INTRODUCTION
The pandemic intensified a range of social and health problems (WHO, 2022; Edward & Mobarak, 2022), particularly affecting women (Burki, 2020). According to experts, unmet needs for contraceptives and safe abortion, lack of reproductive health programs, domestic sexual violence, poverty, and school dropout rates rose during the pandemic (NU - ECLAC, 2020; Borg Xuereb et al., 2023), contributing to the increase in the adolescent fertility rate (NU - ECLAC, 2020), which rose by 30% in Mexico (UNFPA, 2023).
Adolescents who experienced pregnancy and motherhood during the pandemic were forced to cope with adversity and intense emotions; fear of having loved ones with COVID-19, stress due to unemployment and financial difficulties (Astle et al., 2021; Smiley et al., 2021; Merriman et al., 2023), and uncertainty due to changes in their prenatal care and birth plans (Astle et al., 2021; Moltrecht et al., 2022). Many reported feeling unprepared to stimulate their children’s development because they had been unable to take advantage of prenatal classes and contact with adults who would otherwise have provided guidance (Moltrecht et al., 2022).
Some adolescents reported feeling depressed due to the strict lockdown they observed out of fear of the unknown consequences of COVID-19 on pre-existing medical conditions, their pregnancy, or their newborns. Conversely, those who interrupted social distancing to receive support from their families reported experiencing anxiety and guilt (Moltrecht et al., 2022; Merriman et al., 2023). Adolescent mothers who parented their babies without support from their extended families and or partners—who were usually the providers—experienced constant frustration (Merriman et al., 2023). Those who continued their studies during the pandemic found it overwhelming to balance them with motherhood. Many were forced to interrupt or drop out of their studies because they lacked support to care for their children (Smiley et al., 2021).
In 2020, the adversities and intense emotions caused by the pandemic were expected to contribute to mental health problems (Shigemura et al., 2020), and a recent meta-review showed that depression and anxiety increased in adolescents, pregnant and postpartum women and people hospitalized with COVID-19 (Bower et al., 2023). Three research projects were found on the mental health of adolescent mothers during the pandemic. The first reported lower parental stress and postpartum depression (PPD) during the pandemic than before it started, attributed to a life skills program (LSP) and continuous school contact (Astle et al., 2021). The second research project reported a low level of PPD associated with good family support in two groups of adolescent mothers: under lockdown vs. not under lockdown (Matei et al., 2021), while the third found a higher proportion of PPD and lower social support among adolescent than adult mothers in the group (Sangsawang & Sangsawang, 2023).
These research projects during the pandemic coincide with studies prior to this one showing that adolescent and adult mothers who receive adequate postpartum support are less likely to experience PPD and that the protective effect is greater for adolescents (deCastro et al., 2011; Kim et al., 2014).
Self-esteem and confidence in one’s ability to solve problems—associated with parenting or otherwise—increases the use of effective coping strategies, maintaining hope and commitment under challenging circumstances (Bandura, 1994; Lazarus & Folkman, 1987). These characteristics can play an important role in coping with the stressors of motherhood, the pandemic, or both. Research on adolescent mothers reports that low self-esteem (Birkeland et al., 2005; Ramos-Marcuse et al., 2009) and a negative perception of their own abilities to foster the development of infants and overcome parenting difficulties—low perception of maternal efficacy —are associated with PPD (Lara et al., 2017; Léniz-Maturana et al., 2022). Sangsawang & Sangsawang (2023) observed that the maternal efficacy of adolescent girls decreased due to social distancing, which was associated with PPD. Before the pandemic, children of adolescent mothers with lower maternal efficacy were found to have lower emotional self-regulation (Léniz-Maturana et al., 2022).
In addition to the difficulties associated with COVID-19, even under normal circumstances, adolescent mothers are more likely to have obstetric complications, and premature babies (< 37 weeks of gestation or gw) with low birth weight (< 2500g; Ganchimeg et al., 2014). In some contexts, adolescent mothers are stigmatized, especially if they do not have a partner, which reduces social support (Merriman et al., 2023; Moltrecht et al., 2022), except from their mothers, who tend to support them (Alvarez-Nieto et al., 2014). Moreover, many fail to overcome the cycle of poverty due to educational lag (UNFPA, 2020). The disadvantages of adolescent mothers contribute to depression, which can affect their parenting and increase the risk of behavioral problems in their children (Hodgkinson et al., 2014). In Mexico, between 16.05% (deCastro et al., 2011) and 33.3% (Patiño, 2016) of adolescents have been found to have PPD.
In short, previous studies focused on the challenges and emotions faced by adolescent mothers during the pandemic, tending to overlook the detection and analysis of factors associated with PPD and other mental health problems in this population. Only one gathered data on PPD before the pandemic and during the first months of lockdown (Astle et al., 2021). No studies were conducted in Mexico. The data available in this country show that, during the COVID-19 health crisis, pregnant adults suffered stress (32%) and depression (17.5%; Medina-Jimenez et al., 2022), greater stress was associated with higher levels of depression and social support was associated with less depression (Rivera-Rivera et al., 2021). Likewise, it was observed that experiencing pregnancy and postpartum during the pandemic was overwhelming due to the intense fear of contagion and the multiple demanding situations (Lara et al., 2023). Having data on the effects of the COVID-19 pandemic on the mental health and well-being of postpartum adolescent mothers will fill a gap in research, both in Mexico and in other countries, and serve as the basis for PPD prevention and management in this population in future crises.
Objectives
a) Determine the frequency of PPD (EPDS ≥ 9) in adolescent mothers before (AM-BP) and during the pandemic (AM-DP), b) Examine certain psychosocial factors (self-esteem, maternal efficacy, social support, depression and pregnancy anxiety, planned and desired pregnancy) in AM-BP and AM-DP, and c) Analyze whether belonging to the AM-DP group was a significant factor for experiencing PPD (EPDS ≥ 9) when adjusting for other sociodemographic, obstetric, and psychosocial factors.
METHOD
Design of the study/Places
A cross-sectional, comparative, correlational study was conducted with two groups of adolescent mothers. The first was surveyed from July 2019 to March 2020 at two Primary Health Care Centers (HC) in Mexico City (CDMX): adolescent mothers before the pandemic (AM-BP). Recruitment at HC was halted due to lockdown. The second group was surveyed online from March 8 to July 8, 2021: adolescent mothers during the pandemic (AM-DP).
Participants
The inclusion criteria were being a first-time mother, aged 14 to 19, with a baby aged two to nine months and living in Mexico City. In addition, AM-DPs were required to have an email address so they could access the online questionnaire. The exclusion criterion was for the mother to have reported having one of the following situations: 1) health problems during childbirth or postpartum requiring hospitalization for a week or longer or that caused pain and made it difficult for her to perform her everyday activities, 2) health problems in the past month unrelated to childbirth or postpartum causing hospitalization, 3) having a baby with health problems requiring hospitalization, or 4) having had very low birth weight (≤ 1.5 kg) or being born before 32 weeks’ gestation.
The sample of 82 teenage mothers was non-probabilistic and included 41 AM-BP and 41 AM-DP. The groups were matched by mother and baby ages to ensure representativeness of ages. They were also matched by whether the adolescents were in a relationship with the baby’s father, because the majority of the AM-BP had a relationship with the fathers of their babies (n = 31, 75.6%).
Measurements
Sociodemographic data: age of the mother (years) and baby (months), educational attainment, whether the mother attended school during pregnancy and postpartum, whether she worked postpartum, marital status, whether she had a relationship with the baby’s father postpartum. Socioeconomic status (SES) was evaluated using the Mexican Association of Market Intelligence and Opinion Agencies Index (AMAI, 2020), comprising seven levels: A/B high (≥ 205 points), C+ or upper-middle (166-204 points), C or middle (136-165 points), C- or lower-middle (112-135 points), D+ low (90-111 points), D poverty (48-89 points), and E extreme poverty (0-47 points; AMAI, 2020; López-Romo, 2020).
Obstetric data: Birthweight (in grams) and number of weeks of gestation at the time of delivery.
The Edinburgh Postnatal Depression Scale (EPDS; Cox et al., 1987) was used to identify mothers with a high probability of PPD rather than to establish a clinical diagnosis. It consists of ten statements with a Likert-type response (0 to 3), with the total score being calculated by adding the scores of each item. The higher the score, the greater the likelihood of PPD. Although research on the optimal cut-off point of the EPDS to identify adolescents with a high probability of depression during pregnancy and postpartum is incipient, it has been recommended to use the score ≥ 9 (Barassi & Grealish, 2022). In the validation of the instrument with low-income Mexican pregnant adolescents the optimal cut-off point (8/9), adequate sensitivity (70.4%), and specificity (84.9%; Alvarado-Esquivel et al., 2014) were obtained. With primiparous adolescent mothers in postpartum, the cut-off point ≥ 9 had a sensitivity and specificity of 90% (Venkatesh et al., 2014), which is why this cut-off point was used in this study.
The Postpartum Depression Predictors Inventory (PDPI-R; Beck, 2001; Records et al., 2007), was validated in Mexico (Ibarra-Yruegas et al., 2016) and administered to adolescent mothers (Lara et al., 2017; Patiño, 2016). Several features from the inventory were used to evaluate the psychosocial factors described below. Social support: This scale comprises twelve questions evaluating whether a woman has adequate support (from family, partner, and friends). Questions are answered with yes (0) or no (1). The total score is the sum of each item: the higher the score, the greater the participant’s dissatisfaction with the support she received. Reliability of the social support scale in this study was higher than α = .70 in AM-BP and AM-DP. 2) Depression and anxiety in pregnancy. One item was used to evaluate the perception of depression and another to evaluate the perception of anxiety during pregnancy, both of which are a retrospective measurement. The response options for each item are yes (1) or no (0). 3) Planned and desired pregnancy. One item was used to determine whether the pregnancy was planned and another to determine whether it was wanted. The response options for both questions are yes (0) or no (1).
Maternal self-esteem and efficacy were evaluated using the Rosenberg Self-Esteem Scale (1965) and the Parental Evaluation Scale (PES; Farkas-Klein, 2008). The Rosenberg scale comprises 10 statements with Likert-type responses (1 to 4). The total score is the sum of the items; the more the total score increases, the higher the level of self-esteem. Reliability is α = .86 (Ramos-Marcuse et al., 2009). The PES, designed to evaluate overall self-perception of maternal efficacy, has 10 statements answered from 0 to 10. As the total score increases, the perception of maternal efficacy rises. Reliability is α = .77 (Léniz-Maturana et al., 2022).
Procedure
AM-BP. Those who attended the immunization appointment with their babies at the HC were invited to answer the survey. The survey was administered if they met the selection criteria and signed the informed consent form (IC). Any doubts the participants had were clarified before they signed the IC. The author and two trained psychology interns administered the surveys.
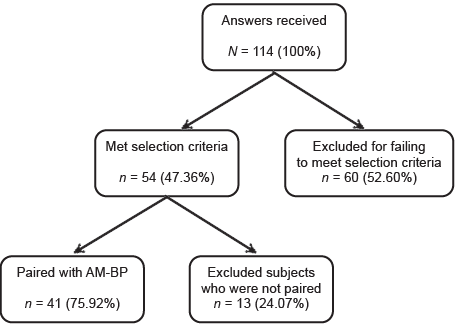
AM-DP. These adolescent mothers were recruited through an online survey developed with the Google forms tool. The survey was published on the Facebook page “Help for Depression” (Administered by a research project of the Ramón de la Fuente Muñiz National Institute of Psychiatry) [INPRFM]. Paid advertising was used to disseminate the survey on Facebook among the population of interest for the study, and the scope criteria were defined by sex, age, topics of interest, and location (women ages 14 to 19, with an interest in motherhood issues, postpartum and health and residing in Mexico City). In the first part of the survey, the justification and objectives of the study were presented. Those interested registered their email to see the IC and those who accepted the research conditions accessed the filter questions (selection criteria). One hundred and fourteen responses were received and 41 were finally included (Figure 1).
Statistical analyses
Descriptive statistics were obtained, and comparison analyses conducted of the groups (AM-BP and AM-DP) for sociodemographic, obstetric, psychosocial, and PPD variables (EPDS ≥ 9). χ2 (categorical variables), Student’s t for independent samples (quantitative variables meeting the assumptions of normality and homogeneity of variances), and Mann-Whitney U (quantitative variables that did not meet the assumption of normality) tests were performed. The assumptions of normality and homogeneity were evaluated using the Kolmogorov-Smirnov and Levene tests. Differences between the groups of paired variables were not analyzed.
The following analyses were conducted to determine whether there was a greater probability of PPD (EPDS ≥ 9) (dependent variable) among AM-DP than in AM-BP when adjusting for other sociodemographic, obstetric, and psychosocial factors (independent variables): simple logistic regression models to evaluate the association between the groups (AM-BP vs. AM-DP) and sociodemographic, obstetric and psychosocial factors (independent variables), and PPD (EPDS ≥ 9; dependent variable). A multiple logistic regression model (adjusted) was built using significant variables from previous regressions.
A significance of p < .05 was used for the difference and association tests. Analyses were performed using SPSS Version 25 (International Business Machines [IBM], 2017).
Ethical considerations
This research was approved by the INPRFM Research Ethics Committee (Initial CEI/C/096/2018. Addendum CEI/C/005/2021). All participants gave their consent prior to their inclusion in the study. In return for their participation, they were given a pamphlet on PPD and a directory of psychological, legal, and sexual health advice.
RESULTS
Sociodemographic and obstetric factors
As can be seen from Table 1, the average age of mothers was 17.7 years (SD = 1.3) and the average age of babies 4.7 months (SD = 2.2), with 45.1% having middle/lower middle SES and 50% having completed their basic education. There were no differences between groups in regard to sociodemographic or obstetric factors.
Table 1 Descriptive analyses and comparison of sociodemographic and obstetric factors
| AM-BP (n = 41) | AM-DP (n = 41) | Total (N = 82) | p | |
|---|---|---|---|---|
| Sociodemographic data | ||||
| Mother’s age (years) | 17.7 (SD = 1.3) | 17.7 (SD = 1.3) | 17.7 (SD = 1.3) | NA |
| Baby’s age (months) | 4.7 (SD = 2.2) | 4.7 (SD = 2.2) | 4.7 (SD = 2.2) | NA |
| SES | ||||
| A/B and C+ (High /upper middle) | 10 (24.4%) | 8 (19.5%) | 18 (22.0%) | |
| C and C - (Middle/lower-middle) | 21 (51.2%) | 16 (39.0%) | 37 (45.1%) | .258a |
| D+ D and E (Low level/poverty) | 10 (24.4%) | 17 (41.5%) | 27 (32.9%) | |
| Educational Attainment | ||||
| Basic | 21 (51.2%) | 20 (48.8%) | 41 (50%) | .825a |
| Middle school | 20 (48.8%) | 21 (51.2%) | 41 (50%) | |
| Attended school at the time they became pregnant | ||||
| Yes | 16 (39.0%) | 19 (46.3%) | 35 (42.7%) | .503a |
| No | 25 (61.0%) | 22 (53.7%) | 47 (57.3%) | |
| Attended school postpartum | ||||
| Yes | 9 (22.9%) | 13 (31.7%) | 22 (26.8%) | .319a |
| No | 32 (78.0%) | 28 (68.3%) | 60 (73.2%) | |
| Marital status | ||||
| Married/Living together | 28 (68.3%) | 29 (70.7%) | 57 (69.5%) | .810a |
| Single/Separated | 13 (31.7%) | 12 (29.3) | 25 (30.5%) | |
| In a relationship with the baby’s father | ||||
| Yes | 31 (75.6%) | 31 (75.6%) | 62 (75.6%) | NA |
| No | 10 (24.4%) | 10 (24.4%) | 20 (24.4%) | |
| Work (at the time of the survey) | ||||
| Yes | 6 (14.6%) | 5 (12.2%) | 11 (13.4%) | .746a |
| No | 35 (85.4%) | 36 (87.8%) | 71 (86.6%) | |
| Obstetrics | ||||
| Gestation weeks at delivery | 39.1 (SD = 1.4) | 38.6 (SD = 1.7) | 38.8 (SD = 1.6) | .343b |
| Birthweight (g) | 2984.7 (SD = 456.2) | 2961.2 (SD = 402.1) | 2972.9 (SD = 427.5) | .805c |
Notes: AM-BP = Adolescent mothers before the pandemic; AM-DP = Adolescent mothers during the pandemic; SES = Socioeconomic Status; GW = Gestation weeks at delivery. Test performed:
aX2;
bU Mann Whitney;
ct test.
PPD (EPDS ≥ 9) and psychosocial factors
As shown in Table 2, 26.8% of AM-BP reported PPD (EPDS ≥ 9) compared to 68.35% of AM-DP, in other words, PPD (EPDS ≥ 9) was 42% higher in MA-DP (p = .001). In regard to psychosocial factors, it was found that AM-DP had significantly lower scores in maternal efficacy (p = .001) and self-esteem (p = .008), as well as greater dissatisfaction with their overall social support (p = .030) and support from their families (p =.022) than AM-BP. Furthermore, AM-DPs reported feeling depressed (82.9%; p = .001) and/or anxious (70.7%; p = .014) during pregnancy more frequently than AM-BPs. No differences were found between the groups in terms of wanted and planned pregnancies.
Table 2 Descriptive analyses and group comparison: PPD (EPDS ≥ 9) and psychosocial factors
| AM-BP (n = 41) | AM-DP (n = 41) | Total (N = 82) | p | |
|---|---|---|---|---|
| PPD | ||||
| Yes (EPDS ≥ 9) | 11 (26.8%) | 28 (68.35%) | 39 (47.6%) | .001a |
| No (EPDS < 9) | 30 (73.2%) | 13 (31.7%) | 43 (52.4%) | |
| Maternal efficacy R [0-10] | 7.6 (SD 1.6) | 6.2 (SD 1.8) | 6.9 (SD 1.8) | .001c |
| Self-esteem R [10-40] | 32.0 (SD 4.8) | 28.7 (SD 6.1) | 30.4 (SD 5.7) | .008b |
| Dissatisfaction with overall social support and by type of source | ||||
| Overall or total† R [0-12] | 3.8 (SD = 2.4) | 5.1 (SD = 2.7) | 4.4 (SD = 2.6) | .030b |
| Partner R [0-4] | 1.2 (SD = 1.7) | 1.6 (SD = 1.5) | 1.4 (SD = 1.6) | .189b |
| Family R [0-4] | .34 (SD = .79) | 1.0 (SD = 1.3) | .6 (SD = 1.1) | .022b |
| Friends R [0-4] | 2.2 (SD = 1.6) | 2.5 (SD = 1.6) | 2.4 (SD = 1.6) | .321b |
| Depression during pregnancy | ||||
| Yes | 13 (31.7%) | 34 (82.9%) | 47 (57.4%) | .001a |
| No | 28 (68.3%) | 7 (17.1%) | 34 (42.7%) | |
| Anxiety during pregnancy | ||||
| Yes | 18 (43.9%) | 29 (70.7%) | 47 (53.3%) | .014a |
| No | 23 (56.1%) | 12 (29.3%) | 35 (42.7%) | |
| Planned pregnancy | ||||
| Yes | 9 (22.2%) | 14 (34.1%) | 23 (28.0%) | .219a |
| No | 32 (78.0%) | 27 (65.9%) | 59 (72.0%) | |
| Wanted pregnancy | ||||
| Yes | 28 (68.3%) | 28 (68.3%) | 56 (68.3%) | 1.00a |
| No | 13 (31.7%) | 13 (31.7%) | 26 (31.7%) | |
Notes: AM-BP = Adolescent mothers before the pandemic; AM-DP = Adolescent mothers during the pandemic; R = Response range. Test performed:
aX2;
b U Mann Whitney;
ct test.
†The higher the score, the greater the dissatisfaction with social support.
Association between groups (AM-BP vs AM-DP), sociodemographic, obstetric, and psychosocial factors and PPD (EPDS ≥ 9)
Table 3 shows the logistic regression models (simple) used to analyze the association between the groups (AM-BP vs. AM-DP) and sociodemographic, obstetric, and psychosocial factors and PPD (EPDS ≥ 9). The results show that belonging to the AM-DP group (p = .001), having lower maternal efficacy (p = .001), lower self-esteem (p = .001), and greater dissatisfaction with overall social support (p = .001) ), their partners (p = .006) and family (p = .013), and presenting with depression (p = .001) and anxiety (p = .013) during pregnancy increased the probability of PPD (EPDS ≥ 9). Table 4 shows the multiple logistic regression model, adjusted for factors such as the group to which the mother belongs (AM-BP and AM-DP), maternal efficacy, self-esteem, dissatisfaction with overall social support, depression, and anxiety during pregnancy. The results indicate that the AM-DP group was no longer significant for PPD (EPDS ≥ 9) when other factors were adjusted for. In this model, self-esteem was the only prevailing factor associated with PPD (EPDS ≥ 9; p = .017). The data fit well with the multiple logistic regression model (χ2 = 55.995; p = .001).
Table 3 Simple logistic regression model for total sample (N = 82): Association between group to which the mother belongs, sociodemographic, obstetric, and psychosocial factors and PPD (EPDS ≥ 9)
| OR | p | 95 CI | |
|---|---|---|---|
| Teenage mother group | |||
| AM-BP | Ref. | - | - |
| AM-DP | 5.874 | .001 | 2.263-15.348 |
| Sociodemographic data | |||
| Age of teenage mother | .756 | .113 | .535-1.068 |
| Socioeconomic status | |||
| A/B and C+ (High / upper-middle) | Ref. | - | - |
| C and C - (Middle/lower-middle) | 1.071 | .907 | .338-3.393 |
| D+ D and E (Low level/poverty) | 2.671 | .117 | .782-9.122 |
| Educational attainment | |||
| Basic (elementary and junior high school) | 1.635 | .270 | .683 |
| Middle school (senior high school) | Ref. | - | - |
| Attended school during pregnancy | |||
| Yes | Ref. | - | - |
| No | 1.138 | .773 | .473-2.736 |
| Attended school postpartum | |||
| Yes | Ref. | - | - |
| No | 1.444 | .466 | .537-3.884 |
| Marital status | |||
| Single/Separated | 1.629 | .313 | .632-4.201 |
| Married/Cohabiting | Ref. | - | - |
| In a relationship with the baby’s father | |||
| Yes | Ref. | - | - |
| No | 1.484 | .445 | .539-4.087 |
| Work (at the time of the survey) | |||
| Yes | Ref. | - | - |
| No | .469 | .259 | .126-1.745 |
| Obstetrics | |||
| GW at delivery | .959 | .759 | .733-1.254 |
| Birthweight (grs) | 1.00 | .937 | .999-1.001 |
| Psychosocial | |||
| Maternal efficacy | .414 | .001 | .281-.608 |
| Self-esteem | .753 | .001 | .666-.850 |
| Dissatisfaction with social support | |||
| Overall or total† | 1.483 | .001 | 1.197-1.838 |
| Partner | 1.489 | .006 | 1.119-1.981 |
| Family | 1.785 | .013 | 1.130-2.822 |
| Friends | 1.294 | .070 | .979-1.711 |
| Depression in pregnancy | |||
| Yes | 11.393 | .001 | 3.874-33.503 |
| No | Ref. | - | - |
| Anxiety during pregnancy | |||
| Yes | 3.215 | .013 | 1.280-8.078 |
| No | Ref. | - | - |
| Planned pregnancy | |||
| Yes | Ref. | - | - |
| No | 1.257 | .644 | .477-3.314 |
| Wanted pregnancy | |||
| Yes | Ref. | - | - |
| No | 1.818 | .213 | .710-4.659 |
Notes: OR = (odds ratio/odds ratio); CI = Confidence interval; AM-BP = Teenage mothers before the pandemic; AM-DP = Teenage mothers during the pandemic; GW = Gestation weeks at time of delivery.
†The higher the score, the greater the dissatisfaction with the social support received.
Table 4 Multiple logistic regression model for the total sample (N = 82): Association of group to which mother belongs and psychosocial factors with PPD (EPDS ≥ 9)
| OR-A | p | 95 CI | |
|---|---|---|---|
| Group to which the teenage mother belongs | |||
| AM-BP | Ref. | - | - |
| AM-DP | 1.474 | .613 | .328 - 6.625 |
| Psychosocial aspects | |||
| Maternal efficacy | .663 | .103 | .405 - 1.087 |
| Self-esteem | .826 | .017 | .737 - .971 |
| Dissatisfaction with social support | 1.430 | .073 | .967 - 2.13 |
| Depression in pregnancy | |||
| Yes | 4.059 | .082 | .836 - 19.713 |
| No | Ref. | - | - |
| Anxiety during pregnancy | |||
| Yes | 2.478 | .219 | .584 - 10.517 |
| No | Ref. | - | - |
Notes: OR-A = (adjusted odds ratio); CI = Confidence interval; AM-BP = Adolescent mothers before the pandemic; AM-DP = Adolescent mothers during the pandemic. Model X2 = 55.995; p = 0.001.
DISCUSSION AND CONCLUSION
The first objective of the study was to determine the frequency of PPD (EPDS ≥ 9) in AM-BP and AM-DP. The results show that PPD (EPDS ≥ 9) was 41.5% more frequent in AM-DP than in AM-BP, which was significant given that the groups had similar sociodemographic and obstetric features. This increase may reflect the stressful situations young mothers faced: fear of having loved ones with COVID-19, financial problems, and fear of interacting with other people (Astle et al., 2021; Smiley et al., 2021; Merriman et al., 2023).
A comparison of the PPD (EPDS ≥ 9) of the AM-DP (68.35%, EPDS ≥ 9) with similar research showed that it was higher than that of other adolescent mothers who also experienced their postpartum during the pandemic (36%, EPDS ≥ 13; Sangsawang & Sangsawang, 2023). These differences can be attributed to the use of different cut-off points, the fact that this study was based on an online survey, and the context and risk factors to which Mexican adolescent mothers were exposed. In regard to context, data in Sangsawang & Sangsawang (2023) were gathered during lockdown, whereas those for this article were collected between March 8 and July 8, 2021, following a spike in infections and deaths due to the pandemic in Mexico. During this period, it was confirmed that although the country had exceeded the worst-case scenario threefold, compulsory lockdown was not restored (Sánchez-Tanquer et al., 2021).
The analysis of sociodemographic, obstetric, and psychosocial factors before and during the pandemic showed differences in all psychosocial factors, with AM-DP displaying lower self-esteem, lower maternal efficacy, greater dissatisfaction with overall social and family support and a history of anxiety and depression during pregnancy. These results coincide with previous research reporting that, the greater the perception of stress due to the pandemic, the lower the parenting effectiveness-in adults (Xue et al., 2021; Gniewosz, 2022) and the lower the self-esteem of adolescents (Goto et al., 2022). They are also consistent with research showing a lack of support from the partners and families of adolescents during the pandemic (Moltrecht et al., 2022; Merriman et al., 2023), which impacted their perception of maternal efficacy due to their feeling that they lacked sufficient practical support and information to promote their babies’ development (Moltrecht et al., 2022).
Evidence was found of higher percentages of perceived depression (82.9%) and anxiety (70%) during pregnancy among AM-DP than AM-BP. Among the former, percentages were also higher than among other groups of pregnant adolescents who experienced the pandemic: depression = 43% (Tele et al., 2022) and anxiety = 45.5% (Chamdimba et al., 2022). The perception of depression and anxiety in pregnancy of AM-DP may be overestimated since they were retrospectively evaluated with single items rather than with conventional scales as in the comparison studies (Tele et al., 2022; Chamdimba et al., 2022). It should be noted, however, that these measurements have proved effective in identifying depression and anxiety symptoms in pregnancy and postpartum (Lara et al., 2017; Patiño, 2016; Marcos-Nájera et al., 2021).
In regard to the third objective, determining whether belonging to the AM-DP group was a significant factor in experiencing PPD (EPDS ≥ 9), simple association analyses showed that being an AM-DP, presenting with lower levels of self-esteem, greater dissatisfaction with overall social support, from their partners and families, as well as experiencing depression and anxiety during pregnancy were associated with PPD (EPDS ≥ 9). As in previous studies, these data confirm the association between low maternal efficacy (Lara et al., 2017; Léniz-Maturana et al., 2022), low self-esteem (Birkeland et al., 2005; Ramos-Marcuse et al., 2009), dissatisfaction with social support (deCastro et al., 2011; Kim et al., 2014), having depression or anxiety during pregnancy (Patiño, 2016), and becoming a mother during the pandemic (Bower et al., 2023) and PPD (EPDS ≥ 9).
A key finding was that, when controlling for the previous factors in a multiple analysis, the only significant factor for presenting with PPD (EPDS ≥ 9) was having lower self-esteem. These data place self-esteem at the center of the relationship between psychosocial factors and PPD. There are two possible explanations for this result. First, adolescence sees a decline in self-esteem—particularly in girls—attributable to changes in body image, the emerging ability to think abstractly about oneself and the future, and to experiencing more challenging situations than in childhood (Robins & Trzesniewski, 2005). Second, being a mother can influence how adolescents perceive themselves (Mora-Guerrero et al., 2021). It can contribute to their self-esteem and identity if they regard it as an opportunity to mature and give meaning to their life, but if they regard it more as an event entailing unwanted responsibilities, it can have negative effects on their self-esteem and identity (Melgar, 2015; Patiño, 2016; Mora-Guerrero et al., 2021). The continuous discrepancy between the ideal and the real self leads to negative thoughts and feelings (Escalante, 2004), a central factor in depression (Abdel-Khalek, 2016).
This suggests that, under normal circumstances and particularly in emergencies, self-esteem should be regarded as a key element in programs to prevent PPD that can begin during pregnancy and continue in the first year postpartum. Likewise, self-esteem should be considered in interventions to treat those who have already been identified with depression in their pregnancy and postpartum. It has already been noted that social support has positive effects on the self-esteem of adolescents and their motherhood: respectful support makes it easier for them to acquire confidence in their abilities and make more appropriate decisions about their life and parenting (Mora-Guerrero et al., 2021).
Strengths: To the best of our knowledge, this is the first study in Mexico to provide information on the psychosocial and mental health factors of adolescent mothers during the pandemic and include a comparison group prior to the health crisis. In general, there is a dearth of research exploring the mental health of adolescents during pregnancy and the postpartum period compared to those of adult mothers. In this respect, this study contributes to lending visibility to the problem. On the other hand, it is relevant that the most widely recognized self-report scale (EPDS) was used to identify those with a high probability of presenting PPD. In addition, a cut-off point was selected that has shown adequate sensitivity and specificity in primiparous and postpartum adolescent mothers (Venkatesh et al., 2014). It should be noted, however, that the EPDS is not a clinical diagnosis.
Limitations: The study is cross-sectional, which only enables levels of association to be established between variables. At the same time, the data correspond to adolescent mothers living in Mexico City, who use primary care health centers (AM-BP) and Facebook (AM-DP). These circumstances limit their generalization to other groups of adolescent mothers who do not share these characteristics. The level of commitment of participants and the social desirability bias (Singh & Sagar, 2021) may differ due to the two methods of administering the survey, although it is not known how this may be reflected. Moreover, both groups primarily comprise people interested in obtaining mental health information and support for themselves, which could be particularly true of AM-DP who answered the online survey a year after the start of the health crisis. Another limitation was that since adolescent mothers were not asked about adverse events they had experienced during the pandemic, we do not know how they may have influenced PPD (EPDS ≥ 9).
In conclusion, AM-DP experienced more PPD (EPDS ≥ 9) than AM-BP. The crisis impacted various psychosocial factors associated with PPD (EPDS ≥ 9). The role of self-esteem in PPD (EPDS ≥ 9) prevails over other factors. These data show how major crises can affect this already vulnerable population and suggests elements to be considered when implementing mental health prevention and treatment measures in this population, such as boosting self-esteem.











 nueva página del texto (beta)
nueva página del texto (beta)