Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista mexicana de cardiología
versão impressa ISSN 0188-2198
Rev. Mex. Cardiol vol.26 no.4 México Out./Dez. 2015
Original research
Ventricular interdependence analysis in patients with congenital heart disease with systolic and diastolic dysfunction of the right ventricle
Análisis de la interdependencia ventricular en pacientes con cardiopatía congénita con disfunción sistólica y diastólica del ventrículo derecho
Horacio Márquez-González,* Lucelli Yáñez-Gutiérrez,* Gabriela Borrayo-Sánchez,** Diana López-Gallegos,* Irais C Ortiz-Vázquez,*** Christopher O Camargo-Zetina,* Moisés Jiménez-Santos,**** Jaime Alfonso Santiago-Hernández,***** Homero Alberto Ramírez-Reyes,***** Carlos Riera-Kinkel******
* Servicio de Cardiopatías Congénitas.
** Dirección Médica.
*** Servicio de Gabinetes.
**** Servicio de Tomografía.
***** Servicio de Hemodinamia.
****** División de Cirugía Cardiotorácica.
UMAE Hospital de Cardiología Centro Médico Nacional Siglo XXI.
Correspondence to:
Horacio Márquez-González
UMAE Hospital de Cardiología
Av. Cuauhtémoc Núm. 330,
Col Doctores,
Del. Cuauhtémoc, México, D.F. 06720
Conmutador: 56276900, ext. 2203
E-mail: horacioinvestigacion@hotmail.com
ABSTRACT
Ventricular interdependence (VI) is understood as the response of one ventricle to the changes in pressure and volume in the remaining other. At the time, this behavior in congenital heart disease is not clear, specially in those which affect the right ventricle (RV). Objective: To determine and compare the different types of VI in patients with congenital heart disease (CHD) involving RV with systolic and diastolic dysfunction. Methods: A cross-sectional, comparative study was performed in patients with CHD with volume overload mechanism (atrial septal defects, ventricular septal defects, patent ductus arteriosus and total anomalous pulmonary venous connection) as well as patients with overload pressure mechanism (Tetralogy of Fallot, pulmonary atresia with ventricular septal defect and Ebstein's anomaly). An echocardiographic study was performed on every patient and based on each ventricle ejection fraction and tricuspid and mitral annular plane systolic excursion (TAPSE and MAPSE, respectively) interdependence was classified as: A (Preserved measurements on both ventricles), B (changes in RV with preserved measurements of the LV) and C (changes in both ventricles). Comparison was made by dysfunction type, time of evolution, the Tei index of myocardial performance (IMF), pulmonary artery systolic pressure (PASP) and functional class. Results: Out of 86 patients, we found: type A VI in 58%, type B VI in 26% and type C VI in 16% of patients, type C VI was mostly associated with Ebsteins anomaly. The bigger the interdependence, the longer the time of evolution, weight and Tei's Index. Conclusions: Interdependence occurs in CHD where RV is mainly affected. There is an association between type of interdependence and the mechanism of RV dysfunction (systolic or diastolic).
Key words: Ventricular interdependence (VI), congenital heart disease (CHD), echocardiography.
RESUMEN
La interdependencia ventricular (IV) se entiende como la respuesta de un ventrículo a los cambios en la presión y el volumen restante en el otro. Hasta hoy, este comportamiento en la enfermedad cardíaca congénita no está claro, especialmente en las que afectan al ventrículo derecho (VD). Objetivo: Determinar y comparar los diferentes tipos de IV en pacientes con enfermedad cardiaca congénita (ECC)) que implica al ventrículo derecho con disfunción sistólica y diastólica. Métodos: Estudio transversal y comparativo que se realizó en pacientes de enfermedad coronaria con mecanismo de sobrecarga de volumen (defectos del tabique auricular, defectos septales ventriculares, ductus arterioso permeable y conexión venosa pulmonar anómala total), así como en pacientes con mecanismo de presión de sobrecarga (tetralogía de Fallot, atresia pulmonar con comunicación interventricular y anomalía de Ebstein). Un estudio ecocardiográfico se realizó en todos los pacientes y con base en cada fracción de eyección del ventrículo y en la excursión sistólica tricúspide y mitral del plano anular (TAPSE y MAPSE, respectivamente) La interdependencia se clasificó como: A (conserva las mediciones en ambos ventrículos), B (cambios en el ventrículo derecho con mediciones conservadas en el ventrículo izquierdo) y C (cambios en ambos ventrículos). Se realizó la comparación por tipo de disfunción, tiempo de evolución, el Índice de Tei de rendimiento miocárdico (IMF), presión sistólica de la arteria pulmonar (PSAP) y clase funcional. Resultados: De los 86 pacientes, se encontró: Tipo A IV en el 58%, el tipo B IV en el 26% y el tipo C IV en 16% de los pacientes, Tipo C IV se asocia sobre todo con la anomalía de Ebstein. Cuanto más grande es la interdependencia, mayor será el tiempo de la evolución, peso e Índice de Tei. Conclusiones: La interdependencia ocurre en las enfermedades del corazón, donde el ventrículo derecho se ve afectado principalmente. Existe una asociación entre el tipo de interdependencia y el mecanismo de la disfunción del ventrículo derecho (sistólica o diastólica).
Palabras clave: Interdependencia ventricular (IV), enfermedad cardiaca congénita (ECC), ecocardiografía.
INTRODUCTION
Ventricular interdependence (VI) is understood as the response of one ventricle to the changes of pressure and volume on the other ventricle.1 This relationship is associated with poor outcomes such as death by myocardial infarction.
With acute ischemia ventricle damage favors its identification, whereas in CHD ischemia presents itself in a chronic fashion, distorting myocardial tissue since birth.2
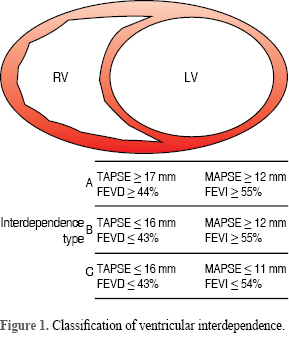
Evaluation of VI mechanism is not standardized, but is mainly obtained by echocardiographic study. Borrayo et al, classified patients with acute myocardial infarction in three types: A, preserved function of both ventricles; B, LV changes with RV preserved and C, changes in both ventricles.3
RV is an embriologic and anatomic site of a considerable number of CHD and volume (diastolic) and pressure (systolic) overload are accountable for right ventricular dysfunction.4,5
As we searched for through medical literature, we found no specific studies on CHD evaluating VI when RV bears the defect causing the disease.
OBJECTIVE
To determine and compare the different types of VI in patients with CHD involving RV with systolic and diastolic dysfunction.
METHODS
A cross-sectional, analytic study was designed at Hospital de Cardiología del Centro Médico Nacional Siglo XXI, CHD clinic, and approved by its local ethics committee, including patients with CHD with the RV as the cause of the disease.
We included patients of both genders, ≥ 4 years of age, without total surgical correction, involving one of these two following lesion mechanisms:
• Diastolic: atrial septal defects (ASD), ventricular septal defects (VSD), patient ductus arteriosus (PDA) and total anomalous pulmonary venous connection (TAPVC).• Systolic: tetrallogy of Fallot (TOF), pulmonary atresia with VSD and Ebstein's anomaly.
Exclusion criteria: left/right coronary infarction history, prior cardiac surgery (patients with systemic to artery pulmonary shunts were not excluded) consisting on cardiopulmonary derivative procedures or therapeutic cardiac/coronary intervention and incomplete data of the patient.
To classify ventricular interdependence, same transthoracic echocardiogram measurements employed by Borrayo et al3 were used, including: ejection fraction (EF) of the left and right ventricle, tricuspid and mitral annular plane systolic excursion (TAPSE and MAPSE, respectively).
Reference values for ejection fraction and TAPSE were taken from echocardiography guidelines for evaluation of both ventricles.6,7 For pediatric patients the lowest reference values were used adjusted to body surface area.8 Figure 1 shows the three variables defining ventricular interdependence.
Age and type of CHD were obtained from surgery/cardiology consensus found on each patient's clinical record.
Tei Index (both left and right), PASP (when Tricuspid insufficiency was present) and RV pressure (when right ventricular outlet obstruction was present) were also obtained.
Echocardiographic study was performed both by cardiologists with fellowship on CHD and pediatric cardiologists with inter and intraobserver kappa index greater than 0.85, according to clinical practice guidelines for echocardiographic windows: parasternal long axis, short axis and apical 4 chamber.
Sample size was not calculated due to the exploratory purpose of this paper, and every patient from January to September 2015 was included in the study. Sampling was carried out accumulating consecutive cases.
STATISTICAL ANALYSIS
Normality tests were performed to determine data distribution. In descriptive statistics, frequencies and percentages were used for qualitative variables, whereas central tendency (mean or median) and dispersion (standard deviation or interquartile ranges) were used for quantitative variables.
Inferential analysis was performed to compare the results between the three categories of ventricular interdependence using linear chi on qualitative variables and mean difference (ANOVA or Kruskal-Wallis) on quantitative variables. The statistical package used was SPSS, No. 20.
RESULTS
We obtained data of 86 patients, with a median age of 15 (8-30) years old, where 56 (65%) were female. The most common CHD found was ASD on 36 (42%) patients. The most common mechanism causing the disease was diastolic on 51 (59%) patients. Frequency of type of interdependence was: A 58%, B 26% and C 16%. Remaining descriptive qualitative and quantitative variables are shown on Tables I and II.
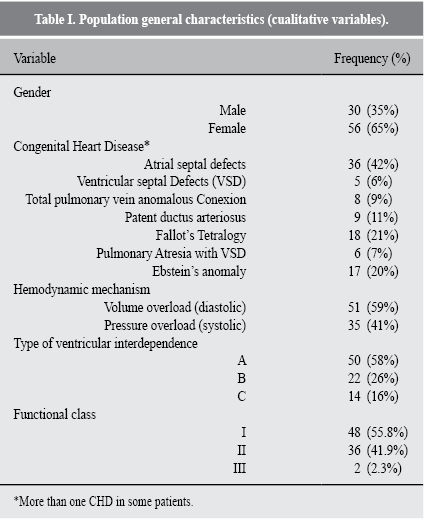
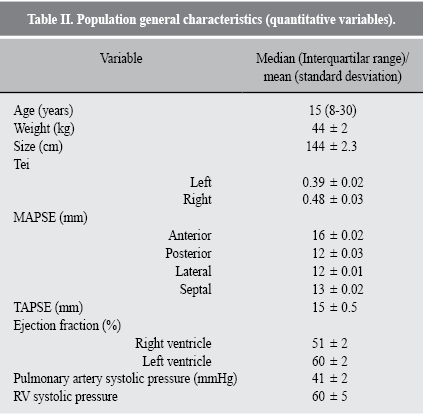
Statistically significant associations were found between CHD and type of ventricular interdependence: pulmonary atresia with VSD and Ebstein's anomaly (Table III). In the same way, we found systolic dysfunction to be related closely to the type (and consequently, degree) of VI. Variables with significant difference according to the type of VI were age/time of evolution, weight and right and left Tei's Index (Table IV).
DISCUSSION
This paper shows that RV systolic dysfunction is statistically associated with a greater degree of VI.
CHD with systolic dysfunction present obstruction of ventricular-arterial continuity with sine-qua-non septal defects, mostly interventricular defects that facilitate right-to-left shunts, causing overload of LV.
Toro R et al compared 28 patients with congenital right-to-left shunts against 28 healthy individuals measuring IMF, strain and strain rate of each ventricle before and after stress test and found differences on LV decreases in function, which were found to significantly correlate (r = -0.69, p â< â0.001) to functional class.9
Interventricular separation of the septum is relevant for VI development, since its displacement diminishes contralateral area and causes pressure overload.10 It is important to mention that we found, when analyzed separately, that pulmonary atresia has a greater association with VI type A. This could be a false association because of the small simple size, although RV outflow tract obstruction conditions a greater right-to-left shunt to the left ventricle, which, unlike RV, will develop volume overload.11,12
When analyzed separately we also found Ebstein's anomaly mostly associates with type C VI; finding integrity of interventricular septum in every case, but a greater RV systolic overload without a chance to release any pressure. This supports previous animal and patient studies with pulmonary embolism where the increase in pulmonary resistance without shunt conditioned a grater degree of left ventricle deformation.13
It is also important to note that CHD with volume overload caused by left-to-right shunt will not significantly associate to severity of VI, which can be explained by the fact that echocardiography mainly evaluates systolic function of both ventricles and because the affecting mechanism which conditions impairment of the ejection fraction of the ventricle is related directly with volume, and its measurement was not included in this study. In this regard, an experimental study on pigs has proven that filling of the RV is not a passive movement, but more like a suction bomb, that requires energy to fill the ventricular cavity by a strong elastic recoil, and it is in this very recoil when the IV septum moves and equals LV pressure. On cases of volume overload, there is a greater energy consumption and an increase on LV pressure. If there is an increase of volume, there will be more energy consumption and an increase that will prevent the LV from filling.14
We found that the median of time of evolution was greater on each type of VI (C being greater than B and B being greater than A), so we can conclude that the longer the time of evolution of the disease, the greater the degree of VI, which has already been analyzed and significant correlation between time and decay of functional class has been found.
Difference found between right and left Tei and type of interdependence can be explained with EF variable, used as a diagnostic variable.
Although this study was not designed to predict outcome, a greater mortality risk has been found with left heart failure on patients with a RV fractional area less than 35% and confirmed LVEF (HR: 2.4, CI-95%: 1.6-2.6, p < 0.0001).15
This is an exploratory study and the associations we found require a more complex methodological analysis that could find the prognostic value of VI on CHD.
Methodological weaknesses of this study include that definition and classification of interdependence were made for patients with myocardial infarction. It is necessary to incorporate other echocardiographic variables that help deduce accurately RV systolic and diastolic function.
It is also necessary to adjust age and surgical treatment, which are relevant on patients with CHD, therefore a bigger sample size to homogenize groups on each CHD.
CONCLUSION
VI is a mechanism occurring on CHD when RV is mainly affected. There is an association between the type and degree and the mechanism of dysfunction of the RV (systolic or diastolic). There is the need to complete the analysis with a greater sample size and to incorporate measurements to the echocardiographic study.
REFERENCIAS
1. Elzinga G, Van Grondelle R, Westerhof N, Bos GC. Ventricular interference. Am J Physiol. 1974; 226: 941-947. [ Links ]
2. Cho YK, Ma JS. Right ventricular failure in congenital heart disease. Korean J Pediatr. 2013; 56 (3): 101-106. [ Links ]
3. Borrayo-Sánchez G, Contreras-Rodriguez A, Careaga-Reyna G, Antezana-Castro J, Argüero-Sánchez R. Interdependencia ventricular sistólica con el desplazamiento del plano auriculoventricular en pacientes con primer infarto del miocardio. Evaluación y propuesta de clasificación. Cir Ciruj. 2004; 72: 465-470. [ Links ]
4. Moorman A, Webb S, Brown NA, Lamers W, Anderson RH. Development of the Heart: 1) formation of the cardiac chambers and arterial trunks. Heart. 2003; 89: 806-814. [ Links ]
5. Greyson CR. Pathophysiology of right ventricular failure. Crit Care Med. 2008; 36: S57-S65. [ Links ]
6. Rudski L, Lai WW, Afilalo J, Hua L, Handschumacher M, Chandresekaran K et al. Guidelines for echocardiographic assessment of the right heart in adults: a report from the ameriacan society of Echochardiography. J Am Soc Echocardiogr. 2010; 23: 685-713. [ Links ]
7. Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009; 22 (2): 107-133. [ Links ]
8. Chubb H, Simpson JM. The use of Z-scores in paediatric cardiology. Am Pediatr Cardiol. 2012; 21: 179-184. [ Links ]
9. Toro R, Cabeza-Letrán ML, Quezada M, Rodriguez-Puras MJ, Mangas A. Impaired right and left ventricular mechanics in adults with pulmonary hypertension and congenital shunts. J Cardiovasc Med (Hagerstown). 2014; Jul 29. [Epub ahead of print] [ Links ].
10. Guazzi MD. Ventricular interdependence. Differences between normal and hypertrophic hearts. G Ital Cardiol (Rome). 2006; 7: 85-90. [ Links ]
11. Starling MR, Walsh RA, Dell'Italia LJ, Mancini GB, Lasher JC, Lancaster JL. The relationship of various masures of end-systole to left ventricular maximum time-varyng eastance in man. Circulation. 1987; 76: 32-43. [ Links ]
12. Dell'Italia LJ, Walsh RA. Application of a time varying elastance model to right ventircular performance in man. Cardiovasc Res. 1988; 22: 864-874. [ Links ]
13. Buckberg GD, Hoffman JI, Coghlan HC, Nanda NC. Ventricular structure-function relations in health and disease: Part I. The normal heart. Eur J Cardiothorac Surg. 2015; 47: 587-601. [ Links ]
14. Goldman E. Age-dependent cardiopulmonary interaction during airway obstruction: a simulation model. Am J Physiol Heart Circ Physiol. 2010; 299: H1610-H1614. [ Links ]
15. Melenovsky V, Hwang SJ, Lin G, Redfield MM, Borlaug BA. Right heart dysfunction in heart failure with preserved ejection fraction. Eur Heart J. 2014; 35: 3452-3462. [ Links ]
Nota
Este artículo puede ser consultado en versión completa en: http://www.medigraphic.com/revmexcardiol














