INTRODUCTION
Patient-physician relationships have been widely studied in the context of chronic health problems. For people living with HIV (PLWH), being seen by different doctors each time or exposure to negative attitudes, like stigma, discrimination or prejudices, shown by medical staff can lead to poor outcomes such as inadequate adherence to antiretroviral treatment (ART) or loss of follow-up (Kuznetsova et al., 2016; Westergaard, Hess, Astemborski, Mehta, & Kirk, 2013). On the other hand, positive experiences with health professionals, health professionals who respond to the emotional needs of patients, satisfaction with one’s doctor and belief in the physician’s competence, have been reported as facilitators for an adequate medical follow-up (Brincks, Feaster, Burns, & Mitrani, 2010; Hurley et al., 2018; Kuznetsova et al., 2016; Yehia et al., 2015).
As a general construct, patient-physician relationships can include different components, such as patient’s satisfaction with care, physician’s communication style or agreement between the patient and physician (Brincks et al., 2010; Honavar, 2018). A determining factor in the patient-physician relationship is patients’ trust in their doctors (Hall, Dugan, Zheng, & Mishra, 2001; Hall et al., 2002). In this sense, in individuals with chronic illness, trust in their doctors has been associated with positive health outcomes, treatment compliance and adherence to doctors’ recommendations (Kerse et al., 2004; Piette, Heisler, Krein, & Kerr, 2005). Similar associations between trust in physicians and adherence to medications and treatment have been found in people living with HIV (Graham, Shahani, Grimes, Hartman, & Giordano, 2015; Roberts, 2002; Schneider, Kaplan, Greenfield, Li, & Wilson, 2004; Whetten et al., 2006), in which adherence to treatment have an impact not only on individual health (Gebrezgabher et al., 2017) but also on public health, preventing transmission of the virus (Skarbinski et al., 2015) or development of drug resistance (Almeida et al., 2014).
The Trust in Physician Scale (TPS; Anderson & Dedrick, 1990) is a psychometric test that measures the patient’s trust in their doctor and consists of 11 items measured in a five-point Likert format with response options ranging from “strongly agree” to “strongly disagree.” The instrument has shown adequate internal consistency (Cronbach’s alphas between .85 - .90) and construct and predictive validity (Thom, Ribisl, Stewart, & Luke, 1999). When used in PLWH, it has shown adequate psychometric characteristics (Piette et al., 2005). Trust in doctor measured with this instrument was significantly related to patients’ desires for control in their patient-physician interactions and to subsequent satisfaction with care (Anderson & Dedrick, 1990).
The instrument has been used in different studies (Aloba, Mapayi, Akinsulore, Ukpong, & Fatoye, 2014; Freburger, Callahan, Currey, & Anderson, 2003; Kalsingh, Veliah, & Gopichandran, 2017) but to date, it has not been validated in Spanish for use in a Mexican population. Considering the important relationship between this construct, adherence to ART and quality of life in PLWH, and the fact that in Mexico, inadequate adherence rates between 40% and 50% have been reported (Peñarrieta et al., 2009; Plascencia de la Torre et al., 2019), it is considered relevant to improve knowledge about trust in physician for which it is essential to have adequate and reliable instruments to evaluate it. We thus adapted and validated the TPS to Spanish and evaluated its psychometric properties in a sample of people living with HIV in Mexico.
METHOD
Design of study
Cross-sectional study, data of this study was part of a larger study aimed to assess which sociodemographic, clinical, contextual, behavioral, psychological, and care-related variables were associated to loss to follow-up in people living with HIV.
Participants and place
Participants of the study were people living with HIV, over 18 years of age, receiving care at an HIV healthcare clinic inside a third-level hospital in Mexico City and who agreed to participate in the study. Due to COVID-19 related restrictions, the test was applied online. Invitations to participate in the study were sent by email to patients receiving care in the HIV clinic. E-mails were in database of the HIV clinic and were used as a routine form of contact with patients. They had previously authorized the use of their e-mail addresses to send them information, including invitations to research protocols. Invitations were also posted on the clinic’s social networks (Facebook and Twitter). A sample size of at least 10 participants by item was established to perform the exploratory factor analysis (EFA) and 20 participants by item to perform the confirmatory factor analysis (CFA; Boateng, Neilands, Frongillo, Melgar-Quiñonez, & Young, 2018; Nunnally, 1978).
Measurements
The sociodemographic variables age, gender, marital status, and educational level were collected. Participants were also asked if they were taking antiretroviral therapy (ART) and how many months had passed since their diagnosis.
To measure trust in physician, the adapted TPS (Anderson & Dedrick, 1990) was used. The original scale is composed of 11 items (seven written in direct form and four in inverse form). Each item contains five response options ranging from strongly disagree (“1”) to strongly agree (“5”). Scores range from 11 to 55, with higher scores indicating greater trust in the physician.
Procedure
Three HIV-specialized psychologists independently translated the TPS from English to Spanish for Mexico and made the cultural adaptation to the clinic’s HIV patients. Translations were compared, reaching agreements on the discrepancies. This version was back-translated into English by a bilingual health professional outside of the study team to ensure the meaning of the items was maintained in the Spanish translation. Following the suggested procedure (Reyes Lagunes & García y Barragán, 2008), a pilot study was conducted with 10 participants to ensure understanding of the items and instructions, only one person had doubts in two of the items. They were carefully reviewed by three expert psychologists, and since no difficulties were found in those items, and the rest of the participants in the pilot test did not report any difficulties, it was concluded that the lack of understanding could be due to the person and not to the items.
Data from first sample to carried out the EFA was collected online between April and May 2020; and data from second sample to carried out the CFA was collected between November 2020 and May 2021. As participation was anonymous, to ensure that the respondents were the target population, they were asked if they were living with HIV, in case they did not self-report HIV, the responses of these participants were eliminated. Respondents were then directed to fill a sociodemographic questionnaire and to fill out the translated and adapted version of TPS. This version was also composed of 11 items (direct and inverse) containing five response options ranging from strongly disagree (“1”) to strongly agree (“5”).
Statistical analysis
Items that were written inversely to measure confidence (1, 5, 7 and 11) were recoded. Frequencies, percentages, means, standard deviation (SD), medians and inter-quartile ranges (IQR) were used to describe sociodemographic variables. Intra-variability for each participant was calculated to eliminate those who had responded exactly the same to each item or who had a response pattern. Outliers were explored through box and whisker plots; skewness values were expected to be less than |1| and kurtosis values less than |2|. The frequency of the response options in each item was examined, paying attention to those with more than 50% or more than 30% in the extreme answer options. To confirm the adequacy and variability of the sample, the Kaiser‐Meyer‐Olkin (KMO) value (expecting it to be > .70) and the Bartlett test of sphericity (expecting it to be significant, p > .001) were calculated before carrying out the exploratory factorial analysis (Thompson, 2008).
For psychometric properties, in the first sample reliability was evaluated with Cronbach’s alpha internal consistency index (expecting it to be greater than .80). We expected the item-scale correlation to be greater than .35 in all items and that Cronbach’s alpha did not increase when eliminating any of them (DeVellis, 2017). Construct validity was evaluated with EFA, using the principal axis factoring, expecting factor loadings > .40 and an explained variance > 45% (Osborne, 2014). These analyses were performed using IBM® SPSS® Statistics Version 26. CFA was performed in the second sample using AMOS® Version 24. A single-factor model was tested with the solution provided by the EFA. Several fit indices were calculated: the model χ2 and its p value, expecting it to be non-significant (> .05); the root mean square error of approximation (RMSEA), where values < .05 represent an excellent fit, and values < .08 represent an adequate fit; the standardized root mean square residual (SRMR), in which values less than or equal to .08 indicate good fit; and the Comparative Fit Index (CFI); where values greater than or equal to .95 indicate a good fit (Bentler, 1990; Browne & Cudeck, 1992).
Ethical considerations
This study was performed in line with the principles of the Declaration of Helsinki. Research Board of the Instituto Nacional de Enfermedades Respiratorias (INER) review the study and approved online informed consent (approval number C02-20). The answers of participants were anonymous; therefore, their confidentiality was assured. Informed consent was obtained after explaining in writing the purpose of the study and having them answer the question: Do you agree to participate in the study? If they answered no, the questionnaire did not continue.
RESULTS
In the sample used to conduct EFA, responses were received from 251 participants who answered the TPS. A total of 36 questionnaires were eliminated: 26 due to lack of variability in the answers, six because they had a response pattern, and four because they belonged to participants who were not living with HIV. Final analyses were carried out with responses from 215 participants. The vast majority (n = 207, 96.3%) were male participants, in line with the sex distribution of PLWH receiving care at the clinic where the study was carried out. Mean age was 32.45 years (SD = 7.73). More than half were single (n = 156, 72.6%) and had higher education (n = 129, 60.1%). The majority was taking ART (n = 210, 97.7%) and the median of months after diagnosis was 41 (IQR = 20-89). Table 1 describes the sociodemographic variables of the participants.
Table 1 Sociodemographic characteristics of study participants (n = 215)
| Age | |
| Mean | 32.45 |
| SD | 7.731 |
| Range | 18-50 |
| Gender % (n) | |
| Male | 96.3 (207) |
| Female | 3.7 (8) |
| Marital status % (n) | |
| Single | 72.6 (156) |
| Married | 5.1 (11) |
| Separated/Divorced | 20.0 (43) |
| Cohabitation/Civil union | 1.4 (3) |
| Widowed | .9 (2) |
| Educational level % (n) | |
| Basic education | 4.6 (10) |
| High school education | 35.3 (76) |
| Higher education | 60.1 (129) |
| Taking ART % (n) | |
| No | 2.3 (5) |
| Yes | 97.7 (210) |
| Months since diagnosis | |
| Median | 41 |
| IQR | 20-89 |
Notes: SD: Standard deviation; IQR: Interquartile range.
Data scanning: items analysis
In the sample used to conduct EFA no outliers were found. Skewness values were less than |1| in every item, and kurtosis values were less than |2|, thus items were distributed normally. No response option had a frequency higher than 50%. However, in four questions (3, 6, 9 and 11) the extreme option “totally agree” had more than 30% of the answers, so these items could benefit from more answer options. Finally, it was found that all items were able to discriminate between extreme groups (quartile 1 and 3, p < .001), so none had to be eliminated.
Reliability
In this first sample (n = 215) correlational analysis were performed, the items 11, 1, 7 and 5 had a low correlation with the total scale (.225, .250, .357, .305 respectively) and were eliminated. When item 8 was eliminated, Cronbach’s alpha increased, so it was also removed from the test. Items were removed one by one until all items had a correlation with the scale of at least .35 and Cronbach’s alpha did not increase when they were removed. Table 2 shows the final item-scale correlation values of the items that were maintained, these range from .728 to .852. The Cronbach’s alpha coefficient for the six remaining items of the TPS scale was .93 for the overall scale, showing good internal consistency.
Construct validity
Adequacy of the first sample (n = 215) was tested using EFA trough the KMO value of .902, and Bartlett’s test of sphericity of χ2(15) = 989.47, p < .001, thus confirming adequacy and variability of the sampling. EFA results showed one factor with eigenvalue > 1, suggesting a unidimensional structure. Factor loading of all six items was over .40, so no more items were excluded. A one-factor solution explained 68.9% of the total variance, which is considered very acceptable. In Table 3, factor loading scores are shown, all of them ranging from .756 to .894.
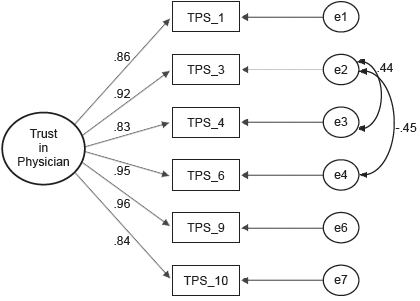
In order to confirm the factor structure of TPS, a model with six items and a single factor was tested by CFA in a second sample of 140 participants. An χ2(7) = 10.19 p = .178 was obtained, indicating good fit. The rest of the indices were then calculated to check the model fit; the RMSEA value was .057 p = .376, the SRMR was .0015 and the CFI was .997, all of them showed an adequate model fit. All factorial weights were high, ranging from .84 to .96. In figure 1 the model obtained with CFA is showed.
Sample scores
The Spanish version adapted for Mexico of TPS instrument consisted of six items, instead of 11, with a score ranging from 6 to 30. When comparing in the first sample (n = 215) the score obtained with the adapted version and the score obtained with the original version, a very high correlation is obtained (r = .990, p < .001), which indicates that even if some items are eliminated, the construct being measured does not change. With this adapted TPS version, the mean score obtained by all participants (joining both samples, n = 355) were 22.95 (SD = 6.80). Fourteen people obtained the lowest score in trust in his physician (3.9%) and 63 people obtained the highest score (17.7%). No significant differences were found between men and women regarding their score (t[353] = 1.14, p = .255), nor between the different age groups (F[2,352] = 2.29, p = .102). Table 4 shows means and standard deviation of the scores by sex and age group.
DISCUSSION AND CONCLUSION
The TPS translated and adapted in a sample of people living with HIV from Mexico was shown to be a valid and reliable instrument, consistent with the original scale (Anderson & Dedrick, 1990). The translated and adapted version was still an unifactorial scale, although it was composed by six of the 11 items of the original scale. The score that can be obtained with this adaptation ranges from 6 to 30, with higher scores indicating greater confidence in the doctor. Scores of adapted version correlated with the ones obtained with the original instrument, suggesting that they measure the same psychological construct. The final internal consistency index was also adequate (Cronbach’s alpha = .93), even higher than those found in other studies (Aloba et al., 2014; Freburger et al., 2003; Kalsingh et al., 2017) and similar to that of the original instrument (Anderson & Dedrick, 1990). The adapted version of TPS remained unifactorial, like the original instrument (Anderson & Dedrick, 1990), and explained a very high percentage of variance (almost 70%). All items were correlated with each other and had high factorial loads. These results were confirmed in a second sample by confirmatory factor analysis, which obtained adequate fit indices, showing the adapted TPS to be a reliable and valid instrument to measure patients’ trust in their doctors. This may be because the population of this study is similar to the population in which the original instrument was developed, which were adults with diabetes, another chronic disease that involves regular treatment and in which the relationship with the physician is key.
In our adapted scale, items that had a very low correlation with the total scale, which curiously coincided with the inverse items of the original scale, were removed. Inverse items (which contain negative statements, or they measure the construct in the opposite direction to the rest of the instrument) may create confusion in certain populations, especially those with low levels of education or scarce resources, leading to inconsistencies with the rest of the scale, and this may have happened for our study population. Although these items do not show lower correlation with the total test in the original instrument, other authors have also had issues with these items, Aloba and collaborates concluded they may belong to a different factor than the rest of the items (Aloba et al., 2014). To tease out these hypotheses, the translated scale could be tested with the inverted items in the same direction as the rest. Despite the elimination of these five items, the correlation between the two versions (adapted and original) is very high, suggesting that they still measure the same construct, and thus making the adapted TPS version an even simpler and shorter instrument, which can be especially useful for use in resource-poor settings, as is the situation in most of Mexico.
The instrument showed a variable spread of answers across the trust spectrum. No differences were found in the level of trust in physician between men and women, although participants were mostly male and the study did not have the power to detect differences between genders. Likewise, no differences were found in the trust score by age group, similar with what was found in other studies (Kayaniyil et al., 2009; Muir et al., 2009), probably because age does not affect the level of trust in the physician, and it is probably other variables included in the doctor-patient relationship that have a greater effect on this construct. The study did not capture data on the patients’ main physician or other potential key variables that could be associated with the observed variability, and it would be important for future studies to address them.
The level of trust in the physician found in this study is considered generally adequate, although at the moment there are no cut-off points for this construct. There are more patients who fully trust their doctors than those who scored the lowest. This would contribute to explain the very good rates of adherence to ART in this population, where the vast majority showed ART adherence of more than 95%. “Trust in the doctor” and “patient-physician relationship” in people living with HIV are very relevant elements because they are related to better commitment to care (Freburger et al., 2003), better health outcomes, better adherence to treatment and better clinical follow-up (Hall et al., 2002; Hurley et al., 2018; Mechanic & Meyer, 2000; Safran et al., 1998), which implies important benefits for individual and public health.
Limitations of the study include that it had to be carried out online due to the COVID-19 pandemic. This can bias the study by excluding people with no Internet access, who don’t follow the clinic’s social networks, or had not provided their email. Also, in online surveys it cannot be controlled who answers the questionnaire, because of that, and to minimize the risk of responses were not from the target population, an HIV self-reporting question was included. Another limitation could be the relatively small sample size, it could be important to test the translated and adapted version of TPS in other Spanish-speaking populations of people living with HIV in Mexico.
The Spanish for Mexican translated and adapted version of the TPS has proven to be a reliable and valid instrument, with adequate psychometric properties and good model fit indices in people living with HIV. A reliable instrument to measure this variable can be key to detect and resolve trust issues in patient-physician relationships in a timely manner. When trust issues will be detected, they may benefit from interventions by mental health professionals, trainings, and workshops to improve patient-physician relationship and confidence in doctors and health system. While more studies are necessary to verify the construct and convergent validity of this instrument, results suggest that the adapted and translated TPS can be a useful, brief and easy-to-use tool to assess trust in doctors among Mexican people living with HIV.











 nueva página del texto (beta)
nueva página del texto (beta)