Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Frontera norte
versión On-line ISSN 2594-0260versión impresa ISSN 0187-7372
Frontera norte vol.14 no.27 México ene./jun. 2002
Artículos
Medical Compliance and Childhood Asthma on the Mexican Border: "They Think You Are God"
Procedimiento médico y asma infantil en la frontera mexicana: "Piensan que eres Dios"
Norah Schwartz*
* Investigadora del Departamento de Estudios de Población de El Colegio de la frontera Norte. Correo electrónico: schwartz@colef.mx.
Artículo recibido el 19 de febrero de 2001.
Artículo aceptado el 22 de mayo de 2001.
Abstract
Often chronic and potentially life threatening, asthma is one of the most common of all childhood illnesses. It is a known risk factor tor pneumonia, as well as tor other acute respiratory infections (ARI). ARIs have become a major focus of study for medical anthropologists. However, little ethnographic research has been conducted on the treatment of chronic childhood respiratory illness. Because of the worldwide increase in antibiotic resistance, understanding how and why treatment choices are made is imperative. This research focuses on life experiences and treatment strategies of mothers of young children with asthma residing in Tijuana, Mexico. Management of illness takes place not only in the clinic but also in relation to home health, pharmaceutical, and traditional medical care. Is there a standard definition of medical compliance followed by all physicians? How does the definition of "compliance" from the perspective of the physician compare to that of the patient? Because children with chronic illness are prone to acute infections, studies of this nature can provide useful insight into treatment choice for both chronic illness and infectious disease.
Keywords: 1. health, 2. childhood asthma, 3. medical pluralism, 4. Mexico, 5. Tijuana.
Resumen
Con frecuencia, el asma es una amenaza crónica y potencial a la vida, v es una de las enfermedades más comunes de la infancia; también es un conocido factor de riesgo en casos de neumonía y de otras infecciones respiratorias agudas, las cuales se han convertido en tema central de estudio para los antropólogos médicos. Para este análisis, hemos realizado una pequeña investigación etnográfica del tratamiento de las enfermedades respiratorias crónicas de la infancia. Debido al incremento global en la resistencia antibiótica, es imperativo entender cómo y por qué se toman decisiones sobre las opciones de tratamiento. Esta investigación se concentra en experiencias de vida y estrategias de tratamiento que las madres dan a los niños residentes de Tijuana, México, que padecen asma. El manejo de la enfermedad no sólo tiene lugar en la clínica, sino también en su relación con la casa, el cuidado farmacéutico y los cuidados tradicionales. ¿Existe una definición estándar del procedimiento médico seguido por los doctores? ¿Cómo es la definición de "proceder" desde la perspectiva del médico en comparación con la del paciente? Debido a que los niños con enfermedades crónicas son propensos a infecciones agudas, estudios de esta naturaleza pueden ofrecer un conocimiento útil sobre opciones de tratamiento tanto para enfermedades crónicas como infecciosas.
Palabras clave: 1. salud, 2. asma infantil, 3. pluralismo médico, 4. México, 5. Tijuana.
Perhaps it is time to redefine the role of the physician
in the treatment of asthma and other chronic diseases.
Emilio Sanz (1999:8)
Quizá es tiempo de redefinir el rol del médico
en el tratamiento del asma y otras enfermedades crónicas.
Emilio Sanz (1999:8)
CHILDHOOD ASTHMA: AN OVERVIEW
As patterns of childhood morbidity and mortality shift in the developing world, the role of chronic illness becomes more prominent (Frenk 1991; Omran 1983). Asthma is increasing in prevalence and severity worldwide, and hospitalizations, especially among young children, are currently on the rise (Phelan 1994; Anderson et al. 1994; Jones 1994. See Map 1.) In Mexico, children under the age of four account for the highest rates of hospitalization and outpatient visits due to asthma. Mortality rates due to asthma for children between the ages of one and four rose from 9.2 per 100,000 in 1980 to 38.4 per 100,000 in 1987, a 300% increase in seven years. Those for children under the age of one rose from 30.9 per 100,000 m 1980 to 600.1 per 100,000 in 1987, representing a rise of nearly 2000% (Salas-Ramírez 1994). With increasing air pollution in large cities, we can expect asthma-related morbidity and mortality rates to continue to rise. The increase is already visible along the United States-Mexico border, as well as internationally (English and Schwartz 2000).
There is a growing concern in both the United States and Mexico regarding increasing child morbidity and mortality due to asthma. The U.S. Department of Health and Human Services (1991) claims that of all chronic diseases, childhood asthma is the number one cause for school absenteeism and for hospitalization of children. As recently as 1995 the official Epidemiological Report for Baja California did not include a category on the incidence of asthma (Secretaría de Salud de Baja California 1996; Salas Ramírez 1994). Yet, by 1999, asthma had become the seventh most frequent cause of morbidity in Baja California (Sistema Nacional de Vigilancia Epidemiológica 2000).
Despite a burgeoning epidemiological and clinical literature on childhood asthma along the United States-Mexico border, little exists on the psychosocial issues or economic decisions confronting Mexican families with limited resources and access to health care, or on the personal consequences for families facing emergencies (English et al. 1998; Christiansen 1996; Von Behren et al. 1999). What little has been written about compliance and asthma focuses on adult medication usage in Europe (Adams et al 1997).
Consumers in many parts of the world now have a choice between Western biomedical medicine and more traditional medical models. Many choose to combine the two. Latinos, in particular, continue to use home remedies and traditional healers for the treatment of common pediatric problems (Risser and Mazur 1995; Trotter 1981; Rubel 1960), and to treat the symptoms rather than the cause (Zayas et al. 1999). There is little communication among the various systems of medicine even though they exist side by side and often overlap. For these reasons, this article provides phenomenological and descriptive data from narratives and observations of the individuals who are most closely associated with the care and treatment of children with chronic asthma.
Asthma and Noncompliance
Studies conducted in Europe estimate that approximately 50% of all patients do not comply with their physician's advice on medication usage (Adams 1997). Noncompliance in the use of asthma medication is not unusual. Research conducted in Brussels, Belgium showed that "a majority of interviewed patients had a negative perception of anti-inflammatory therapy, specifically relating to issues of safety and efficacy. Peak flow meters were seldom used ... Distrust toward inhaled corticosteroids is common, with more than 30% of the patients expressing lack of belief in their beneficial effects and over 40% expressing fear of adverse effects" (Van Ganse et al. 1997: 203, 208).
Since the 1970s, social scientists have discussed widely the issues associated with doctor-patient interaction, patient compliance, and shared decision-making (Conrad 1985; Trostle et al. 1983; De Ridder 1997; Charles 1997; Hayes-Bautista 1976, 1978). Despite this, little consensus exists on the causes of noncompliance (Donovan and Blake 1992; Morris and Schultz 1992), and little attention has centered on noncompliance in relation to medical pluralism—, that is, the belief in and use of a variety of treatment modalities (see Fadiman 1997; Schwartz et al. 1997). This article examines the issue of compliance from the perspective of both the consumer of services and the medical professional.
RESEARCH DESING AND METHODS
Collecting the Data: Key Informants
The study used ethnographic data-collection and analysis techniques, with the intention of formulating an inductive hypothesis-generating study. One objective was to examine some of the similarities and differences in philosophy and treatment modalities for various care providers of asthmatic children in Tijuana. Understanding these philosophical underpinnings is essential for analyzing the cultural construction of medical compliance. Data gathering took place between October 1996 and October 1998. Open-ended, information-gathering interviews were initially conducted with key community informants: the chief of pediatrics, staff pediatricians, and interns at the Hospital Local; administrators of La Clínica;1 local epidemiologists; a community-outreach social worker/nurse; and a small sample of parents whose children had been experiencing chronic "respirator problems" but who had not sought medical treatment. A local field assistant helped to recruit private practitioners (both generalists and asthma specialists) and pharmacists who treat asthmatic children for a one-time, open-ended interview lasting approximately one hour. Over its two-year course, the study employed a triangulation method, involving in-depth interviews (including illness narratives), participant-observation, and structured assessment tools.
Fifteen mothers, whose children were between the ages of one and 13 and medically diagnosed as having asthma, volunteered to participate in this study. We recruited families through clinic observations in the Hospital Local or the asthma clinic at La Clínica. Twelve of these families were in various stages of treatment at La Clínica, ranging from the first visit to being referred to a general pediatrician for follow-up visits.
Prior to the family-member interviews, key community members were interviewed. Depending on an informant's background, semi-structured interviews focused on one or more themes: incidence/prevalence of childhood asthma in Tijuana; type and availability of community services; practitioner's perceptions of parental care-taking behaviors (that is, what practitioners thought parents were doing to manage their child's illness, and whether they thought this care was appropriate); use of antibiotics, over-the-counter medications, injections, and reactions to these medications, including antibiotic resistance; and the effect of economics and education on the ability of the parents to care for their children in times of illness. Interviewees were allowed to lead the discussion along the lines of their own interests and knowledge. This made for rich and diverse data. A number of practitioners wanted to discuss health policy and the need for change, especially regarding the distribution of over-the-counter antibiotics.
Clinic Observations and Practitioner interviews
Approximately four hundred hours of clinic observations took place in the offices of two pediatric asthma specialists of La Clínica. These observations involved more than 1000 physician-patient observations (including return visits). Interviews were tape-recorded with permission of the physician and adult members of the family. In-depth, semi-structured interviews were held with the two asthma specialists and a pediatric pulmonologist in La Clínica, as well as with general physicians, and with physicians who prescribe natural remedies and are not associated with La Clínica.
Household Interviews
H. Russell Bernard (2000:192) recommends using a non-random sample of respondents when trying to gain information about the experiences of individuals. Additionally, he recommends the use of four or five key informants to test whether a majority in a population is likely to have substantially the same culture as that an initial key informant describes. Caretaker interviews, averaging 1.5 to 2 hours, were conducted in the home, clinic, or unrelated location (such as a restaurant) according to the interviewee's wishes. With participants' permission, interviews were recorded on audiotape. All questions were open ended and based on the following themes: definition, prevention, and management of asthma (including crisis and routine care); illness history; choice of medical facilities and access to health care; use of over-the-counter medications, home remedies, and antibiotics; cost of management, including doctor's fees, medication, and time lost from work and school; and the effect of the illness on the caretaker and other family members. Close ties were built with five mothers, whose cases were followed in greater detail than the others. These informants were referred by the specialists at La Clínica or chosen because they appeared to have rich data to share. In order to observe interactions between mothers and those offering treatment and advice, mothers were accompanied on clinic, pharmacy, herbalist, neighbor, and corner store visits when feasible. In some instances, it was the grandmother or other family member who provided or assisted in the care of the child. At each visit, the mother or caretaker was interviewed and asked about illness episodes since the last visit.
Compliance or Inclusion? The Lay Versus Professional Model
Integrative knowledge and practice, based on experience, availability, and affordability, is the backbone of medical treatment within the family. With its mixture of borderland pharmacies, homeopathic stores, botanicas, and biomedical practitioners, Tijuana provides a perfect setting for families to integrate biomedical and "local knowledge" practices (Geertz 1983). By simultaneously seeking care from physicians practicing Western medicine, traditional healers, and storefront or sidewalk clerks, family members bypass the traditional "hierarchy of resort" (Romanucci-Ross 1969), practicing instead a pluralistic "resort of inclusion." What medical anthropologists have coined "medical pluralism" (see Schwartz 2001) practitioners may view as noncompliance. The concept of noncompliance and a wish that patients not employ simultaneous medical systems is not limited to physicians practicing Western medicine. In this study, practitioners of natural health care also expressed a wish that their patients would follow one medical system rather than employing multiple systems. Some went as far as to say that Western biomedical medicine harms their patients. Despite the lay community's pluralistic approach to medicine, interaction between the various professional sectors providing treatment of childhood asthma is limited and may be contributing to patients not following the wishes of the professionals.
How, then, does the medical community define noncompliance? Is there one definition? Or does it vary by provider—or possibly even by patient? Norman Fineman (1991:354-5) argues that "meanings of noncompliance are subjectively constructed by providers just as they are by patients." He notes that "despite increasing interest in the subject of noncompliance, virtually no research focuses upon health care providers subjective understandings of it. No research, in other words, examines the ways in which providers subjectively construct, define, and interpret their patients' noncompliant behaviors." I would argue further that noncompliance is culturally constructed and begs the question of a clearer definition of the boundaries of Western biomedicine. Must medications be physician-prescribed in order to fit within the domain of biomedicine? Or would a medication (and therefore the person purchasing it) fit within the domain if the medication were "recommended" by a pharmacist with a grade-school education who was trained on the job—as is often the case in Mexico? Is a patient being "noncompliant" by following the recommendations of the pharmacist to purchase a less expensive medication—as is also often the case in Mexico? In other words, where does noncompliance begin, and with what system of medicine are patients not complying?
In an interview, a pediatric asthma specialist mentioned that most of his patients get better soon after they begin his care, but some do not. When asked why, he replied simply, "noncompliance." In his estimation, 5% to 10% of his patients are what he would call "noncompliant." I examine here the issue of noncompliance from the perspective of two pediatric asthma specialists, whom I have labeled Dr. #1 and Dr. #2, and then I explore the subjective experiences of mothers of chronically ill children, who these physicians consider to be "noncompliant." Table 1 encapsulates the definitions of "compliance" according to these two specialists. The emergence of a subjective definition of compliance quickly becomes evident. While both physicians agree on two conditions of compliance: 1) showing up for scheduled appointments, and 2) following through with the purchase and administration of medications, they do not agree on how much the patient should rely on the specialist, nor on whether home remedies should be administered.

The degree of importance placed on compliance varied by physician, as well. Dr. #1 believes the following:
It's important that mothers comply. Mothers whose children have severe asthma have a better understanding than mothers of children with moderate asthma. They don't always understand that asthma can be life threatening.
Both physicians agree that the economic situation in Mexico is a major factor contributing to patients' noncompliance. Dr. #1 sees more noncompliance at the clinic than he does in his private practice. He attributes this to differences in economic resources as well as lack of general education. Dr. #1 places more emphasis on compliance than does Dr. #2, claiming that he will do "anything in [his] power to make a patient comply," including cajoling patients or feigning anger. When discussing compliance, Dr. #1 claims to "know my tricks." When all else fails, he has no compunction about "pushing" his patients to comply with his wishes. In summation, he applies the following simple but effective philosophy when dealing with noncompliant patients: "Get them to do what you want."
Dr. #1's approach might seem somewhat contrary to the outside observer, but his patients do not appear to be offended. Taking what might be called a "proactive-personal" approach, or one that is solution oriented, he tells jokes and may feign anger, but he rarely blames the patient directly. The objective is to transform the perspective of the parent to do what the physician considers is in the best interest of the child. In return, the patients express their confidence in "el especialista." Expressing confidence in and complying with the recommendations of the physician, however, are separate issues.
The sub specialists concur that they prefer working with difficult-to-treat patients because they are more interesting, and they present a challenge to the physician. Says Dr. #1: "these patients come to us because no one else wants to deal with them." Dr. #2, who has been in practice slightly longer than Dr. #1 expects and requires less of his patients: "When I started, I wanted to do everything... At first, I was upset when people broke the rules. Now I accept it. I can't change it." In his view, rules are "broken like crystal... People here procrastinate. They don't have preventive check-ups like in the U.S. There is no discipline because of low education..." Rather than blaming the individual, he sees the educational system as a culprit. Other physicians agree and hold lack of education in Mexico responsible for child health problems:
They have troubles. And these are the people who take their children to health centers for medical care, which sometimes is palliative and not enough. They are low-income people, with little education, who do not follow medical directions properly and who do not pay enough attention to the matter. With regard to children, an adult usually says that he or she has recovered just because the child had a medical consultation. After a while, when the parent does not follow through or forgets to continue the treatment or medication, the condition returns. Then, confronted with a new crisis or an even worse respiratory condition, the child is taken to the health center once again. Afterwards, the parents forget or do not continue with the treatment and the cycle] starts all over again... this reflects their lack of medical education.
General Practitioner (Author's Translation from the Spanish)
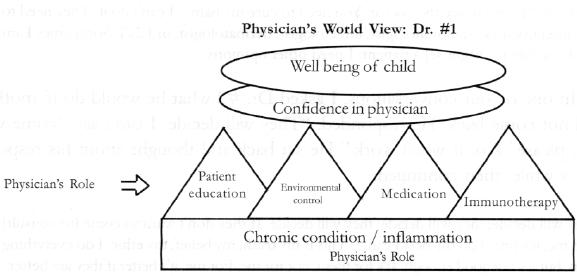
The list of criteria shows that the two asthma specialists have slightly different definitions of "compliance." They also seem to have different concepts of their role as asthma specialists. Dr. #1's main medical objective is to fight inflammation. In order to do that, he uses "everything I've got in my power to try," including a fourfold approach based on education, medication, environmental control, and immunotherapy. In Dr. #1's estimation, these four aspects, when administered properly, can build confidence in the physician and can control the child's asthma—IF the family does its part.
Dr. #2, whose main objective is to "fight infection," describes himself as having "limitations as a doctor." For Dr. #1, one form of noncompliance consists of patients breaking scheduled appointments and not returning for months at a time. One way of dealing with this is to tell patients that he won't see them if they don't show up for their scheduled appointments. When one woman did not return for over 10 months, he made a "deal" with her: If she won't see him, he won't see her. Both physicians volunteer their time at this clinic and both have expressed their frustration with patients "wasting" their time as specialists: "They don't pay me," said Dr. #2 when one child returned sick to the clinic without having seen his regular pediatrician. "It takes too much time to see these people."
For Dr. #2 "noncompliance" has more to do with over-dependency than with not returning for follow-up appointments. "You have limitations as a doctor... They think you are God; they expect you to solve all of their problems. But your doctor has a life, too, and limitations. You want the patient to help. Don't come here sick. Go to the doctor for follow-up. We need to fight together with the disease. It is too much responsibility to do it alone." In contrast to Dr. #1, Dr. #2 is concerned about patients corning to his clinic too often and relying too much on him as a specialist. Specialty clinic visits may be weeks or months apart and are terminated when the child's symptoms are stabilized. Dr. #2 insists that patients have follow-up care with general pediatricians or other specialists, including those at the clinic, while patients prefer the services of the asthma specialists. Says one mother:
There is a big difference because it is the form in which [the physicians] receive the children, how they attend them. They attend the children with affection (con cariño)... And each child is important. There are no differences; they don't treat some well and others poorly; all are treated well. They were very interested when the child was sick. 1 became desperate because I did not have what I needed. Sometimes they helped me with the medicine. When he was very sick, they helped me obtain the apparatus for oxygen and all. This counts for a lot. The help that one receives is important. (Author's translation from the Spanish.)
Dr. #2 wants his patients to develop a greater sense of autonomy, however, especially for emergency situations:
They just come here on [my clinic days]; they need to be seeing a regular pediatrician. If I tell a mother to come here whenever she wants, she'll come every week. I need them to follow-up [with other physicians and in between appointments].
I asked why it was important that parents see other physicians if they have confidence in him:
When I started, I wanted to do everything... But for me to try to do everything is wrong... It's important to refer. I need to share... Some mothers have [psychological] "problems." they say, "I need to see the doctor. You need to cure my baby." I can't do it. They need to see other doctors—pulmonologist, infectologist, dermatologist, or ENT. Sometimes I am stuck [unable to diagnose] a patient; I need other opinions.
In one of our conversations, I asked Dr. #2 what he would do if mothers did not come back. He responded: "They will decide. I can't say 'come with me, please.' No. It won't work." He sat back and thought about his response for a while, then continued:
They will decide; they will decide; they will decide. If they don't want to come [to consult] with me, it's fine. I do the best I can... This is my truth, my belief, my ethic. 1 do everything I can, but it's not good enough. It's for them, not for me. For me, it's better if they are better.
Yet, he, too, gets upset when parents do not show up for their appointments. In one instance, a mother did not come to the clinic for six months because she perceived her child to be doing well. Dr. #2, however, believes this child has hyperactive lung functioning and chronic respiratory infections as well as being at high risk for acute asthma attacks. He wanted this child to be monitored on a monthly basis and now refers him to the pulmonologist for complications.
Physician's Worldview
Figure 1 is a representation of a pediatric asthma specialist's worldview, or what he expects, or at least wishes, to happen. Figure 2 is a hypothetical representation of care-seeking behaviors of families in Tijuana with asthmatic children. Many, if not most, families seek help from more than one physician; they seek assistance from pharmacies and neighbors; and they mix herbal or naturalistic medicine with Western biomedical medication. The specialist's expectations of the patient and the patient's care-seeking behavior exhibit relatively little overlap. An exception is the patient who visits the Clínica, follows the specialist's advice, and does not return to the original care-seeking pattern. Often, these are the children whose symptoms arminish, and who, after a certain amount of time, no longer require specialized care.

Education for asthma treatment generally takes place on two levels: private consultations and monthly patient-education seminars. Within the clinic, education most often consists of teaching parents how to administer medications, particularly bronchodilators. Dr. #1 is fastidious teaching mothers how to use bronchodilators. Often in these consultations, a fine line exists between patient education and the coaxing of patients these physicians consider "noncompliant." As an example, Dr. #1 shows a mother that dust collects under things and must be removed. In the same consultation, the mother admits that her four-year-old son does not like taking his medication. Dr. #1 counsels her that she has to give the child a choice: If the child wants to watch television, he has to take his medicine. He then demonstrates to the mother how to administer Ventolin and gives her an informational handout. He wants the parents to treat their children the same way he treats the patients: "If you want your reward [a healthy child/the privilege to watch television], you need to cooperate with me."
Dr. #1 believes that herbal teas lower the child's iron levels and he does not want parents to administer them. Dr. #2 disagrees and often recommends the use of chamomile tea for cleansing the child's sinuses. A private pediatrician, who owns a pharmacy in the popular shopping area known as the Cinco y Diez, recommends the use of herbal teas because it increases the child's water intake, which all three doctors agree is important for these children. Dr. #1 can be considered the strongest proponent of Western biomedicine. Both the private physician and Dr. #2 are more accepting of herbal medicine, and they do not view its use exactly as "noncompliance."
Rather, they appear to have adopted the role of practicante, as described by James Young: someone "able to incorporate scientific medical remedies, which in many cases are considered faster acting than herbal remedies, without necessarily contradicting local conceptions of illness causation and process" (1981:121).
The Patient's Perspective
The previous section revealed both overlap and differences in how physicians expect their patients to comply with their wishes. The next section examines the perspective of "noncompliant" patients. The following vignettes provide background about why patients may not comply with the wishes of their physicians (see also Table 2).
Vignette 1
When I began interviewing her, Inez and her daughter, Laura, had been seeing Dr. #2. Inez did not want me to visit her house, so the following week, we met at the local Burger King, located in the center of the Cinco y Diez, the bus exchange and hub of shopping for lower-middle-class families residing in Tijuana. Inez arrived half-an-hour late, with a very unhappy daughter in tow. Laura had been up all night with an earache and had cotton soaked in warm oil in her ear. Inez had no intention of visiting a doctor; she expected the cotton to help by keeping out the wind. Because 1 was going to the clinic that day, I suggested that they come with me. Laura was crying and obviously in distress.2 Inez first had to get permission from her husband, which she was reluctant to do. As we drove to the factory where he was a supervisor, Inez told me about the affair he was having with one of the workers. She was torn between her shame at entering the factory and the urgency of her daughter's need for medical attention. In the middle of the situation were a supportive shoulder (mine), a car, and some extra cash (also mine). The decision to enter the factory and confront her husband (and possibly his lover) to ask for permission to take her daughter to a doctor and to request funding to purchase medications was hers alone.
When we entered the clinic, Dr. #2 was not on duty, so Dr. #1 examined Laura on an emergency basis. In order to avoid a conflict of interest, he agreed to see the child this time if Inez would agree to continue follow-up visits with him rather than with Dr. #2, her assigned physician. Had Inez waited another few days, he explained, Laura might have lost her hearing.
The mother and daughter returned once, but then they stopped coming. A few months later—having run out of medication for Laura's chronic asthmatic condition—they returned. They had missed three appointments, and Laura was not doing well nor had she been doing well in Acapulco, where they had spent the past few months with her father's family. On this visit, Dr. #1 asked Inez to show him Laura's medications, as he does with all of his patients. Inez produced two bronchodilators and one bottle of drops. One of the broncho-dilators was empty; Laura had been using it since her visit many months before, and Inez had not renewed the prescription. Laura's nose and ears were all right, but she had been wheezing. Obviously upset, Dr. #1 turned and said to me, "She has enough money to go to Acapulco, but not enough to bring her daughter to the doctor." He then explained to Inez that "running out of medication is like putting a plastic bag over your daughter's head."
In our informal meeting afterwards, Dr. #1 explained that "this is a problem of noncompliance. Sometimes it's due to economics." He explained tha the feigns anger at mothers for not complying with his wishes, even though he is "really not angry":
It's cultural; it's a way to get them to respond. Sometimes women cry. I don't care what I have to do. If a child dies from this illness because the mother didn't comply, I can be held responsible. It's important that mothers comply. [Original English]
After Laura started recovering, I spent an afternoon with her and Inez visiting pharmacies and a homeopathy store. I also followed up with an extensive interview, during which Inez discussed her husband's abuse towards her, her own feelings of inadequacy as a wife and mother, and her intense loneliness. She had moved to Mexico from Honduras on her own, and had no familial or social support. Inez was gaining weight rapidly and had tried committing suicide a few weeks prior to my interview with her. Her husband's family resides in Acapulco, and she felt that she had had no choice but to go with him to visit for the Christmas holidays. At the time that I interviewed her, Inez was as concerned about her own mental health and weight problem as about her daughter's asthma. From her point of view, her options were to stay in Tijuana, and attend her daughter's scheduled clinic appointments, or submit to her husband's wishes that she and Laura go with him to Acapulco. Neither she nor her husband had thought of requesting extra medication to take with them, nor had they discussed seeing a physician while on vacation. Considering that it did not occur to her to take Laura to a doctor on an emergency basis, it is not surprising that the concept of preventive health care was foreign to Inez. Being without familial support contributed to Inez' stress. She chose the path of least resistance: She waited until she could return to the clinic in Tijuana to seek further medical care for her daughter.
Dr. #1 used his bag of tricks —including feigning anger at her — to get Inez to comply with his wishes. He also spent extra time outside of the clinic answering her questions and explaining more about her daughter's condition. For Dr. #1, compliance is imperative to treatment; it is the patient's role to comply, but his responsibility to assure this compliance. Inez, however, confided in me afterwards that she did not understand what it was that he was trying to explain to her. She asked me to explain it in simpler terms.
Vignette 2
Many, if not most, mothers studied at La Clínica have seen at least three other physicians before attending the asthma clinic; at least one has seen as many as 10 physicians. Mothers complain that physicians over-prescribe antibiotics, which "break down the defenses" and affects the "red blood cells." Rebeca, the mother of one of Dr. #2's patients, had stopped giving her son antibiotics after seven days, even though Dr. #2 had prescribed a 15-day course. She did not discuss this with him, but confided in me afterwards. Rebecca did not understand why her son had been prescribed an extended course of antibiotics, and instead of discussing this with her physician, she discontinued giving the prescribed medication for fear that it would do him more harm than good.
Vignette 3
Eighteen-year-old Barbara is another mother who might be considered noncompliant. A native of Tijuana, she lives with her son, Juan, her husband, and their extended family on a large piece of property in Los Reyes. The family owns a grocery store behind which they live. Barbara attended school for 10 years; her husband for five. Like most of the families in this study, Barbara's lives on a dirt road—which means that there is plenty of dust. Eighteen-month-old Juan is chronically ill with chillidos (wheezing) and ojo (evil eye), each of which, from Barbara's perspective, requires a different system of treatment. In addition, Juan has had chronic infections since he was three-months old. He had seen seven physicians for his wheezing and had had a "cleansing" for ojo three months before I began to interview her. Although she claimed to have been very worried about his health since then, Barbara now considers Juan to be "cured" and believes that for the time being, he does not need to be taking the medicine that was prescribed for him at La Clínica.
Barbara has experimented with a variety of treatments, including home remedies (honey and lemon, oregano tea, and fish oils) and medications the seven different doctors had prescribed during approximately 15 months. She claim that each prescribed a different medication, none of which worked in the long run:
We brought him to a pediatrician here, and we returned a week later, but the child continued the same. We returned, and we brought the child back, and [the doctor] told me to come back in 5 days and the baby was already a little better. The infection was gone, but it returned a month later. He continued with the problem, and it became more and more frequent. It began with a cough, a dry cough, and then he began to wheeze. And so we took him to the doctor, and he gave him injections.
After that, Barbara switched doctors:
Barbara: I gave him medications for 15 days.
Interviewer: Did this help?
Barbara: Well, it helped, but it lasted for 15 days and that was it. The symptoms were gone [se le retiró] for the 15 days that he was given medication. They were gone, but then they returned...
Interviewer: Did you return to the same doctor?
Barbara: We did not return to the same one.
Interviewer: Why not?
Barbara: I wanted to, but it was Saturday and the doctor had gone to a consultation in San Diego. So we brought [Juan] to another doctor, and this doctor, another time, gave him another medication. By now, this child had been given every type of medication. I don't have the prescriptions at hand, but I have them like this [makes gesture of holding something]. A stack of prescriptions from so many times that I took him.
Interviewer: To different doctors?...
Barbara: Uh huh. To seven different doctors, and each one gave seven different things; different medications.
Interviewer: Do you remember what they were?
Barbara: Well, they gave me Amoxil, Amoxibron, Keflex.
Interviewer: What is Keflex?
Barbara: It is also an antibiotic suspension for infection. And they gave him Aumentin.
Interviewer: Is this also an antibiotic?
Barbara: Uh huh, injections. They also gave him injections, for example Decadron, Penprocilina... All are antibiotics. The first time that I brought him to La Clínica, [the pediatrician] was frightened. This child is bombarded with so much, and she was frightened. She said that he is so small, how is this possible, all of this; that he was given so much, so much medication. Because of this he has lowered red blood cells; because of so much medication.
Barbara continued with her litany of infections and medications. At one point, I said:
Interviewer: He has a lot of medication.
Barbara: Oh, yes; enough. They gave him everything; especially, they gave him a lot of Garamicina It is an injection called Garamicina.
Interviewer: Garamicina. What is this?
Barbara: It is when the child had a lot of coughing, and I brought him and they gave him the Garamicina, and he got better, but ultimately not. Now 1 don't do it, but they always gave it to him; all the time.
Juan has been doing well with teas prepared from Barbara's backyard and street—eucalyptus, "tabachin," mullein, and one other ingredient that she does not remember. She believes that as long as Juan is doing well, he does not need to be taking prescribed medications. Barbara practices pluralistic medicine by applying home remedies in a preventative manner, and Western biomedicine in a curative manner—which, by the criteria described above, makes her noncompliant with Dr. #1's requirements, but not with those of Dr. #2.
Vignette 4
Adele's 13-year-old son had been diagnosed with asthma by a specialist at La Clínica and was prescribed a bronchodilator, as well as a number of medications to take on a regular basis. When her niece started exhibiting symptoms similar to those of her son, Adela shared his medication with the girl. Like Barbara, Adela felt that it was important to treat the symptoms, though she had little understanding of the underlying causes. While she was in compliance with "following through with purchasing and administering prescribed medication" to her own son, she did not see the danger n administering the same medication to her niece. Like the mothers described in the other vignettes, she had confidence in the especialistas of La Clínica, but did not discuss some of her treatment choices with them.
Concluding Remarks
Why do patients not comply with their physician's wishes? Both the physicians this article describes are respected, by patients and peers alike, as among the best qualified subspecialists in Baja California. They have extensive training in the United States and Mexico, and they are both extremely aware of the cultural practices that their patients follow. Because these physicians are experts in their field, patients wait for months to see them. Some patients travel for many hours by bus just to attend the clinic. All of the physicians interviewed are deeply aware and respectful of the cultural, as well as economic, impediments to child health care in Mexico. Yet, they still believe that patients are not complying with their wishes as physicians—rather than holding the view that the patients are simply earning out behaviors, which have been culturally ingrained over centuries. These include the common practice of employing local knowledge on healing as well as pluralistic medical systems.
Rebeca was brought up with the widespread Mexican understanding that too many antibiotics reduce one's "defenses." After experiencing that antibiotics did not control her child's asthma, should she have been expected to administer antibiotics for yet another 15 days? When one can go to a pharmacy to purchase bronchodilators without a prescription, as well as most other medications, why is it illogical for someone like Adela to offer her niece her son's medication? After all, they are experiencing the same symptoms; why not apply the same medication? Given that the sale of pharmaceutical medications is not regulated in Mexico, who is responsible for deciding when it is necessary to visit a physician to get his or her approval for taking a medication? When it is culturally ingrained (and in some cases empirically provable) that it is more economical to purchase medications at the corner pharmacy, why make an extra trip to the doctor?
Thus the question comes down to: With whom is one complying or not complying? In Inez' situation, she was overcome with suicidal depression and, for a number of reasons, felt that following her husband's orders was more important than following those of her physician. While she was very attached to her daughter and concerned about the girl's health, Inez did not see herself in a position of power or control.
Barbara, on the other hand, was in an equitable marriage, but as long as her son's condition was stable, she preferred to use her situated knowledge as well as locally grown medicinal plants in place of long-term Western biomedical treatment. She lives with her family and is confident about the information that had been passed down to her through her family; but she was confused about the use of biomedications, especially since the prescriptions were constantly changing. As this article has revealed, some physicians, but not others, would consider Barbara noncompliant because of her utilization of her knowledge of herbal medicine.
This article examined medical noncompliance as defined by two subspecialty pediatricians volunteering their time to treat children with chronic asthma. In addition, the issue of noncompliance was explored within a cultural context from the perspective of the patient. Children in this study, for the most part, were progressing in their treatment programs. Parents showed great respect for, and confidence in, the "especialista" physicians associated with La Clínica. Despite this, physicians and patients have different medical worldviews and view compliance differently. As one medical researcher on the treatment of childhood asthma notes:
The competing goals of the pharmacological management of asthma—those of biomedical science compared to those of the family—need to be placed within the framework of concordance where patients become partners in their medical care and medicine use. This implies that the physician must step out of the role of commander-in-chief and begin to play the role of "guide" in a discovery trip... [A] chronic disease such as asthma must, in the final analysis, be "commanded" by the individual (Sanz 1999: 8).
Health care in Mexico is not neatly packaged, nor is it based on a single medical model. Western biomedicine may be the predominant medical system —some would say the hegemonic system-but it is far from the only system. What physicians view as "noncompliance," might be deemed by patients as "coping with reality" and by anthropologists as employing "local knowledge." However, there is a dark side to all of this. There can be a dangerous reality and an outcome based on lack of knowledge if no guidance is provided at all. Barbara's local knowledge of herbal remedies may (or may not) be sound by ethnoscientific standards. But how sound are overlapping medical systems that exist within a void of communication? This article reveals patients withholding medications, mixing types of medications, switching doctors, and sharing medications based on symptoms rather than clinical examinations. It also revealed inconsistencies among general practitioners in how they treat childhood asthma. I hope that this information can be used to stimulate discussion on how to establish communication not only between patient and physician but also between and among the various types of practitioners providing care to children with asthma and other illnesses.
Acknowledgments: The Fulbright-García Robles Foundation, U.C.-MEXUS, Berkeley Center for Independent Living, and El Colegio de la Frontera Norte funded this research. The author wishes to thank Drs. Yewoubdar Beyene, Joan Ablon, Duane Metzger, and three anonymous readers for their comments on earlier drafts of this article.
REFERENCES
Adams, Stephanie, Roisin Pill, and Alan Jones. 1997. "Medication, Chronic Illness and Identity: The Perspective of People With Asthma." Social Science Medicine 45 (2):189-201. [ Links ]
Anderson, H. R., B. K Butland, and D. P. Strachan. 1994. 'Trends in Prevalence and Severity of Childhood Asthma." British Medical Journal 308 (6944):1600-644. [ Links ]
Bernard, H. Russell. 2000. Social Research Methods: Qualitative and Quantitative Approaches. Thousand Oaks, California: Sage Publications. [ Links ]
Conrad, Peter. 1985. "The Noncompliant Patient in Search of Autonomy." Hastings Center Report 17:15-17. [ Links ]
Charles, Cathy, Amiran Gafni, and Tim Whelan. 1997. "Shared Decision-Making in the Medical Encounter: What Does It Mean? (Or It Takes At Least Two to Tango)." Social Science and Medicine 44 (5):681-92. [ Links ]
Christiansen, Sandra C, Stephen Martin, Nina Schleicher, James Koziol, Kenneth Mathews, and Bruce Zuraw. 1996. "Current Prevalence of Asthma-Related Symptoms in San Diego's Predominantly Hispanic Inner-City Children." Journal of Asthma 33 (l):17-26. [ Links ]
De Ridder, Denise, Marja Depla, Peter Severens, and Marijke Malsch. 1997. "Beliefs on Coping with Illness: A Consumer's Perspective." Social Science and Medicine 44 (5): 553-59. [ Links ]
Donovan, J. L., and D. R. Blake. 1992. "Patient Noncompliance: Deviance or Reasoned Decision Making?" Social Science and Medicine 34 (5):507-13. [ Links ]
English, Paul, Juke Von Behren, Martha Harnly, and Raymond Neutra. 1998. "Childhood Asthma Along the United States/Mexico Border: Hospitalizations and Air Quality in Two California Counties." Revista panamericana de salud publica/Pan American Journal of Public Health 3 (6):392-98. [ Links ]
----------, and Norah Schwartz. 2000. "Childhood Asthma at the California/Baja California Border." Paper presented at committee meetings in El Centro, California. July 10-11, 2000. [ Links ]
Fadiman, Anne. 1997. The Spirit Catches You and You Fall Down. New York: Farrar, Straus and Giroux. [ Links ]
Fineman, Norman. 1991. "The Social Construction of Noncompliance: A Study of Health Care and Social Service Providers in Everyday Practice." Sociology of Health and Illness 13 (3):354-72. [ Links ]
Frcnk, Julio. 1991. "The Epidemiologic Transition in Latin America." Boletín de la Oficina Sanitaria Panamericana 111 (6): 485-96. [ Links ]
Geertz, Clifford. 1983. Local Knowledge: Further Essays in Interpretive Anthropology. New York: Basic Books. [ Links ]
Hayes-Bautista, David E. 1976. ''Modifying the Treatment: Patient Compliance, Patient Control and Medical Care." Social Science and Medicine 10:233-38. [ Links ]
----------, 1978. "Chicano Patients and Medical Practitioners: A Sociology of Knowledges Paradigm of Lay-Professional Interaction." Social Science and Medicine 12:83-90. [ Links ]
Jones, A. 1994. "Screening for Asthma in Children." British journal of General Practice 44 (381):179-83. [ Links ]
Leowski, R. W. 1986. "Mortality from Acute Respiratory Infections in Children Under Five Years of Age: Global Estimates." World Health Statistical Quarterly 39:138-44. [ Links ]
Morris, Lisa Stockwell, and R. M. Shultz. 1992. "Patient Compliance—An Overview." Journal of Clinical Pharmacy and Therapeutics 17:283-95. [ Links ]
Omran, Abdel R. 1983. "The Epidemiologic Transition Theory: A Preliminary Update." Journal of Tropical Pediatrics 29:305-16. [ Links ]
Phelan, P. D. 1994. "Asthma in Children: Epidemiology." British Medical Journal 308: 1584-585. [ Links ]
Risser A. L., and L. J. Mazur. 1995. Archives of Pediatric Adolescent Medicine 149 (9):978-81. [ Links ]
Romanucci-Ross, Lola. 1969. "The Hierarchy of Resort in Curative Practices: The Admiralty Islands, Melanasia." Journal of Health and Sodal Behavior 10:201-9. [ Links ]
Rubel, Arthur. 1960. "Concepts of Disease in Mexican-American Culture." American Anthropologist 62 (5):795-814. [ Links ]
Salas-Ramirez, Maribel, Nora Hilda Segura Méndez, and Salvador Martínez-Cairo Cueto. 1994. "Tendencia de la mortalidad por asma en México." Boletín de la Oficina Sanitaria Panamericana 116 (4):298-306. [ Links ]
Sanz, Emilio. 1999. "Pharmacological Treatment for Asthma: Disease, Diagnosis, Drugs and Patients." EuroAsthma Forum 5:4-9. [ Links ]
Schwartz, Norah. 2001. "Siento Que Me Ahogo: Childhood Asthma, Medical Pluralism, and the Mexican Frontier." Doctoral dissertation. University of California, San Francisco and Berkeley. [ Links ]
----------, Sylvia Guendelman, and Paul English. 1997. "Thermometer Use Among Mexican Immigrant Mothers in California." Social Science and Medicine 45 (9):1315-23. [ Links ]
Secretaría de Salud de Baja California. 1996. "Casos acumulados de enfermedades de notificación semanal en orden de incidencia reportada: Baja California 1995." Mexicali: Secretaria de Salud de Baja California. [ Links ]
Sistema Nacional de Vigilancia Epidemiológica. 2000. "Observaciones sobre aumentos recientes en la mortalidad debida al asma." Epidemiología 36 (17): 1-3. [ Links ]
Trostle, James A., Alian Hausser, and Ida S. Susser. 1983. "The Logic of Noncompliance: Management of Epilepsy From the Patients Point of View." Culture, Medicine and Psychiatry 7:35-56. [ Links ]
Trotter, Robert, and Juan Antonio Chavira. 1981. Curanderismo: Mexican American Folk Healing. Athens: University of Georgia Press. [ Links ]
U.S. Department of Health and Human Services. 1991. Allergic Diseases, NIH Publication No. 91-3221. Bethesda, Maryland: Office of Clinical Center Communications, National Institutes of Health. [ Links ]
Van Ganse, E., H. G. M. Leufkens, W Vincken, I. Hubloue, P. Bartsch, A. Bouckaert, and P. Ernst. 1997. "Assessing Asthma Management from Interviews of Patients and Family Physicians." Journal of Asthma 34 (3): 203-9. [ Links ]
Von Behren, Julie, Richard Kreutzer, and Daniel Smith. 1999. "Asthma Hospitalization Trends in California, 1983-1996." Journal of Asthma 36 (7):575-82. [ Links ]
World Health Organization. 1992. Acute Respiratory Infections in the Americas: Magnitude, Trends, and Advances in Control. Pan American Health Organisation. HPM/ARI/02-92. Washington: World Health Organization. [ Links ]
Young, James. 1981. Medical Choice in a Mexican Village. New Brunswick, New Jersey: Rutgers University Press. [ Links ]
Zayas, L. E., C. R. Jaen, M. Kane. 1999. "Exploring Lay Definitions of Asthma and Interpersonal Barriers to Care in a Predominantly Puerto Rican Inner-City Community." Journal of Asthma 36 (6):527-37. [ Links ]
1 I have used pseudonyms for the names of these two health-care facilities.
2 For ethical and professional reasons, I normally do not involve myself in the medical practices of study participants. However, I believe it would have been unethical not to address Laura's need for immediate care.














