BACKGROUND
Obstetric violence is defined as an action or intentional omission by a healthcare professional which hurts, damages, or degrades a woman during pregnancy or birth, as well as medical negligence (Grupo de Información en Reproducción Elegida, A. C., 2015). Various studies demonstrate that this type of violence is frequently reported by women (Castro & Frías, 2020; Treviño-Siller et al., 2018, 2020) and can be normalized and accepted as part of the childbirth experience in the healthcare system of countries such as South Africa (Malatji & Madiba, 2020), Colombia (Vallana Salas, 2019), Argentina (Herrera Vacaflor, 2016), Ecuador (Meijer, Brandão, Cañadas, & Falcon, 2019), Brazil (Alexandria et al., 2019), the United States (U.S.) (Diaz-Tello, 2016), and Mexico (Valdez Santiago, Arenas Monreal, Rojas Carmona, & Sánchez Domínguez, 2018).
While most of these studies emphasize the violence exerted by doctors and obstetricians, this article highlights the perceptions of nursing staff about childbirth care and how they normalize, justify, and even exercise this type of violence. Although some studies (Brilhante & Jorge, 2020; Espinoza-Reyes & Solís, 2020) have explored the perception of obstetric violence from the point of view of nursing personnel, there is a need to analyze these cases as scant evidence suggests that the nursing staff also exerts violence during delivery care. In addition, they spend the most time with women during labor.
The World Health Organization (WHO) has declared that all women have the right to receive the highest level of health care, including the right to dignified and respectful prenatal and postnatal care free from violence and discrimination (World Health Organization, 2015). Despite Mexican and international standards, some 830 women die each day due to pregnancy and birth complications (World Health Organization, 2018). In Mexico, this phenomenon has been studied since the 1980s, when international conventions and conferences began to expose inequalities, discrimination, and the lack of human rights guarantees for women: particularly regarding sexual and reproductive rights (United Nations, n.d.).
This, in turn, influenced the creation of the United Nations Millennium Development Goals, within which the third and fifth are intended to promote gender equality and women’s autonomy, as well as to improve maternal health, respectively. However, none of these goals have been fulfilled.
In Mexico, the Maternal Mortality Ratio (MMR) is an estimated 31.2 deaths for every 100 000 births. Baja California is one of the five states with the highest maternal deaths and an MMR of 83.8, well above the national average (Secretaría de Salud, n.d.). From June 1996 to December 2007, the National Commission of Medical Arbitration (acronym in Spanish, Conamed) processed 18 443 complaints, of which 15% were from the obstetric and gynecologic specialty (Secretaría de Salud, n.d.). Upon further analysis of the most severe damages to health (permanent impairment and death) by specialty, obstetrics and gynecology were in the first place, with 53% of complaints belonging to these fields (Secretaría de Salud, n.d.).
As data from 2016 demonstrates, 33.4% of women suffered some form of abuse by the caregiver of their last birth. Also, mistreatment was reported during care by 40.8% of the women who gave birth in the Mexican Institute of Social Security (acronym in Spanish, IMSS) and 38.7% of those who received care in a local hospital or public clinic. Furthermore, it was reported that during their last birth, 4.2% of Mexican women were given some form of contraceptive or were operated upon or sterilized without consent; 7% were harassed with offensive or shaming comments; 9.2% were obligated to remain in an uncomfortable physical position; 9.2% were pressured to receive some form of contraceptive or ligating fallopian tubes; 9.9% were ignored after birth when they asked for their infants; 10.3% reported neglect as punishment for yelling or complaining too much; and 11.2% were yelled at or scolded (Inegi, 2017).
In Baja California, 34.8% of women reported experiencing any of these types of abuse is above the national average, as for indigenous women, it increases to 40%. Given the low visibility awarded to this problem in the media, an important indicator at the state level is the recommendations issued by human rights organizations for obstetric violence. In this regard, Espinoza Reyes (2019) reports the existence of 10 recommendations directed to public and private health institutions in the municipalities of Ensenada, Tijuana, and Playas de Rosarito, which range from denial of service to women in labor culminating in fortuitous births that occurred in the streets causing the death of the newborn or the mother. In this sense, the present investigation aimed to analyze the nursing staff’s perceptions regarding the mistreatment of women during labor and childbirth through a qualitative study conducted using discourse analysis of 23 interviews conducted in Baja California, Mexico.
Obstetric Violence Concept and Legislation
In Mexico, norms such as the NOM-007 and the Clinical Practice Guides seek to promote the use of practices based on the best available scientific knowledge adhering to current regulations and the human rights framework (Cenetec, 2014). Similarly, there are instruments through which states establish the right to a life free of obstetric violence, such as the State Law for Women’s Access to a Life Free of Violence (H. Congreso del Estado de Baja California, 2008).
Baja California included the concept of obstetric violence in its legislation in 2016, where it is defined as:
Any conduct, action or omission carried out by health personnel, directly or indirectly, and that affects women during the processes of pregnancy, childbirth, or puerperium, through dehumanized treatment, omission of timely and effective care, practices without consent such as sterilization or cesarean section for no reason5 (H. Congreso del Estado de Baja California , 2008, p. 4).
Currently, approximately two-thirds of the Mexican states have included this concept in their laws. In general, it is possible to point out that Mexico has an important regulatory framework in the field of health and prevention, punishment, and eradication of violence against women.
Some researchers have described obstetric violence as a complex and multifactorial phenomenon rooted in elements such as “power relations, discrimination, social and gender inequality, as well as structural conditions such as deficiencies in infrastructure and supplies in the medical units; the strenuous and poorly paid conditions in which health personnel work and the ignorance of women’s rights”6 (Meza, Mancinas, Meneses, & Meléndez, 2015, p. 361). In this same sense, it is useful to understand obstetric violence as a device that is a heterogeneous set of discursive or non-discursive elements with a specific strategic function and inscribed in a power relationship, which results from the crossing of power and knowledge relationships (Agamben, 2009).
Based on these approaches, it is important to understand violence in all its dimensions and peculiarities, focusing on its direct manifestations and cultural and structural elements (Galtung, 2016). In this sense, Cohen Shabot (2016) explains that obstetric violence must be analyzed as a phenomenon different from medical violence and violence in general because it is a feminist question since the laboring bodies are perceived as a threat to the vision of hegemonic power about femininity. Thus, they need to be domesticated. A role played by what Arguedas Ramírez (2014) calls ‘obstetric power,’ that is:
this form of disciplinary power framed within the scope of women’s reproductive capacity and, therefore, exercised in a gender-specific territory: the bodies that can become pregnant and give birth. The microphysics of power that are present in this exercise produce docile and sexed bodies; they are the bodies that, in the social structure of patriarchy, require a particular discipline to channel the economy of reproduction, for which this obstetric power has certain disciplinary technologies7 (Arguedas Ramírez, 2014, p. 156).
The medical field and its culture, particularly the authoritarian medical habitus, have been widely explored by Castro (2014), who explains the enormous asymmetries existing in the relationships between doctors and their patients, especially in the case of pregnant and laboring women. In recent work, Villanueva and Castro (2020) describe the highly hierarchical functioning occurring within this field, which operates from four classification systems: professional, subfields, specialties, and division of labor.
In this context, nursing personnel is subordinated to physicians because of the way in which different professions are valued by those who make up this field. Anyone within the healthcare personnel can exercise violence, yet this hierarchy puts the nursing staff at a disadvantage when witnessing mistreatment, abuse, or disrespectful behavior toward women. Power asymmetries often make them silent witnesses of these practices, as shown by the work of Oliveira and Penna (2017). However, we wonder how much the nursing staff justifies or normalizes this type of violence since they spend more time with women during labor and delivery. The naturalization of hierarchical domination that places nursing personnel as silent witnesses can be categorized as symbolic violence, a form of obstetric violence that makes them part of the process of violence toward pregnant women (Jojoa-Tobar et al., 2019).
Another important element in the origin of obstetric violence is the lack of a solid culture of rights in Mexico. Although, as indicated in this article, the development of a normative framework in this matter has presented enormous advances in the last four decades, there is still work to be done regarding human rights education. That is, work towards the conformation of reproductive citizenship, in which both women and health personnel are informed about the forms to appropriate, exercise and defend their rights, in the case of the former regarding their sexual and reproductive health, and of service providers in relation to the creation of working conditions that allow them to exercise their professions following scientific evidence and providing woman-centered birth care.
Studies from scholars such as Espinoza-Reyes and Solís (2020) demonstrate that through an individual agency, women face significant obstacles to access mechanisms of enforceability and justiciability. They also highlight the existence of a collective agency that is beginning to emerge in these communities through the joint work of academic institutions, NGOs, and social networks. One of the most important tasks that these groups have is to advance in the analysis and visibility of this phenomenon.
Therefore, given that obstetric violence and mistreatment occur in health institutions by health professionals, the goal of this study was to explore the perceptions of hospital nursing staff regarding birth and the care of women who receive it. Of further interest was to identify whether personnel recognized violent care practices and the causes attributed to this violence and generate suggestions to achieve better treatment during care.
DESIGN AND METHODS
The present is a qualitative study using discourse analysis, centered on language as the form of interaction: behaviors and thoughts interpretation of interview subjects through their expression in discourse under the interpretivism paradigm (Silverman, 2011). The study took place in five public hospitals in the state of Baja California, Mexico. We received authorization from directives of all the hospitals to perform the interviews, and the chief nurses facilitated interview schedules and dates. The snowball sampling technique was used, through which nurses from two more hospitals were identified for interviews. A total of 23 interviews were completed for sampling saturation, carried on between October 2018 and April 2019.
An interview guide was designed based on the indicators of the Official Mexican Norm for pregnancy, birth, and puerperium care (NOM-007-SSA2-1993) and the recommendations of the World Health Organization, which was reviewed and approved by subject-matter experts. An interview guideline trial was conducted with nurses who had an extensive obstetric experience but were no longer working in the area. All interviews were voluntary and all participants were informed of their rights (confidentiality and anonymity), that the results would be used only for purposes of scientific study and through informed consent approved by the Bioethics Committee of the Autonomous University of Baja California’s School of Medicine and Psychology.
Additionally, interviews were audio-recorded and transcribed, after which content analysis was conducted using the Atlas.Ti software, version 6.2. We define direct and indirect obstetric violence as the two main categories of analysis; institutional factors are derived from the latter. These categories were consequently data coded, as shown in Figure 1.
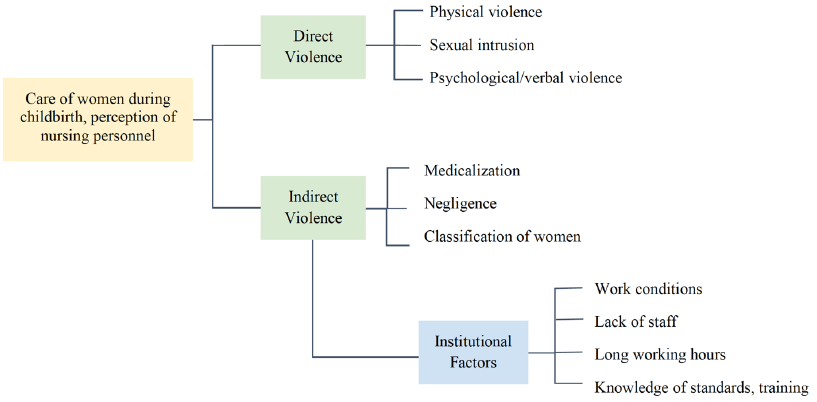
Source: Authors’ elaboration based on interviews with nursing staff of hospitals in Baja California, Mexico.
Figure 1. Categories and Subcategories of Analysis of the Nursing Perspective on the Care of Women in Labor in Baja California
The first category was established because hospital obstetric and gynecological services are among the three top medical specialties which receive the most complaints in the National Commission of Medical Arbitration (acronym in Spanish, Conamed), of which these relate to surgical procedures, doctor-patient relations, birth care, and more (Rangel Flores, Martínez Ledezma, Hernández Ibarra, & González Acebedo, 2019).
Discourse analysis of study participants revealed two different types of obstetric violence, which the research team identified as direct and indirect. Direct obstetric violence was considered as actions toward women seeking care with the intention to offend, hurt, or potentially harm the mother or infant during pregnancy and birth. In interviews, topics discussed included verbal and physical violence and sexual intrusion. The latter is defined as any unjustified touch or incision of the woman’s genital area. Including excessive contact during the labor phase by nursing and medical professionals (Secretaría de Salud, n.d.) and student interns who should maintain minimum tactile interaction (Valdez-Santiago, Hidalgo-Solórzano, Mojarro-Iñiguez, & Arenas-Monreal, 2013), and/or episiotomy without patient consent.
Other procedures were also applied without consent and/or were unjustified by medical necessity, such as placement of contraceptive devices, use of oxytocin and anesthesia or analgesics, and unnecessary Cesarean sections. Regarding this final element, Valdez-Santiago et al. (2013) found that in the state of Morelos, Mexico, 57.4% of births were Cesarean sections, of which only 7.4% were scheduled, despite the World Health Organization directive that these should not exceed 10 to 15% of births (World Health Organization, 1996).
These events were identified as indirect obstetric violence, which refers to unjustified medicalization, negligence, or labeling women based on discriminatory prejudices, which was identified in the present study. Also, an indirect obstetric violence subcategory is constituted by institutional factors limiting or even obstructing the possibility of offering good care to women during the birth process. Training and knowledge of applicable standards were also considered, specifically regarding the NOM 007 and the World Health Organization recommendations.
RESULTS
Participant characteristics
Interviews were carried out with 23 nurses, 19 were female, and four were male. The average age was 38.7 years; four participants were unmarried, one widowed, and the rest 18 were married or in a relationship. Only three participants did not have children, and the remaining 20 had an average of 2.2 children. Eighteen had a higher degree or specialty in nursing, and five had technical degrees. Participants had spent between one and 30 years practicing their profession, with the majority having spent five to seven years in the field.
Table 1. Characteristics of the Nursing Staff Interviewed
| Number of interviewees |
Sex | Age (years) |
Marital status |
Number of children |
Academic background | Years of experience in obstetrics and gynecology |
|---|---|---|---|---|---|---|
| 1 | F | 31 | Single | 0 | Nursing degree / Specialty in perinatal nursing |
4 |
| 2 | F | 36 | Married | 2 | Nursing degree in obstetrics and gynecology |
6 |
| 3 | F | 44 | Married | 2 | General nursing | 5 |
| 4 | F | 48 | Widowed | 2 | Nursing degree | 3 |
| 5 | M | 40 | Free union | 3 | Nursing degree / Specialty in intensive care |
5 |
| 6 | F | 45 | Free union | 1 | Technical degree in nursing |
7 |
| 7 | F | 47 | Single | 4 | Assistant nurse | 3 |
| 8 | F | 52 | Married | 4 | Assistant nurse | 2 |
| 9 | F | 33 | Married | 2 | Nursing degree | 4 |
| 10 | F | 29 | Free union | 0 | Nursing degree | 3 |
| 11 | F | 30 | Free union | 2 | Nursing degree | 5 |
| 12 | M | 44 | Married | 2 | Nursing degree | 1 |
| 13 | F | 28 | Free union | 2 | Nursing degree | 1 |
| 14 | M | 31 | Married | 1 | Nursing degree | 2 |
| 15 | M | 46 | Married | 2 | Nursing degree / Specialty in obstetrics |
16 |
| 16 | F | 24 | Single | 0 | Nursing degree | 2 years 6 months |
| 17 | F | 50 | Married | 2 | General nursing | 25 |
| 18 | F | 54 | Married | 2 | Nursing degree | 30 |
| 19 | F | 35 | Married | 2 | Assistant nurse | 3 |
| 20 | F | 40 | Married | 3 | Nursing degree | 18 |
| 21 | F | 51 | Single | 3 | Technical degree in nursing |
6 |
| 22 | F | 40 | Married | 2 | Nursing degree | 6 |
| 23 | F | 43 | Married | 3 | Technical degree in nursing |
1 |
Source: Authors’ elaboration based on interviews with nursing staff of hospitals in Baja California, Mexico.
OBSTETRIC VIOLENCE
Verbal Violence
All participants acknowledged manifestations of obstetric violence towards women seeking care. Interviews indicated that verbal violence was the most frequent, and occurs in different moments of care, most often at the moment of birth when women are very close to delivery, and external stimulus, exhaustion, and emotions are heightened.
Commonly, violent statements alluded to the pain suffered by women, as well as their sexuality, number of children, physical aspects, and even reprimands or sarcastic comments. Some testimonies highlighted insensitivity towards the pain of childbirth contractions: “some say, and pardon the expression, ‘I bet when you were fucking you didn’t complain like this!’, or ‘When you opened your legs [the first time]!’” (44 years-old female nurse, five years of experience, personal communication, October 04, 2018).
Statements like these judged women’s sexuality as if they were not permitted to feel pleasure, and the pain of birth was a punishment for it. Another manifestation of verbal violence, constant throughout participant discourse, was the allusion to the woman’s physical features:
I’ve seen doctors yelling to the pregnant women. They called one patient a whale because she was morbidly obese and pregnant. The doctor kept saying they would need a harpoon to give her anesthesia, they called her a whale, and the woman cried and cried and cried — and me along with her— they said to her: ‘I’m not going to use a needle, I’ll use a harpoon on you’ (40 years-old female nurse, six years of experience, personal communication, October 27, 2018).
Also frequent were comments regarding women’s number of children, scolding, and sarcasm, which according to nurses, tended to come from peers or, more commonly, doctors or gynecologists, indicating a deflection of the responsibility for committing obstetric violence. In contrast, they positioned themselves far less frequently as the perpetrator of violence:
“look honey, if you don’t want your baby to end up disabled or something, push, the kid is already there, you can already see his little back face, the child has to breathe.” I know it’s obstetric violence, but I also understand that you’re there in the moment, the kid has to come out, she has to get him out, we can’t get him out on our own and yes, actually it worked because she pushed and pushed, and the kid came out; it’s obstetric violence and there are times when we do it without meaning to (48 years-old female nurse, three years of experience, personal communication, September 29, 2018).
In this case, there is ambivalence in the participant’s discourse; she recognizes her own use of violence and knows this is unacceptable behavior. However, she justifies these actions because of their work. Here we can ask ourselves if there are no better strategies to facilitate cooperation during labor.
Physical Violence
Physical violence in obstetric care involves invasive practices. In this article, they have been denominated as sexual intrusion and disrespect for the natural stages of birth, that is, invasive or unnecessary practices that can contribute to physical damage to the woman or newborn.
That the woman is constantly examined; one person arrives and puts his hands on her, another comes and does the same. It’s not one single person providing care from start to finish, it’s everyone in the world examining her; that is obstetric violence (40 years-old female nurse, six years of experience, personal communication, October 27, 2018).
Procedures without patient consent are also considered to be physical obstetric violence. As stipulated by the Mexican National Commission of Bioethics (Arnau Sánchez et al., 2012), regarding patient autonomy, consistent bioethical responsibility by the medical professional, high quality of service, guaranteed respect and dignity towards the patient providing them information, options, and assuring his or her complete understanding should lead to freedom of choice for the patient. Nonetheless, some study participants stated that there is no adequate tactic to ensure that these care procedures are performed effectively in birth settings, constituting indirect obstetric violence, in the sense that it inflicts unintentional harm on the woman seeking care but is believed to be normal within the hospital culture.
Also, it was discovered that non-recommended practices were performed. Some were justified by the nursing staff in events classified as emergencies or due to an adverse health condition of women, and other practices were known to be avoided, such as inappropriate use of medications, unjustified cesarean sections, etcetera.
They often put their hand inside the patient, they medicate her so that her uterus or vagina dilates even though she doesn’t want to take analgesics, but they give it to her anyway, so somehow the human aspect is lost (51-year-old female nurse, six years of experience, personal communication, October 01, 2018).
Analgesic use is not a practice to be avoided outright. However, it should always take place respecting the woman’s decision; some women wish to use them (Belli, 2013) and are denied, representing another form of forced control and lack of respect.
Subsequently, cesarean sections were a constant topic in the participant discourse. Most were aware that this is a practice that should be minimized and assured that some childbearing women do wish to have one. Nonetheless, there are still physicians who perform Cesarean sections without consent, justifying them as medically necessary. As stated by one of the nurses: “they gave one pregnant patient a Cesarean and it wasn’t necessary; she didn’t want a Cesarean and (…) the birth could have been physiological, the natural way” (54-year-old female nurse, 30 years of experience, personal communication, October 04, 2018).
Another example:
She’s dilated at five [centimeters], and I’m getting ready to leave her (…) and soon afterwards ‘don’t worry, we gave her a Cesarean’ [referring to what the physician said to the nurse participant]. But wait a second, when did you tell me you would do that? You never told me. All the patients must be informed (40-year-old, male nurse, five years of experience, personal communication, September 30, 2018).
Additionally, it was common for interviewees to recall episiotomies as a practice that would accelerate birth. They were performed by physicians mostly without the time necessary to allow natural dilation and amnio rhexis. This was sometimes worsened by the failure to receive patient consent:
here many times they’re in a hurry and they do the episiotomy when the woman doesn’t agree with getting one, but right then she’s in no position to negotiate, they just tell her “The baby’s not coming (…) you’re not dilating and let’s do it,” because they didn’t allow her the proper time to dilate naturally (51-year-old female nurse, six years of experience, personal communication, October 01, 2018).
All the previous testimonies are seen as part of the interference that is recognized as direct violence due to the pressure for the delivery to occur at the time that best suits the health personnel, without respecting the natural time, going against what is recommended by the World Health Organization (1996).
Conversely, participants commented that most women are scared during the birth process, which is usually more common in first-time, underage, older adult mothers, and women without prior training or information about the birth process. The study participants classified women according to different manifestations of their fears and experiences (Table 2).
Table 2. Type of Women in Labor According to the Classification of Nursing Personnel
| Type | Testimonies |
|---|---|
| Scared women | “She’s scared, she doesn’t know what is going to happen” (29-year-old female nurse, three years of experience, personal communication, October 24, 2018). “They are really scared, you come near them with a syringe, and they turn to look at you and you just have to tell them ‘My dear, I’m going to give you this (…) and it’s for this’” (44-year-old female nurse, five years of experience, personal communication, October 05, 2018). |
| Demanding women |
“Somehow [the women] will always feel that we haven’t given them our best effort (…) they always want someone by their side but that’s impossible, it’s an enormous amount of work and, well, no!” (44-year-old female nurse, five years of experience, personal communication, October 05, 2018). |
| Underage girls and adolescents |
“We’ve had 13-year-old childbearing girls, 13, 15 years old and that’s when (…) yes, it frustrates us because they’re little girls, but we’re not going to treat them badly for that, so, yeah I’ve heard many people tell them ‘what are you doing here?,’ ‘you should be in school,’ speaking to them in this way, bluntly, and it’s like, well, you’re a little girl, what are you doing? And so, she feels bad, and then she starts to cry. When they’re this age they cry because they’re scared” (28-year-old female nurse, one year of experience, personal communication, October 25, 2018). “I’ve had to take care of girls as young as 13, many are underage, 13, 14, 16 years old, there are so many young girls these days having babies, so many!” (48-year-old female nurse, five years of experience, personal communication, September 29, 2018). “‘Oh, now you scream but when you were [having sex] (…)’ and with things like these, ‘(…) then you didn’t scream,’ or ‘oh, now you want your mother but when you were doing it, with what you were doing you didn’t want your mother then’” (31-year-old male nurse, two years of experience, personal communication, October 04, 2018). |
| Difficult women | “Some patients are aggressive, but it’s almost always because they have some sort of mental illness. We’ve had female patients who are schizophrenic, or who are drug addicts” (29-year-old female nurse, three years of experience, personal communication, October 24, 2018). “The drug addicts don’t obey the doctor or us, they pull us, scratch, everything, so with them it’s a bit difficult to handle them” (45-year-old female nursing technician, seven years of experience, personal communication, September 30, 2018). “They yell, some because of the pain, some because they want to leave, others are at the point where they need their next hit because they’re drug addicts” (24-year-old female nurse, two years of experience, personal communication, September 19, 2018). |
| Women with no prenatal care |
“It’s crazy that patients arrive, and they’ve gotten no prenatal care, they bring nothing, seeing that they don’t even care enough to do the proper prenatal care” (44-year-old female nurse, five years of experience, personal communication, October 05, 2018). “So, they haven’t gotten any prenatal care, much less an ultrasound, they haven’t even done a blood test, so they come with nothing, and it’s really risky to her and to the baby” (48-year-old female nurse, three years of experience, personal communication, September 29, 2018). |
Source: Author’s elaboration based on interviews with nursing staff of hospitals in Baja California, Mexico.
The lack of sensibility is evident in how the nursing staff classifies the different types of women in labor according to their attitudes or feelings. This discourse allows us to interpret what attitude they would have, thinking that they have the faculty to deny service or some care, or get absent adopting an unprofessional attitude (Da Silva Carvalho & Santana de Brito, 2017). “there are some colleagues who seem not to listen and do not attend to them…” (50 years old female nurse, 25 years of experience, personal communication, October 02, 2018). Or they neglect them by prioritizing their own needs, “there are people who are very good, but there are many people who are very bad who have knowledge, but they just want to come, check and be seated” (31 years old female nurse, four years of experience, personal communication, September 14, 2018). This type of attitude and negligence leads us to institutional factors regarding the lack of nursing staff or difficult work shifts as factors that affect both women and the newborn.
Institutional Factors
Nursing staff participants mentioned various reasons for which they couldn’t provide respectful care to childbearing women seeking care. This included several institutional factors which obstructed respectful practices and woman-centered birth care.
One of the reasons was the oversaturation of patients in the facilities. A common practice that requires hospital staff to improvise spaces for childbearing women in full rooms or hallways. Participants agree that this diminishes care time and quality, as well as the information that the women receive; the same occurs in newborn care.
Although it is recognized that emotional support and accompaniment is one of the most crucial needs of women during labor and birth, in public sector health services, women cannot count on the presence of family members outside of highly limited visiting hours. On most occasions, health personnel, who generally cannot offer sufficient support, are the only people available.
Furthermore, participants revealed that occasionally, non-work-related issues interfere with care for childbearing women. Some referred to colleagues with multiple jobs who arrived to work tired or stressed, which contributed to poor treatment of patients.
The internal hierarchy between health personnel is also a barrier to quality care (Jojoa-Tobar et al., 2019); some of the nurses that participated in the study were more concerned about whether a task was part of their job description than about the adequate care for women during labor and birth.
Lack of personnel, exhaustion, and stress, alongside insufficient materials, are institutional factors that can affect the results of a birth. On some occasions, women had to be referred to other hospitals due to the lack of infrastructure or human and material resources.
Other factors related to the personnel themselves were the amount of experience in gynecological care, level of preparation, and individual attitudes, as well as prior training and with that, the knowledge and application of the appropriate standards guiding a series of practices, protocols, and instructions to facilitate respectful and woman-centered birth care. Participant discourse showed the belief that few health professionals have enough experience or adequate preparation, and that awareness of the Mexican Official Standard (NOM 007) is minimal. Finally, having more than one job seemed to be associated with a lack of empathy towards the pregnant woman (Table 3).
Table 3. Institutional Factors which Affect Fair Care of Women During Labor and Birth
| Factor | Testimonies |
|---|---|
| Excess of work and patient oversaturation in delivery areas |
“There’s too much work and only one nurse. I think it’s not enough to have only one nurse for, sometimes the beds which should be for eight patients get full and probably 20 more patients are there waiting, many incoming patients, almost 30, and well, there isn’t enough to go around” (40-year-old female nurse, 18 years of experience, personal communication, October 02, 2018). |
| Scarcity in the pediatric care ward |
“Quick, take the cradle from that baby, another is coming. So, sometimes the reality is we don’t have time to even clean the cradles. Just a clean sheet and bring the next one in, because of the volume of births we see” (36- year-old female nurse, five years of experience, personal communication, September 14, 2018). |
| Scarcity of personnel leading to exhaustion and stress |
“I believe that, if we had more staff, and more materials (…) Sometimes we’re running because we don’t have enough materials and that takes time and it tires us out, but if there was more staff (…) A tired worker isn’t the same as a more rested one; if there were more people, you could rest a half an hour and we would be really thankful while someone else stays with the patient, because we can’t make mistakes, patients are people. The night shift is when they should really have more staff, and it’s when they have less” (44-year-old female nurse, five years of experience, personal communication, October 05, 2018). |
| Transfer to other hospitals |
“A lot of us refer them to Tijuana, but only because our gynecologist didn’t show up, or we don’t have a blood bank. We don’t have intensive care, we attend the patients here and we take the risk, but plain and simple it’s dangerous when we send them away, that’s why we try to do the job with what we have here at our disposal” (48-year-old female nurse, five years of experience, personal communication, September 29, 2018). |
| Lack of empathy | “For having no empathy with the patient, for the (…) simply put, they are rude and don’t care what the patient is feeling” (51-year-old female with a technical nursing degree, six years of experience, personal communication, October 01, 2018). |
Source: Authors’ elaboration based on interviews with nursing staff of hospitals in Baja California, Mexico.
The training was reported as infrequent and sometimes imparted by personnel who were not in the obstetric-gynecological field. Many participants agreed on the necessity for greater training and more efficient supervision:
Training, supervision, that’s what’s missing. If there is good supervision, problems are identified because each person behaves as they want to if they are not supervised, ‘well, nobody is around to watch me, I’ll do as I please.’ Some people are great, and many others with expertise are terrible, but all they do is come, check, and sit around. Then if a supervisor acts the same way and does not come and keep an eye on us there, (…) whatever the worker wants is what happens (44-year-old male nurse, one year experience, personal communication, Oct 25, 2018).
Due to this, many of the personnel interviewed were unaware of the NOM 007. Even if they knew it, they could only describe general aspects of it, as well as the WHO recommendations for dignified and humanized treatment of the pregnant woman. All responses were identical when participants were asked if they had heard about the NOM 007. As stated by the interviewees, “the 007 is the one that (…) yes, I know it (…) it’s the one about (…) maternal care of the newborn and postpartum woman” (24-year-old female nurse, 2.5 years of experience, personal communication, September 19, 2018); “Ah! I don’t know, what is it?” (40-year-old, male nurse, five years of experience, personal communication, September 30, 2018).
As far as the World Health Organization recommendations, only one participant mentioned them:
That is already established. At the global level the World Health Organization identified all the indicators we mentioned, they are indicators precisely because they tell you what the problem is that they indicate, the very word explains itself, they let you know what is happening around the world. And it’s global, it isn’t national, so if you already know what’s going on, then it’s just a matter of enforcing it (44-year-old male nurse, one year experience, personal communication, October 25, 2018).
In addition, as considered by the nursing staff, an institutional factor that leads to some of the deficiencies is the budget lines that are completed before the end of the year, as mentioned by one of the participants:
Especially from October, the budget is closed and when it closes, you can’t buy anything. Normally we are full, and it is normal that in these months there is no budget and obviously there are no purchases, and if there is no purchase then there are no supplies and if there are no supplies there is no good care (34-years old male nurse, one year of experience, personal communication, October 25, 2018).
DISCUSSION
The main finding of this study is the perception of the nursing personnel working in public health services as witnesses of obstetric violence by the medical personnel. The interviewees mentioned different types of violence, such as direct, physical, and verbal violence, including indirect violence exercised through excessive and unnecessary cesarean sections and usage of painkillers and episiotomy, to name a few.
Another relevant finding was the identification of institutional factors contributing to these violent practices, which are becoming normalized and even justified as necessary, such as medicalization and the asymmetric relationship between medical staff and patients in which the childbearing women’s opinion is the least important of all (Almaguer González, García Ramírez, & Vargas Vite, 2010; Biurrun Garrido & Goberna Tricas, 2013; Pozzio, 2016).
Also, it was difficult for the nursing staff to perceive acts of omission of care or negligence as violent practices. However, indirect violence practices are detected in their discourse, such as the omission of service or prejudice when classifying pregnant women. This has also been seen in other studies in which the nursing staff, as well as the women interviewed after delivery, do not perceive these aspects as violent practices but rather as structural or institutional (Brilhante & Bessa Jorge, 2020; Da Silva Carvalho & Santana de Brito, 2017; Espinoza-Reyes & Solís, 2020). However, the World Health Organization, since 1997, and the Mexican Official Standard (NOM 007), mark these practices as violent, and such information is important for training nurses (Da Silva, Sousa, Oliveira, Amorim, & Almeida, 2020).
According to Almaguer et al. (2010) the different elements and behaviors that indicate obstetric violence can be classified into five categories based on the World Health Organization indications regarding medical procedures during pregnancy, birth, and postpartum. These categories are 1) technical procedures made routine, recommended for specific medical indications, 2) mistreatment and shaming, 3) unnecessary obstetric procedures performed for instructional purposes by students, interns, or medical residents, 4) budget and spaces designed for maternal care, 5) cultural and social mistreatment in reproductive health.
This study identified all these elements, especially those related to mistreatment, labeled as direct obstetric violence, and unnecessary procedures, labeled as indirect obstetric violence. This speaks to the necessity for institutional changes to pregnancy care in general and care during birth. These changes must affect infrastructure and the distribution of materials, as well as the constant training of health personnel working in the obstetric area, which should consider humanitarian values, base themselves on woman-centered care models and reeducate on the abolition of procedures that have been deemed harmful to women and newborns (Arnau et al., 2012; Biurrun-Garrido & Goberna-Tricas, 2013).
The results of this study are similar to those reported in other investigations from Mexico and other Latin American countries, which highlight obstetric violence from obstetricians and nurses. They also stress institutional barriers such as lack of space, poor and non-adequate conditions for birth attention (infrastructure), and the absence of sufficient training (Treviño-Siller et al., 2018; Valdez Santiago et al., 2018). Nevertheless, the present study contributes to the understanding that the very personnel involved acknowledge this violence and sometimes justify it, highlighting the necessity to promote a culture of fair treatment based on human, sexual, and reproductive rights.
The discourse of the participants evidences the necessity to act upon these findings to solve this public health problem: an issue coming to light in Mexico as well as other Latin American countries and around the world, as reinforced by Bohren et al. (2015) in a systematic review of 65 obstetric violence studies across 34 countries.
Furthermore, these behaviors are incorporated into care practices to the point of being normalized, which prohibits conscious reflection about their use (Almaguer et al., 2010; Jojoa-Tobar et al., 2019; Pozzio, 2016) and consequent rejection or resistance of them (Biurrun Garrido & Goberna Tricas, 2013; Bohren et al., 2015).
As in other related studies, the results of the present study show that the key negative emotions of women in prenatal care are: fear of the pain of birth and misaligned expectations (Pozzio, 2016), some even maintaining their fear up to a year after birth (Arnau-Sánchez, Martínez-Ros, Castaño-Molina, Nicolás-Vigueras, & Martínez-Roche, 2016; Hildingsson, Nilsson, Karlström, & Lundgren, 2011); negative experiences during birth such as mistreatment and obstetric abuse which may also contribute to Post-Traumatic Stress Disorder (PTSD) in women who have never before experienced symptoms (Dekel, Stuebe, & Dishy, 2017); anxiety and insecurity in the form of confronting the threat of misinformation; loss of trust in medical personnel (Mukamurigo, Dencker, Ntaganira, & Berg, 2017); shame at the violation of privacy; anger and helplessness at the asymmetrical hierarchy of the hospital structure (Da Silva Carvalho & Santana de Brito, 2017; Menéndez, 2003) wherein the female patient is the last place decision-maker forced to submit to the expert professional (Arguedas Ramírez, 2014; Castro, 2014; Secretaría de Salud, 1993), and loneliness, seen in discontinuity in attendance.
Finally, as has been reported in other studies (Pozzio, 2016; Treviño-Siller et al., 2020), health personnel showed very little knowledge of the NOM, highlighting the necessity to increase awareness. The application of this standard does not limit the work of health professionals; it rather contributes to reducing risks during pregnancy, birth, and postpartum care, even protecting health personnel in the case of complications. The NOM is based on evidence at an international level (Arnau Sánchez et al., 2012). It provides actions so that woman-centered care is carried out under the principles of reproductive rights, such as respect for women’s decisions regarding their reproductive and sexual life. It strengthens their autonomy and rejects the idea of childbirth as a pathological or unnatural process. These advancements must be used to benefit the newborn child and women throughout their pregnancy, birth, and the postpartum period as greater technology and personnel with problem-solving capacity become available (Ayoubi et al., 2020).
CONCLUSIONS
Multiple studies confirm the existence of obstetric violence all around the world. Unfortunately, the state of Baja California, Mexico is no exception. The present study identifies instances of both direct and indirect obstetric violence, as well as institutional factors contributing to the mistreatment of pregnant women and new mothers. There is a clear need to improve the treatment of women during labor and birth, beginning with fostering greater awareness of the current Mexican Official Standard (NOM 007) through constant training on the woman-centered care stipulated by international recommendations. Furthermore, sufficient staff and continuous supervision of those who attend women in the birthing process is critical, as is maintaining an adequate stock of hospital and medical materials.
Scholars such as Espinoza-Reyes and Solís (2020) allow us to understand this public health problem through interviews with several women who had given birth at some point in recent years, where they expressed the violence suffered in public and private hospitals of Baja California. Subsequently, Ayoubi et al. (2020) conducted focus groups with postpartum women, and based on this, they developed an evaluation instrument to measure women’s experience of respectful maternity care.
Considering the evidence presented by previous studies and our own, it is crucial to direct new research to investigate why health professionals involved in birth and maternity care continue mistreating women in childbirth, although the recommendations made by the World Health Organization are more than three decades old.
RECOMMENDATIONS
Every health care institution should perform periodic and objective internal evaluations and take the consequent actions to correct incongruencies. Better supervision of health personnel performance is needed, along with training for obstetric-gynecologic personnel regarding the NOM 007, its indicators, and the World Health Organization standards. In addition, it is important to promote empathy and positive attitudes towards childbearing women in general and even more so during labor and birth. Institutional factors must be addressed, such as better shift management, improving general attitude towards women during birth care, and seeking out more and better supervision strategies to identify and correct inadequate practices. Provide the required materials and treatment areas since meeting the needs of health professionals may increase the chances that they will provide timely and respectful care for pregnant and laboring women, turning gestation processes into rewarding experiences.











 texto en
texto en 



