AK. Relationship of high sensitivity C-reactive protein levels to anthropometric and other metabolic parameters in Indian children with simple overweight and obesity. J Clin Diagn Res. 2014; 8 (8): PC05-8. [ Links ]
41. Arnaiz P, Acevedo M, Barja S, Aglony M, Guzmán B, Cassis B et al. Adiponectin levels, cardiometabolic risk factors and markers of subclinical atherosclerosis in children. Int J Cardiol. 2010; 138 (2): 138-144. [ Links ]
42. Acevedo M, Arnáiz P, Barja S, Bammbs C, Berríos X, Guzmán B y cols. Proteína C reactiva y su relación con adiposidad, factores de riesgo cardiovascular y aterosclerosis subclínica en niños sanos. Rev Esp Cardiol. 2007; 60 (10): 1051-1058. [ Links ]
43. Cook DG, Mendall MA, Whincup PH, Karey IM, Ballam L, Morris JE et al. C-reactive protein concentration in children: relationship to adiposity and other cardiovascular risk factors. Atherosclerosis. 2000; 149 (1): 139-150. [ Links ]
44. Arias GM, Castro AM, Castro UG, Magaña J, Martín L, Sánchez E, Vergara M. Risk factors for cardiovascular diseases present in schoolchildren from Sinaloa, Mexico. The FASEB Journal [Internet]. 2010 [cited 2015 July 23];24:731-735. Available from: http://www.fasebj.org/cgi/content/meeting_abstract/24/1_MeetingAbstracts/731.5 [ Links ]
45. Ridker PM. High-sensitivity C-reactive protein as a predictor of all-cause mortality: implications for research and patient care. Clin Chem. 2008; 54 (2): 234-237. [ Links ]
46. Choi J, Joseph L, Pilote L. Obesity and C-reactive protein in various populations: a systematic review and meta-analysis. Obes Rev. 2013; 14 (3): 232-244. [ Links ]
47. Fernald LC, Neufeld LM. Overweight with concurrent stunting in very young children from rural Mexico: prevalence and associated factors. Eur J Clin Nutr. 2007; 61 (5): 623-632. [ Links ]
48. Díaz MX, Mena BC, Chavarría SP, Rodríguez FA, Valdivia MO. Estado nutricional de escolares según su nivel de actividad física, alimentación y escolaridad de la familia. Rev Cub Salud Pública [Internet]. 2013 [cited 2015 Jun 16];38(4):640-650. Available from: http://www.medigraphic.com/pdfs/revcubsalpub/csp-2013/csp134c.pdf [ Links ]
49. Londoño FA, Mejía LS. Factores de riesgo para malnutrición relacionados con conocimientos y prácticas de alimentación en preescolares de estrato bajo en Calarcá. 2006-2007. Rev Gerenc Polit [Internet]. 2008 [cited 2015 marzo 23];7(15):77-90. Available from: http://www.redalyc.org/pdf/545/54571505.pdf [ Links ]
50. Sleddens EF, Gerards SM, Thijs C, de Vries NK, Kremers SP. General parenting, childhood overweight and obesity-inducing behaviors: a review. Int J Pediatr Obes. 2011; 6 (2-2): e12-27. [ Links ]
51. Topham GL, Page MC, Hubbs TL, Rutledge J, Kennedy T, Shriver L. Maternal depression and socio-economic status moderate the parenting style/child obesity association. Public Health Nutr. 2010; 13 (8): 1237-12-44. [ Links ]
Nota
Este artículo puede ser consultado en versión completa en: http://www.medigraphic.com/revmexcardiol














