Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista mexicana de cardiología
Print version ISSN 0188-2198
Rev. Mex. Cardiol vol.26 n.4 México Oct./Dec. 2015
Review
Pregnancy in women with congenital heart disease
Embarazo y cardiopatía congénita
Lucelli Yáñez-Gutiérrez,* Carmen Emma Cerrud-Sánchez,* Diana López-Gallegos,* Horacio Márquez-González,* Marlenne Berenice García-Pacheco,* Moisés Jiménez-Santos,** Jaime Alfonso Santiago-Hernández,*** Homero Alberto Ramírez-Reyes,*** Carlos Riera-Kinkel****
* Servicio de Cardiopatías Congénitas.
** Servicio de Tomografía.
*** Servicio de Hemodinamia.
**** División de Cirugía Cardiotorácica.
UMAE Hospital de Cardiología Centro Médico Nacional Siglo XXI.
Correspondence to:
Dra. Lucelli Yáñez Gutiérrez
Cuauhtémoc Núm. 330,
Col. Doctores, Delegación Cuauhtémoc, 06725, México, D.F.
Tel. (55) 56-27-69-00, ext. 22203
E-mail: lucelli.yanez@imss.gob.mx
ABSTRACT
Advances in the diagnosis and treatment of heart disease have enabled patients to reach adulthood thus reproductive age. In this matter, when women with congenital heart disease get pregnant, it is vital that the multidisciplinary health team includes -of course- an obstetrician, but also a cardiologist and a geneticist. Such teamwork will be able to provide a comprehensive care hence increase the chances of reaching term delivery and, moreover, the probability of reducing the rate of complications for both the mother and the fetus. It is therefore important to acknowledge the physiological changes that occur during pregnancy and the possible complications according to the type of heart disease that the mother presents. It is also responsibility of this multidisciplinary group to provide advice and guidance to terminate the pregnancy when the risk is high.
Key words: Pregnancy, congenital heart disease, women, heart disease.
RESUMEN
Los avances en el diagnóstico y tratamiento de las cardiopatías han permitido que los pacientes lleguen a la edad adulta. La mitad son mujeres y llegarán a la edad reproductiva. Es de vital importancia que el equipo médico incluya tanto al obstetra, como al cardiólogo y al genetista. Esta labor de equipo otorga atención integral y de calidad que incrementa las posibilidades de llevar a término un embarazo con un porcentaje bajo de complicaciones tanto para la madre como para el feto. Por tanto, se debe conocer desde los cambios fisiológicos que ocurren durante el embarazo como las posibles complicaciones de acuerdo al tipo de cardiopatía ya sea de reciente diagnóstico como aquéllas reparadas quirúrgicamente o con cardiología intervencionista. También es responsabilidad de este grupo multidisciplinario brindar consejo y orientación para interrumpir el embarazo cuando el riesgo sea alto.
Palabras clave: Embarazo, cardiopatía congénita, mujer, cardiopatía.
INTRODUCTION
Heart disease is the leading cause of maternal death during pregnancy; this includes several cases of congenital heart disease. Due to advances in treatment options (surgery, cardiological intervention, drugs) the natural history of all congenital heart defects has been modified1 thus, currently, 8-9 out of 10 children with congenital heart disease reach adulthood; from these, half are women who reach reproductive age.2 It is therefore important to provide counseling prior to pregnancy, explain the alternatives for contraception and provide optimal care before, during and after pregnancy.1,2
PREGESTATIONAL ASSESSMENT AND CONTRACEPTION
Ideally, preventive and orientative enforces should begin in adolescence and young women of reproductive age, preparing both patients who have been diagnosed with congenital heart disease, and their parents. Communication between the pediatric cardiologist, the gynecologist, the geneticist and psychologists should interact and perform collaborative work in order to provide the necessary support. These sessions should clarify all doubts and include clear aspects about the morbidity and mortality of procedures, the inherent risk of congenital heart disease complications, indicate life expectancy in the case of congenital heart disease, as well as discussing the need for additional surgeries and future disabilities and hospitalizations.1
The issue of contraception should be addressed by the specialist, however, all team members must keep in mind that several alternatives exist, all with a margin of error or undesirable side effects; therefore the case should be individualized in order to choose the safest option for patients. Hormonal treatments have an increased risk of thromboembolic events and, in the case of patients with anticoagulants, it must be remembered that these modify the metabolism of warfarin and lose their effectiveness when using antibiotics or bosentan. The intrauterine device is safe, although it has been reported in some groups to cause risk of bacteremia and infectious endocarditis, in addition to the fact that about 5% of patients may have a vasovagal reaction to manipulating the cervix during insertion; in addition, replacement must take place at least every 5 years. Barrier methods are definitely not first choice because of the high probability of failure. The best options include definitive treatments such as ligation of the fallopian tubes or recently, stent implants.3-6
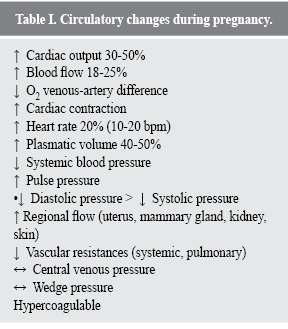
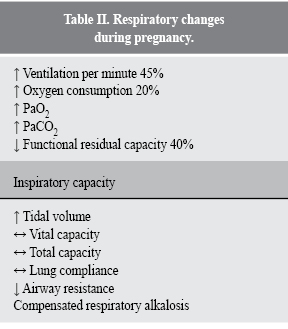
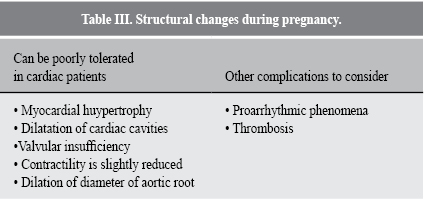
As mentioned before, in order to assess a pregnant patient with congenital heart disease, the physiological changes that occur both at circulatory level (Table I) as well as those to the respiratory system (Table II), structural changes (Table III) and some special considerations at the moment of delivery, such as hemodynamic changes secondary to pain and anxiety, the fact that with each uterine contraction there is a 50% increase in heart rate and cardiac output (approximately 300-400 mL of intravascular volume) and that decompression of the inferior vena cava causes a transfer of blood from the contracted uterus must be considerered.7,8
RISK ASSESSMENT
Based on cohort studies such as the CARPREG study, conducted in 13 Canadian hospitals from 1994-1999, including 546 patients and a total of 599 pregnancies, from which 74% had congenital heart disease and 22% developed heart disease.
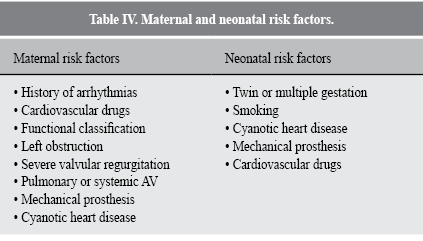
Of all the patients with congenital heart disease, at least 46% had been intervened. Further, predictors of both maternal and fetal events were established. Maternal ones included: history of cardiac events, the presence of arrhythmia, functional classification (FC) of the New York Heart Association (NYHA) above II, the presence of cyanosis, left obstruction data and systemic ventricular dysfunction. Fetal ones included: NYHA functional classification above II, cyanosis in the mother, using heparin or warfarin in the peripartum period, history of maternal smoking, multiple gestation and evidence of left obstruction. Upon analysis of arterial hypertension, it was apparent that nulliparity, lupus erythematosus and a history of coarctation of the aorta are the most important risk factors. Regarding postpartum hemorrhage, only the use of oral anticoagulant (warfarin) or heparin during peripartum are risk factors. Another important fact to consider is that cyanosis in the mother obviously disrupts hemostasis and was a significant factor.
Another published paper specifies that left obstruction will be in either the left mitral valve (area less than ââ2 cm2), aortic (area less than ââ1.5 cm2) or gradient of the left ventricular outflow tract greater than 30 mmHg. Events of arrhythmias, stroke, transient ischemic attack and acute pulmonary edema before pregnancy were other variables to consider and it is noteworthy that age was analyzed as a risk factor, concluding that if you are under 18 or over 35 you are more at risk, as well as taking into account fitness and whether a smoker.9,10
The Zahara study, published in 2010, perhaps the largest published to date, included 1,802 women, 1,302 pregnancies, 336 spontaneous abortions and 58 who chose abortions, aged 27.4 + 2.6 years. This included almost all congenital heart diseases and the most common cardiac complications were arrhythmias and heart failure, whereas the most frequent obstetric complications were arterial hypertension and low birth weight or prematurity.11
From these works, maternal and neonatal risk factors were proposed (Table IV), together with the amended classification from the World Health Organization (WHO) for maternal cardiovascular risk (Table V).9,11,12
SPECIAL TOPICS
Risk of Inheritance
It is a frequently asked question within the assessment of women of reproductive age, due to the fact that overall risk is increased when the mother presents cardiopathy (up 6.7%); however, the fact that the father presents heart disease can also incur risk (2.1%). The type of cardiopathy also modifies such risks: atrioventricular defects in the mother incur a risk of 11.6%, but if it is the father, the risk is 4.3%; aortic stenosis 8 versus 3.8%, respectively; aortic coarctation 6.3 versus 3%, interventricular communication 6 versus 3.6%, pulmonary stenosis 5.3 versus 3.5% and Tetralogy of Fallot 2 versus 1.4%, again, respective to mather/father. Therefore it is imperative that all patients with congenital heart disease are provided with genetic counseling.9,10,13
Cardiovascular drugs
It is well known that congenital cardiopathies will affect embryonic development and organ, thus both angiotensin converting enzyme inhibitors and antagonists of angiotensin II receptors are contraindicated due to the potential renal injury that may result. Likewise, amiodarone is also contraindicated because of the risk of neonatal hypothyroidism, prematurity or neurodevelopmental problems. Spironolactone is not recommended because of genital abnormalities; oral anticoagulants (warfarin and acenocumarine) because of their inherent embryopathy and the risk of bleeding.14,15
However, the following drugs are considered relatively safe: aspirin, diuretics, beta blockers (although there are reports showing that they stunt growth), digoxin, calcium channel blockers, adenosine, procainamide (although pseudo-lupus syndrome must be considered), lidocaine, and flecainide.16
Oral anticoagulation
A controversial aspect concerning embryopathy and the risk of thrombosis, is the use of oral anticoagulants for any therapeutic indication, e.g., prosthesis, history of thrombus, atrial arrhythmias, etc. Guidelines state that the use of oral anticoagulation (OAC) can be prescribed during the second and third trimester to the 36th week; in the first trimester, unfractionated heparin (UFH) or low molecular weight heparin (LMWH) was used, adjusting for APTT> 2 times control or anti Xa 4-6 hours weekly, after administration of 0.8-1.2 U/mL, as appropriate. This change in anticoagulation regimen during pregnancy should be implemented within hospital settings; if labor starts while still in treatment with OAC, caesarean section is indicated. LMWH should be suspended 36 hours before delivery and changed to UFH, which is then suspended 4-6 hours before the planned delivery and restarted after 4-6 hours if there is no complication from hemorrhaging. An echocardiogram is obviously indicated for those women with mechanical prostheses who present sudden dyspnea or an embolic event during the aforementioned regime change between anticoagulant and heparin.12,16
Classification IIA, could consider continuing with OAC during the first trimester if the dose required to maintain therapeutic anticoagulation is < 5 mg/day of warfarin or < 2 mg/day acenocumarine. If doses are > 5 or 2 mg respectively, suspension of OAC between weeks 6 to 12 should be considered and further replaced with UFH or LMWH, among high-risk patients. The use of LMWH is considered within classification III, if the level of antiXa cannot be controlled.16
Severe arrhythmias
In case of severe arrhythmia, antiarrhythmic drugs can be used with some confidence regarding the product. Cases where vagal maneuvers have been used safely have been reported, as well as the introduction of an implantable cardioverter defibrillator or a pacemaker guided by echocardiography in pregnant women with serious arrhythmias or conduction disorders that compromise their lives and that of the product.16-18
Interventionist cardiology
It is known that interventionist procedures must be postponed as far as possible because of the teratogenic risk from radiation (limit is 50 mGy), although common procedures do not involve a very high dose (e.g., both mitral valvuloplasty and coronary angioplasty produce 20mGy). Nevertheless, if it is necessary to undergo a procedure, security measures should be taken in order to protect the abdomen with a lead vest, and should be postponed at least until the second trimester when the uterus is still small and can be perfectly covered and dye should be used; the latter, even if not considered teratogenic, has been reported to be related to neonatal hypothyroidism. E.g., a conventional X-ray causes < 0.01 mGy of fetal exposure and 0.1 mGy for the mother, a CT scan irradiates 0.3 mGy to the fetus and 7 mGy to the mother, coronary angiography yields 1.5 mGy to the fetus and 7 mGy to the mother, and a percutaneous intervention or radiofrequency ablation gives 3 mGy to the fetus and 15 mGy to the mother.12,19,20
Cardiac surgery
Although mortality is reported to be similar to that of the general population, surgery is usually reserved only for cases resistant to medical treatment, due to > 30% fetal loss.19,21
Cardiopulmonary resuscitation
Should this be necessary, it is suggested that resuscitation is performed with the mother discreetly placed on the left lateral decubitus position 15-30o, compressions are made slightly higher than usual and the femoral route should not be used for delivering drugs. A C-section should be urgently scheduled.22
Unresolved lesions
Obstructive lesions of the pulmonary valve with maximum gradient > 64 mmHg must be resolved before pregnancy. Ebstein's anomaly with symptoms of cyanosis and/or heart failure must be resolved prior to pregnancy or strong advice to desist from getting pregnant should be given. Patients with severe enlargement of the right ventricle because of insufficient pulmonary valve should be referred for pulmonary valve replacement with biological prosthesis before pregnancy. All women with bicuspid aorta should have an echocardiogram and other imaging studies in order to assess the ascending aorta and surgical treatment will be proposed if the aorta is > 50 mm. In patients with Fontan surgery, oral anticoagulation will be proposed during pregnancy, as well as for patients with PAH and suspected pulmonary embolism.
Finally, women are contraindicated and advised to terminate the pregnancy if they have PAH, with saturation of < 85%, women with transposition of the great arteries and impairment of right ventricular function, those with an univentricular heart who have undergone the Fontan operation or who have deterioration in the systemic ventricular function or moderate failure of the atrioventricular, or those with cyanosis or protein losing enteropathy.23
CONCLUSIONS
Improvements in medical and surgical treatments have enabled women with congenital heart disease to reach adulthood. Awareness of the need for pregnancies to be programmed and monitored by a multidisciplinary team and necessarily include genetic counseling should be initiated in adolescence. It is the duty of health personnel to promote an echocardiogram for both mother and fetus. We must insist that patients with lower risk of complications are those in FC i-II with resolved heart disease or simple lesions and we must suggest that cyanotic patients or classification III-IV patients should not become pregnant because they present high risk for both the mother and fetus.
REFERENCIAS
1. Wren C, O'Sullivan JJ. Survival with congenial heart disease and need for follow up in adult life. Heart. 2001; 85: 438-443. [ Links ]
2. Uebing A, Steer PJ, Yentis SM et al. Pregnancy and congenital heart disease. BMJ. 2006; 332: 401-406. [ Links ]
3. Thome SA. Pregnancy in heart disease. Heart. 2004; 90: 450-456. [ Links ]
4. Stout K. Pregnancy in women with congenial heart disease: the importance of evaluation and counselling. Heart. 2005; 91: 713-714. [ Links ]
5. Thorne S, MacGregor A, Nelson-Piercy C. Risks of contraception and pregnancy in heart disease. Heart. 2006; 92: 1520-1525. [ Links ]
6. Miner PD. Contraceptive choices for females with congenital heart disease. Prog Pediatr Cardiol. 2004; 19: 15-24. [ Links ]
7. Canobbio MM, Perloff JK, Rapkin AJ. Gynecological health of females with congenital heart disease. Int J Cardiol. 2005; 98: 379-387. [ Links ]
8. Hall ME, George EM, Granger JP. The heart during pregnancy. Rev Esp Cardiol. 2011; 64: 1045-1050. [ Links ]
9. Siu SC, Sermer M, Colman JM et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation. 2001; 104: 515-521. [ Links ]
10. Khairy P, Ouyang DW, Fernandes SM et al. Pregnancy outcomes in women with congenital heart disease. Circulation. 2006; 113: 517-524. [ Links ]
11. Drenthen W, Boersma E, Balci A et al. Predictors of pregnancy compllications in women with congenital heart disease. Eur Heart J. 2010; 31: 2124-2132. [ Links ]
12. Regitz-Zagrosek V, Blomstrom C, Borghi C et al. Guía de práctica clínica de la ESC para el tratamiento de las enfermedades cardiovasculares durante el embarazo. Rev Esp Cardiol. 2012; 65: 171 e1-e44. [ Links ]
13. Siu SC, Sermer M, Harrison DA et al. Risk and predictor for pregnancy-related complications in women with heart disease. Circulation. 1997; 96: 2789-2794. [ Links ]
14. Koren G, Pastuszak A, Ito S. Drugs in pregnancy. N Engl J Med. 1998; 338: 1128-1137. [ Links ]
15. Qasqas S, McPherson C, Frishman W et al. Cardiovascular pharmacotherapeutic considerations during pregnancy and lactation. Cardiol Rev. 2004; 2: 201-221. [ Links ]
16. Tan HL, Lie KL. Treatment of tachyarrhytmias during pregnancy and lactation. Eur Heart J. 2001; 22: 458-464. [ Links ]
17. Leffler S, Johnson DR. Adenosine use in pregnncy: lack of effect on fetal heart rate. Am J Emerg Med. 1992; 10: 548-549. [ Links ]
18. Natale A, Davidson T, Geiger MJ et al. Implantable cardioverter-deibrillators and pregnancy: a safe combination? Circulation. 1997; 96: 2808-2812. [ Links ]
19. Pieper PG, Hoendermis ES, Drijver YN. Cardiac surgery and percutaneous interention in pregnant women with heart disease. Neth Heart J. 2012; 20: 125-128. [ Links ]
20. Guidelines for diagnostic imaging durign pregnancy. ACOG Commiteee Opinion No 299. American College of Obstetricians and gynecologists. Obset Gynecol. 2004; 104: 647-650. [ Links ]
21. Patel A, Asopa S, Tang AT et al. Cardiac surgery during pregnancy. Tex Heart Inst J. 2008; 35: 307-312. [ Links ]
22. 2005 American Heart Association Guidelines for Cardiopumonary resuscitation and Emergency Cardiovascular Care. Circulation. 2005; 112 (Suppl 24): IV1-203. [ Links ]
23. Baumgartner H, Bonhoeffer P, De Groot NM et al. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J. 2010; 3: 2915-2957. [ Links ]
Nota
Este artículo puede ser consultado en versión completa en: http://www.medigraphic.com/revmexcardiol














