Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista mexicana de cardiología
versión impresa ISSN 0188-2198
Rev. Mex. Cardiol vol.26 no.4 México oct./dic. 2015
Case Report and Review
Ruptured sinus of Valsalva aneurysm in adult age; percutaneous closure with occluder device. Report of three successful cases
Ruptura de aneurisma del seno de Valsalva en la edad adulta; cierre percutáneo con dispositivo oclusor. Informe de tres casos exitosos
Lucelli Yáñez-Gutiérrez,* Diana López-Gallegos,* Carmen Emma Cerrud-Sánchez,* Horacio Márquez-González,* Marlenne Berenice García-Pacheco,* Moisés Jiménez-Santos,** Jaime Alfonso Santiago-Hernández,*** Homero Alberto Ramírez-Reyes,*** Carlos Riera-Kinkel****
* Congenital Heart Disease Department.
** Computed Tomography Department.
*** Interventional Cardiology/Catheterization Lab.
**** Cardiothoracic Surgery Division.
Cardiology Hospital, National Medical Center "UMAE Siglo XXI", Mexico City, Mexico.
Correspondence to:
Lucelli Yáñez Gutiérrez, MD
Cuauhtémoc Núm. 330,
Col. Doctores
Del. Cuauhtémoc, 06760,
Mexico City.
Phone: +52 (55) 56-27-69-00, local 22203
E-mail: lucelli.yanez@imss.gob.mx
ABSTRACT
Valsalva sinus aneurysms (VSA) are rare defects, representing 0.09% of all congenital heart diseases. They are more common in male and can be either acquired or congenital. The latter is consequence of an incomplete fusion of the distal bulbar septum that separates the pulmonary artery from the aorta and piece together with the fibrous annulus of the aortic valve. The subsequent thinning of the middle layer of the aorta, leads to progressive dilatation over time. We present three cases of VSA, comprising those of two male patients (aged 19 and 25 years old) and a third pertaining to a woman (aged 32 years old), all of them without cardiovascular risk factors. All patients clinically manifested heart failure and continuous murmur. The two males had sudden chest pain. Echocardiographic diagnosis was confirmed by cardiac catheterization and angiotomography. In all patients, percutaneous closure with an Amplatzer occluder, guided by three-dimensional transesophageal echocardiography, was successfully performed. In the follow-up, all three remain free of heart failure, without signs of significant aortic insufficiency. The etiology of all three cases was congenital. Although traditional surgical repair is associated with less than 2% mortality, since 1994, transcatheter closure of these lesions with different devices had been tested, being the Amplatzer occluder the one with better results because their bigger retention discs. With this technique the associated complications of median sternotomy and cardiopulmonary bypass are avoided; and at the same time a shorter recovery time and hospitalization length of stay are achieved. There are not many cases like these reported in literature.
Key words: Congenital heart disease, Valsalva sinus aneurysms, Amplatzer occlude, three-dimensional transesophageal echocardiography.
RESUMEN
Los aneurismas del seno de Valsalva (ASV) son defectos raros que representan el 0.09% de todas las cardiopatías congénitas. Son más comunes en varones y pueden ser congénitos o adquiridos. Los ASV congénitos ocurren debido a una fusión incompleta del septum bulbar distal, que separa la aorta de la arteria pulmonar y se une al anillo fibroso de la válvula aórtica. El adelgazamiento consecuente de la túnica media de la aorta puede llevar con el tiempo a la dilatación progresiva. Presentamos tres casos de ASV, dos de pacientes masculinos (edades de 19 y 25 años) y un tercero de una mujer de 32 años, todos ellos sin factores de riesgo cardiovascular. Los tres pacientes tuvieron insuficiencia cardiaca y soplo continuo. Los dos hombres, además comenzaron con dolor torácico súbito. El diagnóstico ecocardiográfico fue confirmado mediante cateterismo cardiaco y angiotomografía. Los tres pacientes fueron sometidos exitosamente al cierre de la ruptura aneurismática con el oclusor de Amplatzer, bajo la guía de la ecocardiografía transesofágica tridimensional. En el seguimiento los tres pacientes están libres de insuficiencia cardiaca y sin signos significativos de insuficiencia aórtica. La etiología de los tres casos fue congénita, pero la ruptura se asoció a trauma torácico. La reparación quirúrgica se asocia a menos del 2% de mortalidad. Desde 1994, han sido probados varios dispositivos para cerrar el defecto vía transcatéter, siendo el oclusor de Amplatzer el que obtuvo mejores resultados, por sus discos de retención más grandes. Con esta técnica se evitan las complicaciones de la esternotomía y de la circulación extracorpórea y se logran además tiempos de recuperación y de hospitalización menos prolongados. No hay muchos casos como estos en la literatura.
Palabras clave: Cardiopatías congénitas, aneurismas rotos del seno de Valsalva, oclusor Amplatzer, ecocardiograma transesofágico tridimensional.
INTRODUCTION
According to their relationship to the coronary arteries there are three sinuses of Valsalva at the root of the aorta: the right and left sinuses, giving rise to the right and left coronary arteries and the posterior non-coronary sinus. Valsalva sinus aneurysms (VSA) are thin-walled outpouchings due to destruction or weakness of the middle layer of the aorta at the origin of the sigmoid valves, with discontinuity between this layer and the aortic valve fibrous annulus. They represent < 1% of all congenital heart defects. Most of them involve the right sinus (70%), 28% affect the non-coronary sinus, and just 2% entangle the left sinus.
Without treatment, the natural evolution is a progressive dilatation of the affected tissue, leading in around one third of the patients to the rupture generally into a low pressure right heart chamber. Infrequently, the rupture causes myocardial ischemia when the left VSA is involved, due to compression of the circumflex artery. Clinically, there is a continuous murmur in the left parasternal area and the examination reveals signs of aortic valve insufficiency. We describe 3 cases seen of our department, diagnosed with rupture VSA, who underwent percutaneous closure with occlusion device.
CASE 1
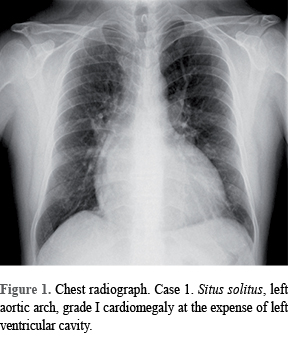
An otherwise 19-year-old healthy male had in his medical records the antecedent of an "innocent heart murmur" in his childhood. One year ago to his admission he began to have progressive dyspnea and lower limbs edema. He was referred to our center with diagnosis of aortic valve disease and ventricular septal defect. X-ray chest film showed mild cardiomegaly (Figure 1) and normal electrocardiogram. The echocardiogram revealed ruptured VSA of 8 mm into the right ventricle and mild aortic regurgitation. It was decided to perform transcatheter closure employing an Amplatzer occluder for interventricular septal defect. The procedure, guided by transesophageal echocardiography was successful without any residual deficit. Twenty four hours later was discharged in good clinical condition. The follow-up has been uneventful.
CASE 2
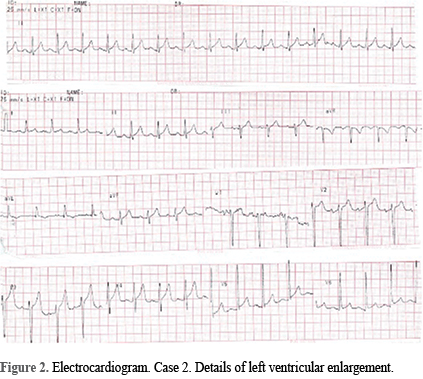
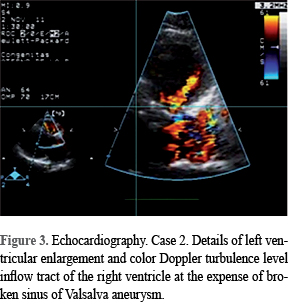
Male, 25 years old. An unruptured aneurysm of sinus of Valsalva was diagnosed in childhood. After physical exertion he experienced sudden oppressive chest pain, progressive dyspnea and palpitations. X-ray chest film showed grade I cardiomegaly, and pulmonary venocapillary hypertension. The electrocardiogram showed left ventricular enlargement (Figure 2). Echocardiogram showed ruptured right VSA of 10 mm diameter towards right ventricle, and aortic valve insufficiency of moderate degree (Figure 3). The pathology was confirmed by angiotomography. Percutaneous approach was also decided, and the procedure was done successfully. Follow-up monitoring has demonstrated that aortic regurgitation has decreased and is of slight degree.
CASE 3
A 32 years-old woman without cardiovascular risk factors and no previous cardiovascular disease, began to have progressive dyspnea, palpitations and lower limbs edema, after chest trauma. A continuous murmur was auscultated in the precordial area. X-ray chest film showed cardiomegaly and cephalization of blood flow, whereas ECG had signs of left ventricular hypertrophy. Echocardiogram showed ruptured right VSA of 10 mm into the right ventricle, with color mosaic and turbulence at this level. Angiotomography confirmed the lesion (Figure 4). Percutaneous closure with Amplatzer septal occluder, guided by three-dimensional transesophageal echocardiography, was carried out, uneventfully. In the follow-up, the patient is in good clinical conditions.

LITERATURE REVIEW
In 1840, the first description of VSA was made by Thurman in a necropsy. In 1955, Oram described the first clinical description. Lillihei, in 1957, performed the first successful surgical intervention. In 1962, Sakakibara and Konno, elaborated the classification which is valid still today. VSA are rare anomalies, representing < 1% of all congenital heart defects. They are more common in Asia and India, and affect more males than females in a 3:1 proportion. The etiology can be congenital, like in our descriptions, or acquired, due to an acute or chronic, degenerative or inflammatory process like syphilis, endocarditis, atherosclerosis, aortic dissection, Marfan syndrome, tuberculosis and fungi, etc.).
VSA can be associated to trunco-conal defects like ventricular septal defects, aortic insufficiency, pulmonary stenosis or subaortic stenosis.1 Mostly, they are unique but occasionally can be multiple. In general, if they are small do not cause symptoms, but when increased size can block or compress other structures.
In general, the symptomatology starts after the aneurysm breaks into a low pressure cardiac chamber, as in our three cases. The rift is usually associated to a strenuous exercise, infection or trauma. Another risk factor for aneurysm rupture is hypertension (not seen in our patients). The rupture can be in a single site or multiple places. In the right sinus take place 70% of the ruptures, while 25% occur in the non-coronary sinus. More uncommon are the ruptures in the left sinus, which acquires a round shape and exhibits early calcification.2
Sakakibara and Konno classification categorizes VSA in four types, the first three involve the right sinus which breaks into the right ventricle, below pulmonary leaflets (type 1), above the supraventricular crest (type 2) or below septal leaflet of the tricuspid (type 3), and type 4 involve non-coronary sinus and it is directed to the right atrium above the tricuspid septal leaflet.3
According to the VSA location, clinical outcomes vary. Those of the right sinus obstruct the outflow tract of the right ventricle and can produce pulmonary valve insufficiency or can obstruct the ostium of the right coronary artery. The aneurysms from the non-coronary sinus are associated to stenosis or tricuspid regurgitation and conduction disorders, while those of the left sinus origin can compress the left coronary artery and calcify. Also, the site towards VSA breaks depends on its location. In order of frequency, the right origin VSA opens to the right ventricle and right atrium, pericardium, pleura and left chambers and very seldom towards the interventricular septum, pulmonary artery or superior vena cava.
The aneurysms from right coronary sinus are associated of 30-50% with septal defects, aortic coarctation, atrial septal defect, tetralogy of Fallot, and patent ductus arteriosus.4,5
Among the main complications of VSA are described aortic insufficiency, coronary artery compromise, diverse arrhythmias, rupture and endocarditis. In our three patients, some degree of aortic valve insufficiency was documented.
The diagnosis is suspected by clinical evidence of acute heart failure, with right failure predominance due to right ventricular overload. Sometimes patients experience chest pain. Some patients shown aortic regurgitation signs but generally in VSA it is described a continuous left parasternal murmur, between the III and IV left intercostal space. In fact, this is the characteristic clinical finding, obliging to a differential diagnosis with other causes of continuous murmur.5 If the anomaly causes right side cardiac overload, X-ray chest can show different grades of cardiomegaly, raised apex and increased pulmonary blood flow. The ECG can be nonspecific.
The diagnosis is confirmed by imaging studies including echocardiography and tomography that in our patients allowed the identification of the affected sinus and the cardiac chamber in which the VSA broke, as well as the measure of the size of the defect, with high correlation with angiographic data. During the closure, transesophageal echocardiogram is a very useful assisting tool permitting the adequate placing of the closure device. Also, it is advisable that after the deployment of the device, an aortography and ECG have to be carried out, in order to reveal possible complications.6,7
As it is estimated that survival after the moment of rupture is less than 1 year, therefore it is mandatory that all patients with ruptured aneurysm should be treated either by surgery or percutaneously.8
Traditionally the repair was surgical, until 1994, when Cullen performed the first percutaneous closure using a Rashkind umbrella device. Later coils and other devices were used as occluders. However, Amplatzer devices (for interventricular or interatrial septal defects) have shown better results a cause of the increased stability of the devices and the size of the retention disks.7 For those reasons we selected the Amplatzer device for our patients.
The percutaneous transcatheter approach has the advantage that avoids the complications of sternotomy and cardiopulmonary bypass. The interventional procedure causes less pain, leaves no scars, and shorter hospital stays and recovery times. For example, our patients were discharged 24-48 hours after the intervention. The percutaneous technique is more relevant due to is used in the cases of lesions cause by a primary surgery, due to the increasing risk in re-interventions.8
It is evident that remain the possibility of a new rupture in the abnormal tissue of the aortic root. However, that eventuality has not happened in none of our patients, after three year of follow-up. The epithelization of the implanted device can render more resistant the surrounding tissue. Inasmuch this technique is relatively new, it is necessary to observe and follow treated patients over the time to document any complication. For now, percutaneous intervention is a feasible and safe intervention for selected cases.9,10
REFERENCIAS
1. Edwards JE, Burchell HB. The pathological anatomy of deficiencies between the aortic root and the heart, including aortic sinus aneurysms. Thorax. 1957; 12: 125-139. [ Links ]
2. Sher RF, Kimbiris D, Segal BL, Iskandrian AS, Bemis CE. Aneurysm of the sinus of Valsalva: its natural history. Postgrad Med. 1979; 65: 191-193. [ Links ]
3. Sakakibara S, Konno S. Congenital aneurysm of the sinus of Valsalva: anatomy and classification. Am Heart J. 1962; 63: 405-424. [ Links ]
4. Feldman D, Roman M. Aneurysm of the sinuses of Valsalva. Cardiology. 2006; 106: 73-81. [ Links ]
5. Moustafa S, Mookadam F, Cooper L et al. Sinus of Valsalva aneurysms -47 years of a single center experience and systematic overview of published reports. Am J Cardiol. 2007; 99: 1159-1164. [ Links ]
6. Smith RL, Irimpen A, Helmchke F et al. Ruptured congenital sinus of Valsalva aneurysm. Echoardiography. 2005; 22: 625-628. [ Links ]
7. Cullen S, Somerville J, Redington A. Transcatheter closure of a ruptured aneurysm of the sinus of Valsalva. Br Heart J. 1994; 71: 479-480. [ Links ]
8. Azakie A, David TE, PEniston CM et al. Ruptured sinus of Valsalva aneurysm: early recurrence and fate of the aortic valve. Ann Thorac Surg. 2000; 70: 1466-1471. [ Links ]
9. Rao PS, Bromberg BI, Jureidini SB et al. Transcatheter occlusion of ruptured sinus of Valsalva aneurysm: innovative use of available technology. Catheter Cardiovasc Interv. 2003; 58: 130-134. [ Links ]
10. Bialkowski J, Zabal C, Szkutnik M et al. Percutaneous interventional closure of large arteriovenous fistulae with the Amplatzer duct occluder. Am J Cardiol. 2005; 96: 127-129. [ Links ]
Nota
Este artículo puede ser consultado en versión completa en: http://www.medigraphic.com/revmexcardiol














