Background
The current taxonomic framework for psychiatric disorders presents both posttraumatic stress disorder and obsessive-compulsive disorder as categories characterized by specific criteria. Nonetheless, there is a noticeable overlap in the symptomatology of these disorders, which our current diagnostic model frequently fails to recognize. Ultimately, this ends up being one of the main drawbacks associated with a categorical approach in psychiatric practice. (Kendall, Brady, & Verduin, 2001). Taking this into account, the broad spectrum of anxiety disorders is no exception to this issue. Several symptomatic domains characterized by intrusive, repetitive, and multimodal cognitions that cause distress outline this heterogenous group of constructs. These could be further formulated into five symptomatic domains: fear, recurrent thoughts, intrusive images, physical symptoms, and avoidance (Cohen, Mychailyszyn, Settipani, Crawley, & Kendall, 2011). The obsessive-compulsive disorder (OCD) is an entity defined by the presence of obsessions and/or compulsions. Obsessions represent recurrent and persistent thoughts, impulses, or images that are intrusive, inappropriate, and experienced as distressing, while compulsions indicate repetitive, intentional behaviors carried out according to inflexible rules to reduce such distress. Similarly, the posttraumatic stress disorder (PTSD) is characterized by a cluster of symptoms that develop in response to trauma, an experience in which an individual lives or witnesses an event involving actual or threatened death, serious injury or peril to the integrity of itself or others (American Psychiatric Association, 2013). Coincidentally, OCD and PTSD share some clinical domains, with the occurrence of intrusive symptoms being common in both conditions. Whereas OCD patients tend to experience intrusive phenomena of distressing events, PTSD patients usually experience them as recurrent memories of their traumatic experience (Morina et al., 2016).
This theoretical, clinical, and empirical overlapping of functional connections between OCD and PTSD has been discussed previously (Gershuny, Baer, Radomsky, Wilson, & Jenike, 2003). However, the frequency of this phenomenon remains relatively understudied (Huppert et al., 2005; Nacasch, Fostick, & Zohar, 2011). Furthermore, similarities between recurrent, intrusive thoughts between both entities continue to be among the most challenging aspects of the clinical differential diagnosis process in current psychiatric practice (Cohen et al., 2011). Previous efforts that sought to explain these phenomena pondered a biological and environmental role following an exposure to traumatic events and OCD (Fostick, Nacasch, & Zohar, 2012).
According to this, some researchers believe that trauma in adults could be an arbiter for gene-environment transactions that lead to a late phenotypic expression of OCD (Lafleur et al., 2011; Sasson et al., 2005). Other authors suggest that there may be a temporal connection between specific types of trauma and the development of OCD symptoms (Fontenelle et al., 2012). Likewise, interpersonal traumas and certain personality traits also may play a predictive role in PTSD diagnosis or severity in OCD patients (Gershuny et al., 2008). Interestingly, traumatic experiences may be highly prevalent in children with OCD (Lafleur et al., 2011), and child abuse may be a relevant factor in regards to clinical, functional, and trauma-related differences between pretraumatic and posttraumatic OCD diagnosis in PTSD patients (Araújo et al., 2018). In addition, mental imagery, another main feature of many anxiety disorders, has been functionally linked to earlier adverse events (Speckens, Hackmann, Ehlers, & Cuthbert, 2007). This shouldn’t be surprising, given that both disorders interact with elements of threat conditioning and fear extinction, features which play a role in the development of both disorders (McGuire et al., 2016). Also, it has been shown that individuals with comorbid OCD and PTSD have a higher prevalence of severe OCD symptoms in a lifespan course than those without lifetime PTSD (Ojserkis et al., 2017). Given these points, it is worth noting that current medical literature available in regards to the relationship between PTSD and OCD is limited, which makes understanding their comorbidity and impact on their treatment outcomes a challenging undertaking (Van Kirk, Fletcher, Wanner, Hundt, & Teng, 2018). Hence, as a main objective, this research aims to provide a comprehensive overview of empirical and observational studies involving the symptomatic overlap between OCD and PTSD.
Method
Data source, search strategy, and research questions
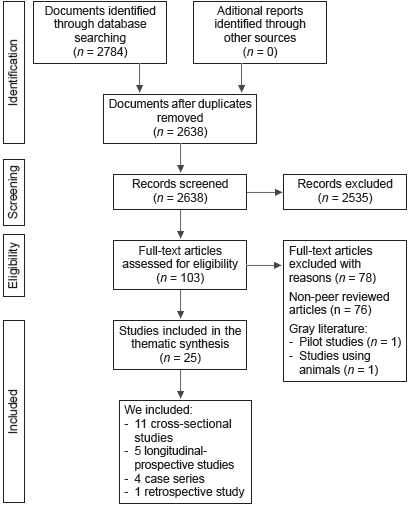
No previous systematic review that focused on this phenomenon of interest was found after a comprehensive search in the PROSPERO database. Thus, this review was not registered in the International Prospective Register of Systematic Reviews, since according to the National Institute of Health Research, scoping reviews are ineligible for registration into PROSPERO. A review of literature was undertaken to identify all relevant publications concerning the overlap of OCD and PTSD symptomatology. We followed the PRISMA-ScR Statement (Moher et al., 2009), and the following research questions were formulated: 1. Does a functional connection exist between OCD and PTSD symptoms? 2. Which variables (e.g., risk factors, clinical similarities, treatment implications, etc.) influence the treatment outcomes of patients with mutual OCD and PTSD symptom clusters? Consequently, two independent authors searched PubMed, PsycINFO, and Web of Science databases between April 01 and July 26, 2020. The search was made from inception through July 26, 2020 using the following terms: (overlap of) AND (symptoms OR symptomatology); (OCD) OR (obsessive OR compulsive) AND (PTSD) OR (posttraumatic OR trauma); (“humans”[Mesh]AND “comorbidity”[Mesh]); (“Obsessive-Compulsive Disorder / diagnosis”[Mesh]) AND “Obsessive-Compulsive Disorder / epidemiology”[Mesh] AND “Obsessive-Compulsive Disorder / psychology” [Mesh]); (“Stress Disorders, Post-Traumatic / diagnosis”[Mesh]) AND (“Stress Disorders, Post-Traumatic / epidemiology”[Mesh] AND “Stress Disorders, Post-Traumatic / psychology” [Mesh]).
Eligibility criteria
Initially, we restricted our literature search to include articles that met the following criteria according to the key words mentioned above: studies published in English in peer reviewed journals that contributed quantitative or qualitative data and that specifically addressed the relationship between OCD and PTSD symptoms as the main aim or outcome of the study. Secondly, non-peer-reviewed articles, studies that did not address this phenomenon of interest and gray literature documents were excluded. Thirdly, we eliminated all duplicate findings from these searches following a title and abstract review. Lastly, the reference lists of all articles that were relevant, as well as any recent review papers that examined this phenomenon, were surveyed in full detail to determine if they met our inclusion criteria. No other conditions than those previously described were applied to our study selection. Most initial search results (2,784) were excluded because of unrelatedness in the title or abstract regarding our subject matter (e.g., “traumatic brain injury,” “surgical trauma,” “compulsive exercise” etc.), and thus, the search resulted in 103 articles for further review. After additional inquiry, we narrowed these articles down to 25 relevant to the present study. Data and biases from these studies were scrutinized using critical appraisal tools, such as the Newcastle-Ottawa Scale for cross sectional, retrospective and cohort studies, and the Joanna Briggs Institute’s Critical Appraisal Tools for case series and case reports (Jordan, Lockwood, Munn, & Aromataris, 2019; Stang, 2010). Pertaining to their methodological approach, we included 11 cross-sectional studies, five longitudinal-prospective studies, four case series, four case studies and one retrospective study. Ultimately, all included studies were read, and key pieces of information were extracted, considering their sample size, recruitment process, design, outcomes, measures, psychometric tools used, main results, and consequences for future research.
Analysis
We did not conduct any statistical test or meta-analysis because of methodological disparities between the included studies. Likewise, weighting the studies was not possible or done because articles with distinct methodological approaches and properties were utilized. Taking this into account, both authors chose to examine the extent, range, and characteristics of the found evidence of this phenomenon of interest. This effort meant to summarize findings from this body of knowledge that is heterogeneous in its methods and facilitated the identification of gaps in the literature to aid the planning and commissioning of future research. Thus, a thematic synthesis was done employing the data extracted, since scoping reviews is a type of knowledge synthesis that follows a systematic approach to further map evidence on a topic, helping to identify main concepts, theories, and knowledge gaps that may inspire further innovative research (Figure 1).
Results
Twenty-five studies met the inclusion criteria for this review (Table 1). To our knowledge, this is the first review article addressing the putative relationship and overlap between OCD and PTSD symptom clusters utilizing studies of varied methodologies (e.g., case series, cross-sectional studies, retrospective, and prospective studies, etc.). Four types of research were identified through the thematic analysis of the included studies: clinical domains; risk factors and other correlates; prognostic factors; and treatment approaches. Thus, our results section describes each of these categories. To establish confidence in the evidence reviewed we utilized the ConQual approach, a practical tool developed by the Joanna Briggs Institute, to grade the included articles according to the type of study, dependability, and credibility. The proposed system would then give an overall score of High, Moderate, Low, or Very Low. This ranking can be considered a rating of confidence in the synthesized findings. Afterwards, a summary of findings table was developed to convey the key findings of the review in a tabular format with the aim of improving the accessibility and usefulness of the systematic scoping review (Table 2; Jordan et al., 2019; Stang, 2010).
Table 1 Characteristics of the 25 included studies for the present review
|
Study authors,
and year |
Country | Design | Diagnosis population | Age | Gender |
No. of
patients |
Outcome |
|---|---|---|---|---|---|---|---|
| Pitman, 1993 | United States | Case study | Military personnel | 46 years old | Male | 1 | Concurrent OCD and PTSD. |
|
Langlois et al.,
2000 |
Canada | Cross-sectional study |
Students | 22.5 years old (mean age) |
Male and female |
254 | Disfunction caused by worry is more severe than disfunc- tion caused by obsessions. |
|
de Silva & Marks,
2001 |
United States | Case series | Treatment resistant OCD pa tientsa |
16-76 years old | Male and female |
104 | 82% reported a history of at least one trauma, 49.4% met criteria for PTSD (criteria non-disclosed). |
|
Gershuny et al.,
2002 |
United States | Cross-sectional study |
OCD patients (DSM-IVb) with previous failed trials of behavior therapy and/or medication |
19-66 years old | Male and female |
15 | Patients with comorbid PTSD had worse outcomes in be havior therapy. |
|
Gershuny et al.,
2003 |
United States | Case series | Patients who met criteria for OCD (YBOCSc) and PTSD based on interview and self-report |
Not reported | Male and female |
4 | An inverse relationship between PTSD symptoms versus OCD symptoms that may hamper therapy effectiveness. |
|
Huppert et al.,
2005 |
United States | Cross-sectional study |
128 OCD patients (OCI-Rd), 109 PTSD patients (PDSe), 63 pa- tients with other anxiety disor- ders and 40 college students |
21.7-44.5 years old (mean age) |
Male and female |
340 | Overlap of OCD and PTSD symptoms using continuous rating scales. |
|
Sasson et al.,
2005 |
Israel | Case series | Military personnel | Not reported | Male | 13 | 4 Case reports had evidence of previous trauma regard- ing OCD symptom onset. |
|
Cromer et al.,
2007 |
United States | Cross-sectional | OCD patients (YBOCSc) | 41 years old (mean age) |
Male and female |
265 | Traumatic life events are associated with higher OCD se- verity in Y-BOCSc severity ratings. |
|
Grabe et al.,
2007 |
Germany | Cross-sectional study |
OCD patients (DSM-IVb) | 37.4 years old (mean age) |
Male and female |
210 | No apparent relationship between trauma, PTSD and OCD. |
|
Speckens et al.,
2007 |
United Kingdom | Prospective study | OCD patients (DSM-IVb) | 35.7 years old (mean age) |
Male and female |
37 | Patients with traumatic mental images had more OCD symptoms. |
|
de Moraes et
al., 2008 |
Brazil | Case study | PTSD patients (criteria non-dis- closed) |
35 years old | Male | 1 | Scored 30 on the initial Y-BOCSc symptom severity post-trauma and non-responsive to pharmacotherapy. |
|
Ehring et al.,
2008 |
United Kingdom | Prospective study | Motor Vehicle Accident Survivors | 35.17 years old (mean age) |
Male and female |
147 | 22.4 % participants met criteria for PTSD (DSM-IVb) and alongside with checking behaviors. |
|
Gershuny et al.,
2008 |
United States | Cross-sectional study |
OCD patients (DSM-IV-TRf) | 32 years old (mean age) |
Male and female |
104 | 82% reported at least one trauma, 39.4% met criteria for PTSD. |
|
Shavitt et al.,
2010 |
Brazil | Prospective study | OCD patients (DSM-IVb) | 36.3 years old (mean age) |
Male and female |
219 | Patients with OCD and PTSD presented a greater re sponse in symptom dimensions through therapy versus patients without PTSD. |
|
Nacasch et al.,
2011 |
Israel | Cross-sectional study |
PTSD patients (MINIg) | 44.29 years old (mean age) |
Male and female |
44 | 41% of PTSD patients had comorbid OCD (MINIg). |
| Badour et al., | United States | Cross-sectional study |
Women with diagnosis of prev- ious sexual trauma or physical assault (DSM-IV-TRf) |
28.37 years old (mean age) |
Female | 49 | Peritraumatic self-focused disgust was significantly relat ed to contamination-based OCD symptoms (OCI-Rd). |
|
Fontenelle et al.,
2012 |
Brazil | Retrospective study | OCD patients (DSM-IVb) | 37.3 years old (mean age) |
Male and female |
1001 | OCD occurring after or near the onset of PTSD is associ- ated with distinct clinical features specially when patients did not had history of pre-traumatic OCD. |
|
Fostick et al.,
2012 |
Israel | Case series | Military personnel | 21 years old | Male | 5 | The onset of PTSD and OCD was simultaneous and oc- curred after combat trauma. |
|
Semiz et al.,
2014 |
Turkey | Cross-sectional study |
OCD patients (DSM-IVb) | 35.80 years old (mean age) |
Female | 120 | Dissociation (according to DESh) scores may be a predic- tor of poor treatment outcome. |
|
Morina et al.,
2016 |
Switzerland | Cross-sectional study |
Civilian survivors of Kosovo War. | 43.0 years old (mean age) |
Male | 51 | Participants with high levels of PTSD symptoms (PDSe) were significantly more likely to have OCD symptoms (OCI-Rd). |
|
Ojserkis et al.,
2017 |
United States | Prospective study | OCD patients (DSM-IVb) | 39.16 years old mean age) |
Male and female |
266 | PTSD patients with comorbid OCD reported significantly more OCD symptoms (Y-BOCSc). |
|
Araújo et al.,
2018 |
Brazil | Prospective study | Patients with comorbid PTSD and OCD (DSM-IVb) |
40.1 years old (mean age) |
Male and female |
63 | 45.2% of PTSD patients with pre-traumatic OCD had his- tory of childhood abuse. |
|
Van Kirk et al.,
2018 |
United States | Case study | Military personnel | Mid-40s | Male | 1 | Apparent functional overlap between OCD (Y-BOCSc) and PTSD (PCL-5i) symptoms. |
|
Franklin &
Raines, 2019 |
United States | Cross-sectional study |
Military personnel | 45.1 years old (mean age) |
Male and female |
117 | Significant overlap between PTSD and OCD symptoms according to self-report instruments (PCL-5i, DOCSj). |
|
Rossi et al.,
2020 |
Italy | Case study | Motor Vehicle Accident survivor | 35 years old | Male | 1 | OCD diagnosis (DSM-5k) with apparent treatment re- sponse to sertraline – aripiprazole. |
Notes:
aTreatment resistant OCD patient: Participants with failure of at least one adequate prior treatment trial or at least two types of medication trials.
bDSM-IV: Diagnostic and Statistical Manual of Mental Disorders Fourth Edition.
cYBOCS: Yale Brown Obsessive Compulsive Scale.
dOCI-R: Obsessive Compulsive Inventory-Revised.
ePDS: Posttraumatic Diagnostic Scale.
fDSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders Fourth Edition Text Revision.
gMINI: Mini International Neuropsychiatry Interview.
hDissociative Experiences Scale.
iPCL-5: Posttraumatic Stress Disorder for DSM-5.
jDOCS: Dimensional Obsessive-Compulsive Scale.
kDSM-5: Diagnostic and Statistical Manual of Mental Disorders Fifth Edition.
Table 2 Confidence of the synthesized findings graded according to the Joanna Briggs Institute’s ConQual approach
|
Population: Participants with overlapping clinical symptoms of both OCD and PTSD. Phenomena of interest: Overlap of OCD and PTSD symptomatology. Context: Participants of any age, sex, ethnicity, and culture that manifest comorbid OCD and PTSD symptoms | ||||
|---|---|---|---|---|
| Synthesized finding |
Type
of research |
Dependability | Credibility |
ConQual
score |
|
Clinical domains There seems to be a temporal and causal factor relating to the specific context and timing of trauma, since some symptom clusters manifest differ- ently according to the moment of experienced trauma. |
Observational and empirical |
Downgraded one level |
Downgraded one level |
Moderate |
|
Risk factors and other correlates Of interest, early life adversity such as sexual and interpersonal violence and other stressors like combat trauma seem to influence the development of both OCD and PTSD symptoms. |
Observational and empirical |
Downgraded one level |
Downgraded one level |
Moderate |
|
Prognostic factors It appears that when both psychopathologies concur that the overall prog- nosis is diminished. |
Observational and empirical |
Downgraded one level |
Downgraded one level |
Moderate |
|
Treatment approaches To date, no single clinical guideline or evidence- based recommendation exists that focuses on both entities when comorbid. Some reports show mixed results when employing pharmacological and psychosocial ap- proaches |
Observational and empirical |
Downgraded two levels |
Downgraded two levels |
Low |
Note: The downgrade of the main scores was due to common dependability issues across the included studies and owing to a mix of equivocal and unequivocal findings. For example, in most studies, the researchers had no acknowledgement of their influence on their or future research.
Clinical domains (n = 7)
Several of the included studies addressed phenomenological and symptomatic domains of OCD and PTSD symptoms in a variety of community samples. These reports were mostly comprised of observational studies or clinical cases. To start with, relatively recent literature has showcased PTSD patients that manifest cognitions such as compulsions that have been described to occur strictly within the context of trauma, and that these may not be necessarily indicative of a comorbid diagnosis of OCD (de Silva & Marks, 2001). Similarly, other researchers have noticed that adults with intrusive cognitions tend to be more aware of specific external or internal stimuli in comparison to other adults with obsessions. Also, it was observed that worry, as a dimensional cognition, tends to be more severe than dysfunction-generating obsessions (Langlois, Freeston, & Ladouceur, 2000). Coincidentally, mental images, a recurrent phenomenon in many anxiety disorders, tend to be portrayed as irrational in nature in OCD patients. In comparison, it is important to note that individuals with this diagnosis can also experience intrusive images associated with earlier trauma (Speckens et al., 2007). Likewise, checking behaviors, another symptomatic dimension in obsessive and anxiety disorders, have been noted in a sample of motor vehicle accident survivors with up to six months post-trauma (Ehring, Ehlers, & Glucksman, 2008). In regards to a possible temporal causality factor, another study found that nearly all OCD symptoms were more frequent or severe among posttraumatic OCD patients, with the exceptions of certain symptomatic domains, such as symmetry-seeking behaviors, hand washing, and hypersensitivity to specific sensory phenomena, and that these symptoms were more common in pretraumatic OCD (Fontenelle et al., 2012). In the same way, another study about civilian survivors of war found that compulsive washing was the most frequent and severe symptom in participants with high levels of PTSD symptoms (Morina et al., 2016). Likewise, some researchers found a similar thematic connection in an outpatient sample of veterans with OCD self-report. These results may show that some OCD symptom profiles could be similar to PTSD cognitive symptom clusters (e.g., feeling responsible for harm, and unacceptable violent, or sexual thoughts; Franklin & Raines, 2019).
Risk factors and other correlates (n = 9)
Several findings included in this review discussed the relevance of specific stressors that resulted in the development of OCD symptoms in PTSD patients. Of interest, an old case report describes an individual without previous overt psychopathology who, after experiencing combat stressors, underwent development of concurrent OCD and PTSD, showing classical symptoms, such as obsessions of violent nature, contamination, doubt, compulsive hand-washing, cleaning, checking, counting, touching, attempts to resist these compulsions, and other related phenomena (Pitman, 1993). Subsequently, another series of cases suggested that the course of each disorder may run a heterotypical course when comorbid, and that this may address a different, heterogeneous subtype of OCD resulting from trauma (Sasson et al., 2005). Also, in one of the largest studies to date, 52% of 365 individuals with previous OCD had at least one or more earlier traumatic events (Cromer, Schmidt, & Murphy, 2007). In contrast, a study found no apparent relationship between trauma, acute stress disorder, PTSD, or symptoms in patients with OCD when compared to control patients from the general population (Grabe et al., 2007). Afterwards, a brief report observed that a high proportion of individuals seeking treatment for resistant OCD showcased earlier history of childhood and adulthood interpersonal violence. Of these, incestuous childhood sexual abuse, witnessing violence, and a greater frequency of experienced traumatic experiences were taken into account as putatively predictive of higher PTSD severity (Gershuny et al., 2008). Ratifying the findings of this report, another study found that a history of childhood abuse was statistically more common amidst PTSD patients with pre-traumatic OCD than among their counterparts with post-traumatic OCD (Araújo et al., 2018). Other researchers found in their study sample that nearly half of their participants developed OCD symptoms following exposure to combat- or terror- related trauma, and that most of those eventually met criteria for full OCD (Nacasch et al., 2011). In the same vein, a case series of five Israeli veterans with no prior personal or family history of OCD or other psychiatric comorbidity who were diagnosed simultaneously with PTSD and OCD following combat trauma, described that OCD symptoms were initially related to the previous trauma, but then expanded to include other non-traumatic related triggers (Fostick et al., 2012). Incidentally, another group of investigators that studied peritraumatic fear, self-focused and other-focused disgust found out that self-focused disgust was related to contamination-based OCD symptoms, while peritraumatic fear and other-focused disgust was not significantly related with this type of phenomena (Badour, Bown, Adams, Bunaciu, & Feldner, 2012).
Prognostic factors (n = 6)
A small case series noted an apparent inverse relationship between symptom intensity in both conditions (when OCD symptoms lessen, symptoms of PTSD increase, and vice versa.). Likewise, the authors of this work discussed that targeting OCD (and perhaps PTSD) in isolation may hamper therapy effectiveness (Gershuny et al., 2003). Moreover, another study found a significant relationship between OCD and PTSD symptoms in clinical and non-clinical samples utilizing continuous ratings instruments like the Posttraumatic Diagnostic Scale and the Obsessive-Compulsive Inventory (Huppert et al., 2005). Of interest, another clinical case described a patient without earlier psychiatric comorbidities who developed PTSD, depression, and OCD after a work-related trauma. This patient scored 30 on the initial Yale Brown Obsessive-Compulsive Scale (YBOCS) and 24 on the Beck Depression Inventory. Then, he reported panic attack phenomena in trauma-related situations or when his OCD symptoms worsened. Curiously, the authors of this report commented that adequately dosed medications provided no response, including the use of fluoxetine, sertraline, citalopram, bupropion, paroxetine, and fluvoxamine (de Moraes, Torresan, Trench, & Torres, 2008). Another study that compared the clinical characteristics of OCD with and without comorbid PTSD in an outpatient sample also revealed a high prevalence of OCD symptom severity for the comorbid group when the severity was measured using multiple OCD symptom dimensions (Shavitt et al., 2010). Other researchers noticed that severe OCD symptoms were found in patients with a higher degree of dissociative symptoms. In this report, is was shown that YBOCS scores were significantly correlated to severity of dissociation, anxiety, depression, and traumatic phenomena (Semiz, Inanc, & Bezgin, 2014). Lastly, a naturalistic, seven-year, longitudinal OCD study reported that individuals with comorbid OCD and PTSD had more severe and impairing OCD symptoms, poorer insight, lower quality of life, and greater incidences of lifetime affective and substance use disorders at the baseline assessment (Ojserkis et al., 2017).
Treatment approaches (n = 3)
Although scarce, this section addresses few treatment modalities employed, or pondered, in patients with both comorbidities. Even if unclear, some studies have found that behavioral treatment of OCD (with or without pharmacological interventions) may be hampered by the presence of comorbid PTSD and may even be contraindicated, since this type of interventions have been shown to reactivate symptoms associated with the traumatic event (Gershuny, Baer, Jenike, Minichiello, & Wilhelm, 2002). Some researchers have also distinguished in a case series that an integrated treatment approach to address both OCD and PTSD symptoms through a cognitive-behavioral system (cognitive restructuring to modify trauma-related beliefs paired with exposure and prevention therapy for OCD symptoms) may be effective when there is a functional connection between both entities (Van Kirk et al., 2018). Lastly, a recent case study reported an apparent successful treatment approach with aripiprazole augmentation of sertraline (Rossi, Niolu, Siracusano, Rossi, & Di Lorenzo, 2020).
Discussion and conclusion
The aim of this work was to provide a comprehensive overview of empirical and observational research concerning the overlap between OCD and PTSD symptoms. The studies reviewed indicate that a functional relationship between trauma and the development of both PTSD and OCD symptoms in some clinical populations may exist (Knowles, Sripada, Defever, & Rauch, 2019). It should be noted that some reports have stated that the clinical features of OCD symptoms vary according to the timing of the traumatic experience, suggesting the possibility of a subtype of OCD (pretraumatic vs posttraumatic; Araújo et al., 2018). Also, in phenomenological terms, many studies have observed that some symptom clusters correlate with the natural history and severity of both comorbidities. For example, cognitions such as worry, which are common in both disorders, may be predictive of higher disfunction when compared to isolated OCD symptoms (Langlois et al., 2000). Likewise, dissociation, a common symptom in trauma survivors, may be a predictor of a poorer treatment outcome in patients with OCD (Semiz et al., 2014). Peritraumatic self-disgust was significantly related to contamination cognitions, and war survivors have been shown to have high prevalence of OCD symptoms (Badour et al., 2012). This functional overlap has been consistently observed in multiple reports and measured through validated and standardized self-report instruments. These findings have utmost importance regarding treatment outcomes, since this has been exemplified in a few studies that highlight the difficulties of managing both disorders when comorbid.
Thus, as a conclusion, we propose a functional connection between the symptoms of both disorders. This connection may be of considerable difficulty to distinguish when comorbid and could hamper the prognosis of some patients. Hence, we recommend that future research should cover this phenomenon in detail. These efforts may aim to optimize treatment modalities and focus on specific outcomes for this patient population that carries a great burden and, perhaps, may be underdiagnosed. More longitudinal and qualitative methodologies could be combined to offer a comprehensive picture of this phenomenon, taking into consideration the sociodemographic and psychosocial environment it is part of.
We would like to add that this revision was expanded from previous research and targeted specific outcomes of studies covering this topic, but it is not without its limitations. Firstly, data regarding this phenomenon is scarce, and the few reports that were included may be highly heterogenous in their demographical population and methodological approaches. Distinct instruments or measures to diagnose both disorders and their symptoms were employed in many studies, which limited our capacity to aggregate results. There was also an imbalance in sample sizes in the included reports, and therefore, we were limited to make any statistical comparisons across study groups. Secondly, while this phenomenon may be an emerging area of interest, it should be noted that the assumptions derived from this work cannot explain the complex mechanisms in which both disorders connect and manifest, which should also be a focus of future research. Thirdly, while we followed rigorous search methods to identify relevant papers, the review was limited only to published reports that we were able to locate. Lastly, the exclusion of research in other languages should also be taken in consideration even though our search aimed to include studies in any vernacular, making it possible that additional data that covers this topic exists but was not included in this review (i.e., because of publication bias). As a concluding remark, we would like to issue the possible overlap of symptoms in these disorders, seeing that both are associated with great burden and may be underdiagnosed.











 nueva página del texto (beta)
nueva página del texto (beta)