Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista mexicana de cardiología
Print version ISSN 0188-2198
Rev. Mex. Cardiol vol.26 n.4 México Oct./Dec. 2015
Original Research
Late complications of aortic coarctation treatment: a mexican cohort study with more than 10-year follow-up
Complicaciones tardías de tratamiento de coartación aórtica: estudio mexicano de cohorte con más de 10 años de seguimiento
Horacio Márquez-González,* Salime De León-Mena,* Lucelli Yáñez-Gutiérrez,* Diana López-Gallegos,* Christopher O Camargo-Zetina,* Irais C Ortiz-Vázquez,** Moisés Jiménez-Santos,***Jaime Alfonso Santiago-Hernández,**** Homero Alberto Ramírez-Reyes,**** Carlos Riera-Kinkel*****
* Servicio de Cardiopatías Congénitas.
** Servicio Gabinetes.
*** Servicio de Tomografía.
**** Servicio de Hemodinamia.
***** División de Cirugía Cardiotorácica.
UMAE Hospital de Cardiología Centro Médico Nacional Siglo XXI.
Correspondence to:
Salime De León-Mena
UMAE Hospital de Cardiología.
Av. Cuauhtémoc Núm. 330,
Col. Doctores, 06720,
Del. Cuauhtémoc, México, D.F.
Conmutador: 56276900, ext. 22203
E-mail: salimed@gmail.com
ABSTRACT
Aortic coarctation's (CoA) prevalence is 0.2 in every 1000 live births. Therapeutic options include surgery and, for the last 20 years, interventional cardiology. Objective: To determine the complications of CoA and examine their association with the type of treatment recieved. Methods: Patients that underwent CoA treatment and had follow-up in our center were included. They were included according to treatment in 3 groups: balloon aortoplasty (group 1), stent aortoplasty (group 2) and open surgery (group 3). Patients who suffered from interrupted aortic arch and those who received treatment in other hospitals or presented complications detected in other hospitals were excluded. Data analysis: Descriptive statistics with central mean tendency and dispersion according to distribution, inferential statistics, X-square, ANOVA/Kruskal-Wallis and Kaplan Meier analysis of survival. Results: n =166, age = 18 (range 13-25), 118 male (71%), 48 in group 1, 57 in group 2 and 61 in group 3. The mean follow-up was 15 years. From the analyzed complications, those with statistical significance were: persistent systemic arterial hypertension (group 1, 15%; group 2, 34%; group 3, 41%, p < 0.001) and re-intervention (group 1, 58%; group 2, 11%; group 3, 36%), p = 0.03. Conclusions: The balloon aortoplasty presents greater percentage of reoperation; and aortoplasty stent has fewer complications, but these are manifested in less time.
Key words: Aorctic coarctation, congenital heart disease, interventional cardiology, stent aortoplasty, complications.
RESUMEN
La prevalencia de Coartación Aórtica (CoA) es de 0.2 por cada 1000 nacidos vivos. Las opciones terapéuticas incluyen cirugía y en los últimos 20 años cardiología intervencionista. Objetivo: determinar las complicaciones de CoA y determinar la asociación con el tipo de tratamiento recibido. Material y métodos: Se incluyeron todos los pacientes con CoA atendidos en nuestra unidad y con seguimiento. Se incluyeron 3 grupos de acuerdo al tratamiento: Grupo 1, aortoplastía con balón, Grupo 2, aortoplastía con Stent y Grupo 3, cirugía. Se excluyeron pacientes con interrupción de arco aórtico o los que habían sido atendidos en otros hospital pero que las complicaciones se registraron en nuestra unidad. Análisis estadístico, se usó estadística descriptiva con medidas de tendencia central y dispersión de acuerdo a la distribución, estadística inferencial con X-cuadrada, ANOVA y Kruskal-Wallis, Kaplan Meier para sobrevida. Resultados: n =166, edad = 18 (rango 13-25), 118 hombres (71%), 48 en grupo 1, 57 en grupo 2, 61 en grupo 3. Seguimiento por 15 años. Al analizar las complicaciones las que tienen significancia estadística fueron: hipertensión arterial persistente (grupo 1, 15%; grupo2, 34%; grupo 3, 41%, p<0.001) y reintervención (grupo 1, 58%; grupo 2, 11%; grupo 3, 36%), p = 0.03. Conclusiones: La aortoplastía con balón tien mayor porcentaje de reintervención y la aortoplastía con stent tiene menor porcentaje de complicaciones, pero estas se manifiestan en un lapso menor de tiempo.
Palabras clave: Coartación aórtica, enfermedades cardiacas congénitas, cirugía, intervención vascular percutánea, complicaciones.
INTRODUCTION
Aortic coarctation (CoA) represents up to 5-7% of all congenital cardiopathies, with a prevalence of 0.2 per 1000 live births and a male-female ratio of 2-1.1
CoA is an abnormal thickening in the medial layer and intimal hyperplasia of the aorta. It usually affects the posterior wall, adjacent to the beginning of the subclavian artery, mainly the distal aortic arch and the emergence of the descending aorta.2 It is accompanied by other cardiac anomalies like bicuspid aortic valve, patent ductus arteriosus or ventricular septal defects and is one of the heart defects usually found in genetic syndromes such as Turner syndrome.3
Untreated CoA decreases quality of life and life expectancy, and in spite of treatment, secondary complications may arise, so the need for continuous monitoring for diseases such as arterial hypertension, premature coronary artery disease or stroke is warranted.4
Corrective treatment must be invasive, and there are two possible approaches: catheterization (balloon or stent aortoplasty); and open surgery (coarctation resection with end-to-end anastomosis, arch dilatation and placing of extra-anatomic bypass).5
Which intervention is used depends on the age of the patient, CoA's anatomy and the presence of coexisting alterations. Cardiologist and pediatric cardiologist are obliged to provide appropriate follow-up in patients in order to timely detect complications.
OBJECTIVE
To compare the frequency of complications in patients CoA treated balloon aortoplasty, stent aortoplasty and open surgery.
METHODS
After obtaining approval from the local ethics committee, we performed a prospective, ambispective study, from CoA patients who had been treated with balloon aortoplasty, stent aortoplasty and open surgery in the congenital heart disease clinic of the Centro Médico Nacional Siglo XXI general hospital in Mexico City.
Patients of both sexes over four years old, that underwent balloon aortoplasty, stent aortoplasty and open surgery and attended all programmed follow-up visits in our hospital were enroled. We excluded subjects who had complications that were detected in other hospitals, or underwent surgical procedures in other hospitals, as well as patients who had other complex heart diseases, like interruption or hypoplasia of the aortic arch, or that were treated in other services and subjects with unsuccessful surgical interventions.
The inclusion of patients was obtained from databases of our department. According the type of interventionist treatment. Three groups were formed: group 1, balloon aortoplasty; group 2, stent aortoplasty; and group 3, open surgery.
In those patients that require re-interventionism (surgical or catheterization) through follow-up, were grouped as a dichotomous outcome variable named: catheterization re-intervention or surgical re-intervention.
The outcome variables were defined as follows:
• Re-coarctation: after successful procedure, evidence of maximum gradient in the re-estenosis site over 20 mmHg.6• Systemic arterial hypertension: blood pressure values over 140/90 mmHg in more than three isolated times in patients with history of normotensive values or patients that need reset antihypertensive drugs after withdrawal.
• Stroke: ischemic or hemorrhagic lesions by skull CT scan and neurology clinical examination.
• "Associated injury" was considered by the high prevalence of bicuspid aorta in this type of heart disease and aortic injury it was divided into:
- Aortic valve insufficiency: moderate and severe degree were included. by two methods, echocardiography (contract vein, diameter of the regurgitant orifice area, M-mode deceleration time and pressure half-time) or catheterization (Seller's classification).- Aortic valve stenosis: were considered as present any degree of manifestation in the absence of diagnosis of aortic regurgitation in the immediate post operative. For the diagnosis was performed echocardiography and catheterization.
- Double aortic lesion: was considered as present to any patient who in the same valve was demonstrated the two lesions described above, in the absence of previous injuries.
- Aortic dissection: diagnosticated by contrast CT scan trough aorta from the root to the descendant segment.
- Endocarditis: were used international guidelines for infectious endocarditis of the infectious Diseases Society of America (IDSA).7
Another outcomes considered were the death and the presence of two or more coexisting complications. The minimal follow-up in the patients was 5 years and maximum of 20.
Patients who received treatment in other hospitals or presented complications in other hospitals were considered losses.
Data analysis: Descriptive statistics, measures of central tendency and dispersion according to distribution was evaluated. Incidence density for each of the outcomes was calculated. Inferential statistics, X-squared, ANOVA was calculated and was performed Kaplan Meier bivariate survival analysis in the outcomes with statistical significance.
RESULTS
166 subjects were included, with a mean age of 18 years (13-25), of which 118 were male (71%, male to female ratio 2.45:1). 48 patients had undergone balloon aotoplasty (27%), 57 stent aortoplasty (34%) and 61 open surgery (37%). The last group included different surgical techniques, in order of frequency: coartectomy and termino-terminal anastomosis (85%), Dacron patch (11%) and extracardiac tube (3%). The incidence density is presented in image 1, the rest of the descriptive variables is presented in table I.
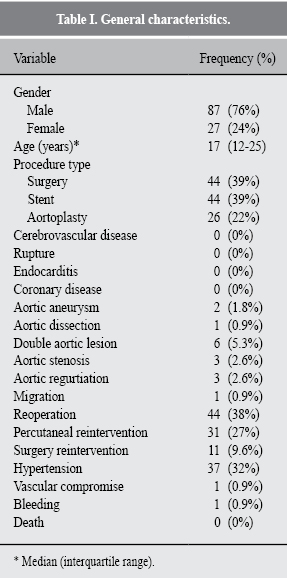
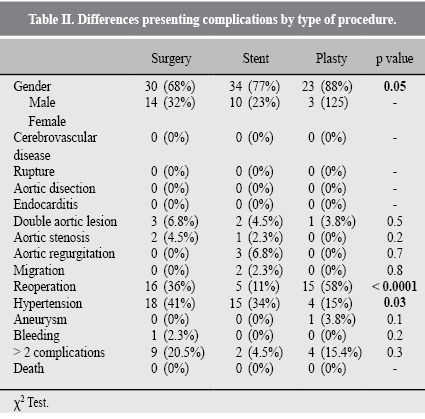
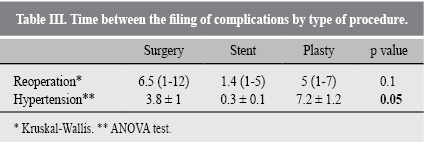
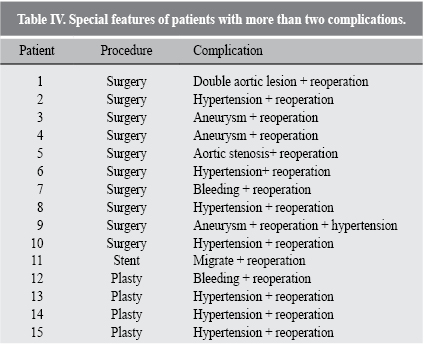
The statistically different complications according to the type of procedure were re-intervention and systemic arterial hypertension, as seen in table II. In stent aortoplasty, the time free of systemic arterial hypertension was the longest (Table III), this procedure was also the one with the lowest risk of reintervention compared with the rest of procedures (Figure 1). Open repair was the one with the highest rate of re-interventions, which are described in table IV.

DISCUSSION
Our patients show similarities to previous reports, male predominance and hypertension, as the main complication.
While the election treatment is given by the individualized intervention criteria and the experience in each center; the universal recommendation is that percutaneous approaches like aortoplasty are performed in children without other injuries, while stent aortoplasty is preferable in those adults with isolated CoA and poststenotic aneurysmal dilatation.8
We observed complications such as endocarditis and aortic valve lesion without achieving statistical significance, we consider that this facts are not procedure dependent but on the previous anatomy of the valve prior to the procedure, or the coexistence with bicuspid aortic valve.
The balloon aortoplasty was the procedure less associated with hypertension, and showed longer time presentation. We relate these findings that this procedure is performed in children, where the growth has not yet completed and the age is not a risk factor to the hypertension development. The group of patients treated with stent showed aortoplasty have lower complication rate compared with the treated group ballon aortoplasty, but complications such as hypertension and reoperation occurred in less time; This is explained in which the subjects selected had probably arch hypoplasia or unfavorable anatomy and added that in adulthood essential hypertension manifests.
In adulthood, Any type of intervention is prone to hypertension development due to the sum of previous factors such as endothelial modifications and angiogenic effects stimulated by the surgical procedure. Taelman L et al, described an exacerbated response in those endotheliums mostly handled as in the case of repeated aortoplasty and surgery.9
Cannife et al10 in a systematic review found 32.5% prevalence of hypertension in CoA patients, and showed that the main factors to its development are: late-age correction, invasive procedures and repetitive interventions raise the likelihood to manifest.
CONCLUSIONS
In our study, high blood pressure and reoperation were the most frequent complications.
The balloon aortoplasty presents greater percentage of reoperation; and aortoplasty stent has fewer complications, but these are manifested in less time.
REFERENCIAS
1. Jarcho S. Coarctation of the aorta. Am J Cardiol. 1962; 7: 544-547. [ Links ]
2. Jasper A, Keshava SN. Aortic coarctation associated with an absent segment of the proximal right subclavian artery. J Postgrad Med. 2014; 60: 397-399. [ Links ]
3. KobyliÅska J, DworzaÅski W, Cendrowska-Pinkosz M, DworzaÅska A, Hermanowicz-Dryka T, Kiszka J et al. Morphological and molecular bases of cardiac development. Postepy Hig Med Dosw (Online). 2013; 67: 950-957. [ Links ]
4. Pinto Júnior VC, Branco KM, Cavalcante RC, Carvalho Junior W, Lima JR, de Freitas SM et al. Epidemiology of congenital heart disease in Brazil. Rev Bras Cir Cardiovasc. 2015; 30: 219-224. [ Links ]
5. Ostovan MA, Kojuri J, Mokhtaryan M, Razazi V, Zolghadrasli A. Procedural outcome and one year follow up of patients undergoing endovascular stenting forcoarctation of aorta: a single center study. J Cardiovasc Thorac Res. 2014; 6: 117-121. [ Links ]
6. Vassilev DI, Rigatelli G, Kaneva-Nencheva A, Levunlieva E, Alexandrov A. Prevention of cerebral embolization by placing a neuroprotection filter before recoarctation stent dilation. JACC Cardiovasc Interv. 2014; 7: e11-e12. [ Links ]
7. Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Bolger AF, Levison ME et al. Infective endocarditis diagnosis, antimicrobial therapy, and management of complications a statement for healthcare professionals from the committee on rheumatic fever, endocarditis, and Kawasaki disease, council on cardiovascular disease in the young, and the councils on clinical cardiology, stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association. Circulation. 2005; 111: e394-e434. [ Links ]
8. Saxena A. Recurrent coarctation: interventional techniques and results. World J Pediatr Congenit Heart Surg. 2015; 6: 257-265. [ Links ]
9. St Louis JD, Harvey BA, Menk JS, O'Brien JE, Kochilas LK. Mortality and operative management for patients undergoing repair of coarctation of the aorta: a retrospective review of the pediatric cardiac care consortium. World J Pediatr Congenit Heart Surg. 2015; 6: 431-437. [ Links ]
10. Canniffe C, Ou P, Walsh K, Bonnet D, Celermajer D. Hypertension after repair of aortic coarctation--a systematic review. Int J Cardiol. 2013; 167: 2456-2461. [ Links ]
Nota
Este artículo puede ser consultado en versión completa en: http://www.medigraphic.com/revmexcardiol














