Introduction
The World Health Organization (WHO) has urged countries to invest in mental health services to address the emergence of massive psychosocial risks and the upcoming mental disorder crisis because of the COVID-19 pandemic. At the same time, it recognizes that the most vulnerable sectors include frontline health workers, who face an imminent risk of infection and various psycho-emotional demands that affect their psychological well-being and mental health (World Health Organization [WHO], 2020). It is a well-known fact that health systems worldwide were unprepared to cope with the number of seriously infected patients in this pandemic, particularly in certain low- and middle-income countries, where the lack of personnel, materials, and infrastructure is more serious than in highly developed countries (Bong et al., 2020). In particular, Latin America has proved to be vulnerable in the pandemic not only because of the number of infections with which it contributes to global statistics, but also because of the vulnerability of its health workers since, by August 23, 2020, in Mexico alone, 97,632 professionals had been infected in this sector and 1,410 had died from COVID-19 (Agren, 2020).
The demands or negative psychosocial stressors to which health workers have been exposed during the COVID-19 pandemic include fear of infection; infection of family members; weakening of the social fabric due to social distancing; lack of personal protective equipment, conflicts with safety protocols and the desire to help others; difficulty in maintaining healthy lifestyles, uncertainty due to the duration of the crisis and lack of vaccines; ethical conflicts regarding decision-making, social esteem, discrimination and violence by relatives of patients, and even attacks in the public thoroughfare (Chen et al., 2020; Organización Internacional del Trabajo, 2020; Toribio, 2020; Tsamakis et al., 2020; Wu, Styra, & Gold, 2020). Psychosocial factors at work can be understood as facts or conditions of work activity, which through pathogenic or salutogenic strees mechanisms, influence health and disease. There may therefore be negative psychosocial factors (or stressors) (psychosocial risk factors) and positive psychosocial factors (favorable or salutogenic resources), and the nature of their interaction or synergy is what determines the health-disease process (Juárez García & Camacho Ávila, 2011; Osorio Escobar, 2011).
Given the above, it should be noted that no studies were found that identified resources or positive psychosocial factors in health workers in epidemic situations, and even less so in the current context due to COVID-19, despite the fact that the most prominent models of psychosocial factors indicate the importance of exploring both the stressful demands and the protective resources available in the context of workers, not only at the diagnostic but also at the intervention level (Bakker & Demerouti, 2013). It is therefore an area of opportunity in current research to explore both factors and their relationship with mental health in these workers, which has become a priority and a major challenge during the COVID-19 pandemic (Badrfam, Zandifar, & Arbabi, 2020).
The consequences for the mental health of workers who work directly with COVID-19 patients are revealing. In China, the country where the pandemic originated, 50.4% of health workers have been found to have symptoms of depression, 44.6% anxiety, 35% insomnia and 71.5% distress (Lai et al., 2020), while another study found that 35.6% of Chinese health workers suffered generalized anxiety and 23.6% sleep problems (Huang & Zhao, 2020). Likewise, studies in other countries have shown that health workers who have provided medical care during the COVID-19 emergency report a higher prevalence of insomnia, anxiety, depression, somatization, and obsessive-compulsive symptoms than other health workers (Zhang et al., 2020). In countries such as India and Singapore, it was also found that just over 30% of the workers have somatic and physical discomfort (such as headaches, sore throats, tiredness, and insomnia) associated with mental health (Chew et al., 2020). Evidence also suggests that the pandemic itself may be an independent risk factor for stress in (Spoorthy, Pratapa, & Mahant, 2020) healthcare workers.
At the time of writing, in Latin America there are only articles for reflection and narrative reviews published on the mental health of health workers because of the COVID-19 pandemic and the psychosocial factors of the context possibly associated with them. In this respect, the identification of these psychosocial and mental health factors through empirical studies is important not only because they are indicators of alterations in themselves, but also because of their link with medical errors (Shanafelt et al., 2010), patient satisfaction (Stimpfel, Sloane, & Aiken, 2012), immune and endocrine (Mommersteeg, Heijnen, Kavelaars, & van Doornen, 2006), cardiovascular (Juárez-García, 2007), and musculoskeletal diseases (Ballester Arias & García, 2017), which have made health personnel more vulnerable.
Even before the pandemic, health personnel in Mexico had mental health indicators that attracted attention (Aguirre Hernández, López Flores, & Flores Flores, 2011). However, there have been no articles on whether these indicators have deteriorated or of their potentially specific psychosocial factors (whether these are negative stressors or positive protective resources), which may be associated with them in health workers in Mexico. Given the above, as part of a larger project in several Latin American countries, the purpose of this study was to identify the levels of stress, burnout, anxiety, and depression, and their possible relationship with negative psychosocial stressors and positive psychosocial resources in a sample of health workers in Mexico during the COVID-19 pandemic.
Method
Study design and participants
Two hundred and sixty-nine health workers from various COVID clinics and hospital centers in Mexico located in the states of Morelos (n = 89, 33.1%), Mexico City (n = 80, 29.7%), State of Mexico (n = 66, 24.5%) and other states (n = 34, 12.6%), such as Aguascalientes, Guerrero, Hidalgo, Michoacan, San Luis Potosi, Oaxaca, Puebla, and Yucatan, participated in a study with a non-experimental, transactional, correlational design. Table 1 shows the sociodemographic characteristics of the subjects (Table 1).
Table 1 Sociodemographic profile of subjects
| Variable | n | % |
|---|---|---|
| Age | ||
| Up to 32 years | 68 | 25.3 |
| 33-39 years | 80 | 29.7 |
| 40-46 years | 59 | 21.9 |
| Over 47 years | 62 | 23 |
| Sex | ||
| Male | 65 | 24.2 |
| Female | 203 | 75.5 |
| Did not wish to specify | 1 | .4 |
| Marital status | ||
| Single | 84 | 31.2 |
| Married | 120 | 44.6 |
| Living together | 44 | 16.4 |
| Separated or widowed | 21 | 7.8 |
| Educational attainment age | ||
| High school or technical school | 36 | 13.4 |
| Bachelor’s degree | 114 | 42.4 |
| Master’s or specialty | 113 | 42.0 |
| Doctorate | 6 | 2.2 |
| Sector | ||
| Public | 230 | 85.5 |
| Private | 16 | 5.9 |
| Both | 23 | 8.6 |
| Seniority | ||
| Up to 7 years | 91 | 33.8 |
| 8 to 15 years | 102 | 37.9 |
| 16 years or over | 76 | 28.3 |
| State | ||
| Morelos | 89 | 33.1 |
| State of Mexico | 66 | 24.5 |
| Mexico City | 80 | 29.7 |
| Other | 34 | 12.6 |
| Position | ||
| Medical personnel | 110 | 40.89 |
| Nursing | 70 | 26.02 |
| Operating staff | 34 | 12.64 |
| Administrative personnel | 38 | 14.13 |
| Various health professions | 17 | 6.32 |
| Area | ||
| Administration | 41 | 15.24 |
| Consultation | 77 | 28.62 |
| Hospitalization | 30 | 11.15 |
| Surgery | 15 | 5.58 |
| Laboratory | 23 | 8.55 |
| Emergencies | 47 | 17.47 |
| ICU | 9 | 3.35 |
| Other | 27 | 10.04 |
Within the framework of the health emergency declared by federal authorities in Mexico, all personnel who took part in the study were invited to participate non-randomly and virtually through directed sampling using the snowball strategy, through the contact networks of the authors of this article, using emails, social networks, and other virtual means. They were asked to share the survey with their work colleagues and acquaintances in the health field, and no face-to-face questionnaires were administered. Data collection took place between June and July 2020.
Instruments
Negative stress, burnout or emotional exhaustion, anxiety, and depression were evaluated as mental health outcome variables using previously validated brief or single-item versions. In the case of stress, the item used (“Stress means a situation in which a person feels tense, restless, nervous, anxious or has trouble sleeping, because they are preoccupied all the time. Have you felt like this recently?”) has shown moderate correlations with various indicators of mental health (.24-.75) and job demands (.15-.30), as well as discriminant and content validity (Elo, Leppänen, & Jahkola, 2003). The item has five answer options ranging from “hardly at all” (1) to “a lot” (5). Three was chosen as the cut-off point when representing the theoretical mean on the scale.
For burnout, the item “Please choose the option that is closest to what you currently feel. (Here BURNOUT refers to feeling mentally and physically exhausted, as if work had wiped you out)”, has shown theoretically consistent structural relationships of moderate magnitude with coping and the Maslach Burnout Inventory (.58 -.63) (Merino-Soto, Juárez-García, Altamirano-Bringas, & Velarde-Mercado, 2018). The item has five answer options ranging from “I enjoy my work. I don’t have burnout” (1), to “I feel completely burned out and often wonder whether I can recover. I’m at the point where I need to make changes or seek some kind of help” (5). Three was chosen as the cut-off point when representing the theoretical mean on the scale and an important symptomatology: (3) “I definitely feel burnout and have one or more of its symptoms, such as emotional or physical exhaustion.”
To evaluate anxiety and depression, the ultra-brief version of the Patient Health Questionnaire (PHQ-4 items) was used, which has shown a satisfactory factorial structure and inter-correlations with various mental health criteria (Löwe et al., 2010). The scale contains four answer options ranging from “not at all” (0) to “nearly every day” (3). The cut-off point chosen was “more than half of all days” (2), because it was in the theoretical mean.
A sociodemographic section and five ad hoc questions developed by the authors of this article were included as well as questions on the status of health personnel in relation to the COVID-19 pandemic: 1. “For approximately how many weeks have you attended patients in connection with the SARS-CoV-2 / COVID-19 pandemic? (Mark 0 if you have not seen patients),” 2. “On average, how many suspected or confirmed cases of SARS-CoV-2/COVID-19 do you have contact with per week? (Mark 0 if you have not treated patients),” 3. “Do you suffer from any chronic disease?,” 4. “Have you presented symptoms or been diagnosed with COVID-19?,” and 5. “Have you suffered the loss of a family member or close friend or colleague due to COVID-19?”
In the last section, a mixed simultaneous qualitative-quantitative exploration technique was used to obtain information on the psychosocial factors experienced by workers in highly specific contexts, which has already been used in other studies (Flores-Jiménez & Juárez-García, 2016; Juárez-García, Flores-Jiménez, & Pelcastre-Villafuerte, 2020). This heuristic methodological approach explores negative (stressors) and positive (resources) psychosocial factors through an open- question format, which were as follows for this study: “What aspects cause you the most stress in this pandemic?” and “What are the resources or supports you have to cope with the stress of this pandemic?” These questions or prompts also include the instruction to mark the frequency with which they are experienced on a Likert-type scale (from 1 = never or rarely, to 5 = always, every day). In keeping with the technique, answers are recorded on an Excel sheet and a group of at least three judges subsequently carry out a discussion and the open, hierarchical coding and categorization of the answers obtained until emerging categories are defined, based on an inductive logic. Once the categories and their frequencies have been obtained, and exported to any statistical program, the quantitative statistical associations with the outcome variables are estimated, using the categories as dichotomous variables and the Likert frequencies obtained within the categories as continuous variables (Flores-Jiménez & Juárez-García, 2016; Juárez García, Flores, & Hindrichs, 2019).
Results analysis strategy
Regarding the psychosocial factors (stressors and resources) obtained in a quali-quantitative way, the open questions were characterized by three judges (the first three authors of this article) and frequencies of the aforementioned categories were obtained, together with the means and standard deviations of the frequencies of exposure indicated on the Likert scale. Statistical associations between the factors obtained and outcome variables (burnout, stress, depression, and anxiety) were estimated using two means or strategies: first, using the Spearman correlation coefficient (rs) to estimate the correlation between the mental health variables and the intensity of exposure (Likert scale) within each category; and then considering the variables as categorical for the entire sample (0 = did not mention it, 1 = did mention it), through the Phi (Φ) coefficient, which is considered an implicit measure of effect size (Cohen, 1988). This strategy would enable us to explore the possible harmfulness of these factors for health at two levels: either the mere effect of their absence or presence on the entire sample or the magnitude of their effects according to their frequency of exposure indicated on the Likert scale (dose-response effect), the latter only being used for those who indicated this specific factor (JuárezGarcía et al., 2019). Within this same step, the association between mental health and the variables of the subjects’ personal status regarding COVID-19 (presence of symptoms or diagnosis of COVID-19, loss of a family member or person close to them, number of weeks and number of patients treated) were calculated using the point biserial correlation coefficient for the former (bivariate categorical and continuous relationship) (Palmer, Jiménez, & Montaño, 2000) and r Spearman (rs) for the last two (ordinal variables).
Finally, to identify a possible structure of the simultaneous relationships between the psychosocial variables or categories obtained, a cluster analysis was conducted using the hierarchical method, a multivariate technique suitable for exploring and characterizing multivariate relationships between categorical variables that are unsuitable for factor analysis and where it is not known whether such relationships are linear (Justus & Uma, 2016). For a more parsimonious exploration, one dendrogram was created separately for negative stressors and another for positive resources.
The “furthest neighbor” grouping method was used, which helps to build compact clusters and detect distant (atypical) data in large sets of variables (Vilà Baños, Rubio Hurtado, Berlanga Silvente, & Torrado Fonseca, 2014). As a measure of similarity between categories, the four-point Phi Φ coefficient was used, which is a binary version of Pearson’s correlation coefficient as a measure of distances in categorical variables (Pardo Merino & Ruiz Diaz, 2002).
Ethical considerations
Participation in the study was strictly voluntary and potential subjects were informed of the nature and objectives of the research; this informed consent was shown at the beginning of the survey. Virtual data collection guaranteed the safety of subjects and researchers by ensuring social distancing, required by health authorities during the pandemic. The autonomy, anonymity, and confidentiality of subjects were guaranteed by not requesting any name or identifier in the survey and informing participants that they were free to start or stop answering the survey at any time as they wished. The nature of the study meant there were no invasive procedures. At the end of the survey, a directory of eight direct contacts of psychological care centers was provided if, based on subjects’ responses, they wished to receive a more in-depth evaluation or psychological assistance in general. As a benefit to the subjects, it is hoped that information derived from the research will help health institutions develop and implement intervention strategies that consider the relevance of psychosocial risk factors or protective factors identified in the current emergency context due to COVID-19.
The general project protocol was approved by the ethics committee of the Center for Transdisciplinary Research in Psychology of the Autonomous University of the State of Morelos (Universidad Autónoma del Estado de Morelos, UAEM) with folio 161220-50. At all times, the guidelines for research on human beings established in the Declaration of Helsinki (World Medical Association [AMM], 2013) and Article 21 of the Regulations of the General Health Law in Mexico (Secretaría de Salud, 1987) were followed.
Results
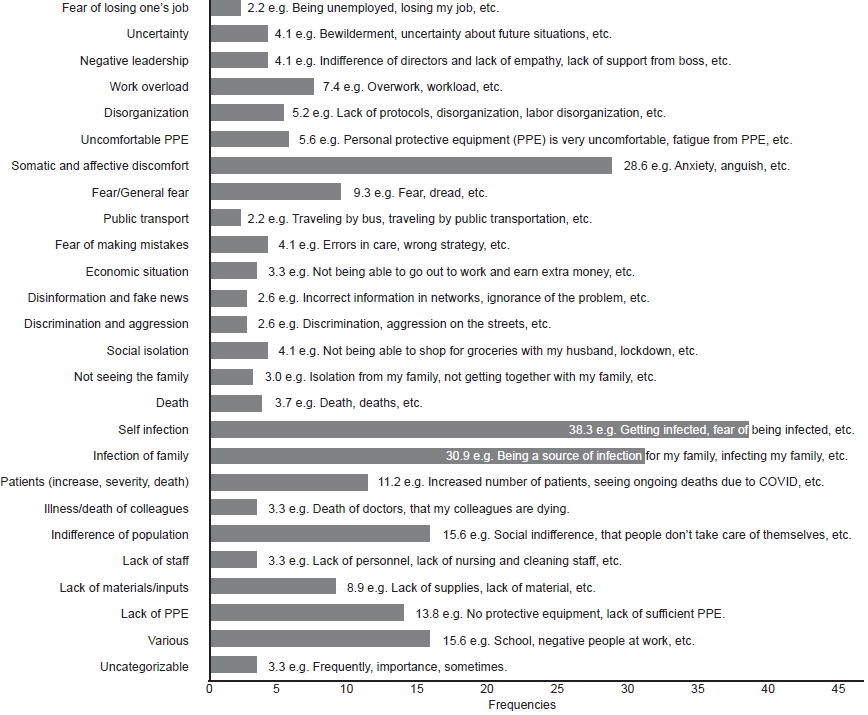
Regarding the main stressors or negative psychosocial factors cited by those evaluated, those who mentioned a minimum of five times were considered, yielding 25 factors or categories and one “uncategorizable” one (incoherent or misunderstood the instructions). The most frequently mentioned stressors were grouped into the categories of “infection of self” (38.3%), “infection of the family” (30.9%), and “somatic and affective discomfort” (28.6%) (Figure 1). As for positive psychosocial factors or resources, 21 categories were mentioned together with one “uncategorizable” one. The most frequently mentioned ones were “the family” (34.6%), “availability of) personal protective equipment” (24.5%), “receiving psychological care” (16.7%), “training” (15.6%), and interestingly, “none” (16.7 %), which could be a negative aspect (Figure 2).

Figure 2 Psychosocial resources mentioned by health care workers during COVID-19 pandemic (percentages).
Likewise, it was found that 24.5% of the health workers in the sample suffer from a chronic disease, 14.5% have symptoms or have been diagnosed with COVID-19, and 55.8% have experienced the loss of a family member or someone close to them because of this disease. 69.6% had seen an average of 11.84 COVID-19 patients per week, with an average of 6.16 weeks of care at the time of the study (Table 2). The frequencies of high levels of the outcome variables were striking, with 56.9% for depression (X̄ = 1.93), 74.7% (X̄ = 2.26) for anxiety, 49.8% (X̄ = 2.61) for burnout, and 46.8% (X̄ = 3.31) for negative stress.
Table 2 Association between mental health variables and psychosocial categories in health workers during COVID-19 Pandemic (strategy 1, continuous variables, Likert scale, n = variable)
| Valence | Categories | N = Mentions |
Exposure factor X̄ (SD) |
Mental health rs (α =) | |||
|---|---|---|---|---|---|---|---|
| Depression | Anxiety | Burnout | Stress | ||||
| Negative psychosocial factors |
Various | 42 | 3.85 (.94) | .32* (.03) | .38 (.01)** | .52 (.00)*** | .34 (.02)* |
| Lack of materials/inputs | 24 | 4.29 (.75) | .38 (.06) | .41 (.04)* | .50 (.01)** | .52 (.00)** | |
| Illness/death of colleagues | 9 | 4.11 (.78) | .73 (.02)* | .57 (.10) | .46 (.20) | .59 (.08) | |
| Patients (increase, complication, etc.) | 30 | 4.03 (.77) | .45 (.01)** | .75 (.00)*** | .39 (.03)* | .48 (.00)** | |
| Infection of family member | 83 | 4.34 (.79) | .36 (.00)*** | .34 (.00)** | .32 (.00)** | .19 (.08) | |
| Infection of self | 103 | 4.22 (.78) | .36 (00)*** | .43 (.00)*** | .75 (.00)*** | .43 (.00)*** | |
| Death | 10 | 3.70 (.67) | .84 (.00)** | .70 (.02)* | .75 (.01)** | .46 (.17) | |
| Fear/general fear | 25 | 3.76 (.83) | .10 (.61) | .18 (.39) | .22 (.28) | .47 (.01)** | |
| Somatic and affective discomfort | 77 | 3.63 (.80) | .34 (.00)** | .40 (.00)*** | .51 (.00)*** | .60 (.00)*** | |
| Work overload | 20 | 4.00 (.85) | .50 (.02)* | .60 (.00)** | .30 (.18) | .75 (.00)*** | |
| Positive psychosocial factors |
Personal protective equipment | 66 | 3.69 (1.14) | -.23* | -.14 | -.11 | -.01 |
| Support of superiors | 26 | 3.57 (1.35) | -.59 (.00)** | -.46 (.01)** | -.45 (.01)** | -.56 (.00)** | |
| Recreational activities at home | 7 | 4.28 (.75) | .63 (.12) | .82 (.02)* | .00 (00) | .80 (.02)* | |
| Healthy habits | 41 | 3.73 (.71) | -.31 (.04)* | -.08 (.60) | -.12 (.42) | -.20 (.19) | |
| Religiosity/spirituality | 22 | 4.63 (.65) | .15 (.49) | .53 (.01)** | .24 (.27) | .46 (.02)* | |
| Personal COVID-19 status |
Has chronic disease (yes) | 66 | 24.5% | .13 (.03)* | .11 (.07) | .10 (.07) | .14* (.01) |
| Has presented symptoms or been diagnosed with COVID-19 (yes) |
39 | 14.5% | .13 (.03)* | .12 (.03)* | .14 (.01)** | .08 (.15) | |
| Loss of a relative, close friend or colleague due to COVID-19 (yes) |
50 | 55.8% | .16 (.00)** | .19 (.00)** | .19 (.00)** | .25 (.00)*** | |
| No. of weeks attending COVID-19 patients |
206 (69.6%) attended |
6.16 (4.80) | .07 (.23) | .11 (.06) | .14 (.02)* | .06 (.28) | |
| No. of COVID-19 patients per week |
206 (69.6%) attended |
11.84 (22.08) | .06 (.26) | .10 (.10) | .12 (.04)* | .05 (.38) | |
| Mental health indicators |
Depression | 56.9% | 1.93 (.81) | 1.00 | .66 (.00)*** | .54** (00)*** | .65 (.00)*** |
| Anxiety | 74.7% | 2.26 (.88) | 1.00 | .55 (.00)*** | .74 (.00)*** | ||
| Burnout | 49.8% | 2.61 (1.07) | 1.00 | .65 (.00)*** | |||
| Negative stress | 46.8% | 3.31 (1.29) | 1.00 | ||||
Notes:
***p < .001,
**p < .01,
**p < .05.
Regarding the association of these mental health outcomes with psychosocial factors, the first strategy, related to the correlation of the frequency or intensity of exposure and mental health, found at least one statistically significant association with moderate to high magnitudes with the factors of: “lack of materials/supplies,” “illness/death of colleagues,” “patients,” “infection of a family member,” “infection of oneself,” “death, “general fear/fear,” “somatic and affective ailments,” “work overload,” and “various.” All these relationships were in the theoretically expected directions. Regarding positive psychosocial resources, statistically significant relationships were found with moderate to high magnitudes in the cases of “(availability of) personal protective equipment,” “support from superiors,” “healthy habits,” “recreational activities in the home,” and “religiosity and spirituality,” although the last two were not in the expected direction (Table 2).
Table 2 shows the correlations between mental health and COVID-19 personal status variables (chronic disease, COVID-19 symptoms or diagnosis, number of weeks and COVID-19 patients treated, loss of a relative or close person), which were mostly statistically significant. However, the last one showed the highest correlations (Φ = .16 - .25) and therefore the greatest effect on mental health. It is worth noting that, as expected, the four mental health outcomes were significantly associated with each other with moderate to high correlations (rs = .54 - .74).
In the second strategy to analyze the relationship between mental health and psychosocial factors mentioned previously (categorical variables, n = total), significant associations emerged with at least one mental health link for stressors: “lack of personal protective equipment,” “patients,” “financial situation,” “general fear/fear,” “negative leadership,” and “social isolation,” although the latter showed a negative correlation, in other words, it seemed to have a protective effect. The resources or positive factors that proved significant were: “personal resources,” “supplies and protective materials,” “training,” “listening to music, reading, etc.” and strikingly, “none,” which showed inverse correlations, which were nonetheless theoretically feasible as regards what might be expected. In general, the correlations of the factors categorized as resources were of magnitudes that could be considered low or very low (Cohen, 1988) (Table 3).
Table 3 Association between mental health indicators and psychosocial categories in health workers during COVID-19 pandemic (strategy 2, categoric variables, n = 269)
| Valence | Category | Mental health (categories) Φ (α =) | |||
|---|---|---|---|---|---|
| Depression | Anxiety | Burnout | Stress | ||
| Negative psychosocial factors |
Lack of personal protective equipment | .10 (.07) | .13 (.02)* | .03 (.61) | .01 (.81) |
| Patients (increase, complication, etc.) | .11 (.05)* | -.01 (.85) | .00 (.98) | .04 (.45) | |
| Social isolation | -.16 (.00)*** | -.13 (.02)* | .09 (.12) | -.08 (.18) | |
| Financial status | .12 (.04)* | .01 (.83) | .10 (.08) | .11 (.05)* | |
| Fear/general fear | -.03 (.60) | .06 (.26) | -.01 (.84) | .13 (.02)* | |
| Negative leadership | .06 (.27) | .03 (.58) | .13 (.03)* | .03 (.60) | |
| Positive psychosocial factors |
Personal resources | -.13 (.03) | -.10 (.08) | -.03 (.61) | -.07 (.19) |
| Inputs and protective materials | -.08 (.16) | -.02 (.64) | -.15 (.01)** | -.10 (.07) | |
| None | .10 (.07) | .10 (.10) | .19 (.00)** | .17 (.00)** | |
| Training | -.14 (.01)** | -.15 (.01) | -.16 (.00)** | .07 (.21) | |
| Listening to music, reading, videos, social networks |
-.04 (.49) | -.13 (.02)* | -.08 (.18) | -.01 (.75) | |
Notes:
***p < .001,
**p < .01,
*p < .05.
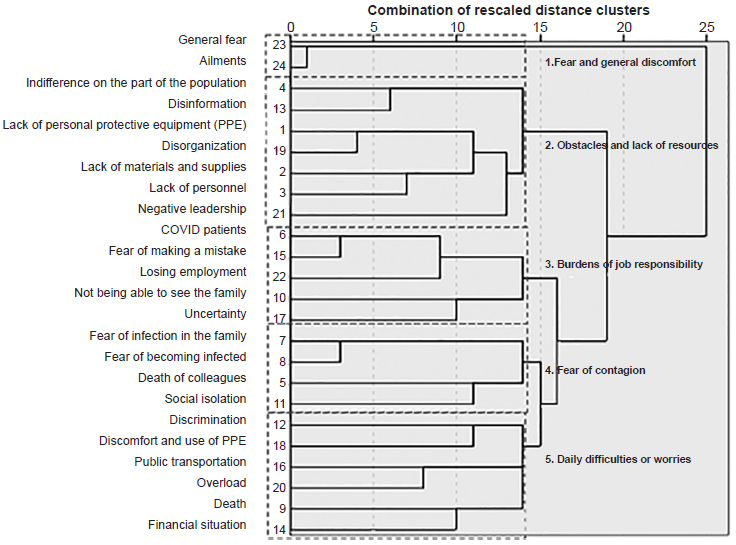
Finally, the hierarchical cluster analysis showed large distances between the different categories, both in negative psychosocial stressors and positive psychosocial resources, which would mean that in general they are dissimilar categories and extremely orthogonal. Given the number of variables, we proceeded to exclude the categories of “other” and “uncategorizable,” which, in fact, would have proved difficult to interpret theoretically. In the case of stressors, using the criterion of the greatest percentage change in distances (Justus & Uma, 2016), and mainly a viable theoretical interpretation, stage 14 seemed the most appropriate for the cluster formation cut-off, so the dendrogram made it possible to identify five clusters of stressors that could concentrate the main negative factors in terms of a more representative structure, which could be called: 1. “fear and general discomfort,” 2. “obstacles and lack of resources,” 3. “burdens of work responsibility,” 4. “fear of infection,” and 5. “everyday difficulties” (Figure 3).
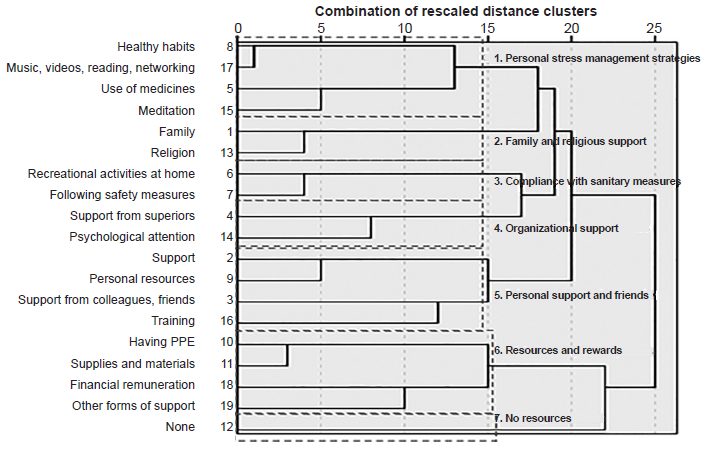
Regarding positive psychosocial resources, the criterion of percentage change in distances suggested that the determination of clusters could occur in stage six. However, in that case, there were 11 clusters that not only failed to contain any possible theoretical interpretation, but the integration of categories was too poor to summarize the data in a more representative structure. In this way, using the second most important percentage change in stage 16 as a criterion, a structure of seven theoretically viable clusters of psychosocial resources was identified, which could be called: 1. “individual anti-stress strategies,” 2. “family and religious support,” 3. “compliance with health measures,” 4. “organizational support,” 5. “personal support and support from friends,” 6. “resources and rewards,” and 7. “no resources” (Figure 4).
Discussion and conclusion
The aim of this study was to identify the levels of stress, burnout, anxiety, and depression and their relationship with negative and positive psychosocial factors perceived by health workers in Mexico during the current contingency caused by the global COVID-19 pandemic. The results confirm the high levels expected in the symptoms of depression, stress, burnout, and anxiety, particularly the latter, which presents the most worrying levels (74.7%). These findings coincide with those reported in other countries such as China, where approximately 50% of the health workers presented generalized anxiety, depression, and over 70% negative stress, among other mental health disorders, which has been recurrently reported in several studies (Lai et al., 2020; Huang & Zhao, 2020; Zhang et al., 2020).
It is worth highlighting the results of the aspects evaluated of the personal status of health workers during the COVID-19 pandemic. For example, although they are frontline workers during this contingency, 24.5% admitted that they have a chronic disease, which entails an implicit danger to life that is being assumed due to the serious risk of being infected by this disease. This is significant because of its possible link to the fact that Mexico ranks first in the number of health workers who have died from COVID-19 (Agren, 2020). Moreover, those who reported these diseases also showed a statistically significant relationship with higher scores for symptoms of depression and stress, which creates a vicious circle between physical and mental vulnerability. Likewise, the relationship between burnout scores and the number of weeks and COVID-19 patients seen confirms the cumulative attrition at this stage of the contingency and is seen as a time bomb in the mental health of the health sector workforce. One of the most striking and telling data on this issue is that at the time of the study, 55.8% of health workers mentioned having lost a family member, colleague, or person close to them to COVID-19, which was obviously related to all the mental health indicators and reflected the heavy psychological and affective burden the health sector is experiencing in this pandemic in Mexico.
Regarding psychosocial factors, subjects mentioned a broad array of stressors and specific resources, which in turn were differentially associated with mental health. Regarding negative factors or stressors, although the frequency of mention would suggest that the main stressors were “self-infection,” “infection in the family,” or “somatic and affective ailments,” the greatest harm seemed to be caused by the frequency of exposure to stressors such as “work overload,” “patients,” “illness / death of colleagues” or “death,” which were precisely those that displayed the highest association coefficients with negative mental health (Table 2). The last two show an even greater trend in effect sizes (rs = .46 - .84), so it is necessary to consider their harmfulness to some extent for the four mental health indicators (depression, anxiety, burnout, and stress), regardless of their statistical significance. This makes it possible to highlight the emotional demands associated with illness and death which, together with the workload, are psychologically exhausting health workers during this contingency and may constitute the initial framework of future post-traumatic alterations and post-pandemic suicide risks expected by international authorities in health personnel (United Nations [UN], 2020).
In the case of the analysis by categorical variables, it is perhaps only worth highlighting “economic status” which was weakly related to at least two mental health variables (depression and stress) and shows one of the stressors common to the general population. One correlation found in an unexpected direction concerned social isolation, which despite its low magnitude, indicated that the greater the isolation, the lower the depression and anxiety. An initial interpretation in this regard could be that social isolation reduces the perception of risk of infection and therefore cushions negative mental health symptoms, which could be partly validated by locating these variables in the same cluster called “fear of infection” (Figure 3). However, future studies are required to confirm this interpretation.
At the same time, although the most frequently mentioned positive psychosocial resources were those located in the categories of “family,” “personal protective equipment” and “companionship and friends,” the resource that seems to have the greatest protective effect was “support of superiors,” which showed the highest coefficients or effects in its relationship with all the mental health variables. This highlights the need to include complementary intervention strategies focused on positive or protective factors, but above all, to consider changes in the organizational contexts and the improvement of institutional leadership as intervention strategies in addition to the single individual psychological supports currently provided for health workers during this health emergency. It is worth mentioning that positive strategies should not replace the mental health care initiatives of those who are already suffering and receiving treatment for stress, burnout, anxiety, or depression, but rather that all these strategies should be complementary. It is worth noting that the relationships in unexpected directions of the variables of “recreational activities at home” and “religiosity / spirituality” with poorer mental health may reflect coping strategies which people at high risk are using to cope with the deterioration they are suffering (anxiety and stress lead them to seek recreational activities at home or religious behaviors to reduce them), which seems clinically possible. However, it is impossible to confirm this interpretation with the data from this study.
Regarding the methodological aspects and analysis strategies in this research the strategy of bivariate correlations with the variables in categorical format showed, interestingly few significant relationships, with very low magnitudes and they were dissimilar to those that proved significant by exploring relationships with frequencies of exposure in continuous variables (Tables 2 and 3). One possible explanation for these differences is the foreseeable weakness of the statistical power in categorical variables, but above all, the possible increase in error variance when assuming the equivalence of measurement in the categories defined by the “absence-presence” value (0, 1) according to the reports of the subjects, as well as the possible incompatibility of the meaning and accuracy of the classification made by the judges in relation to the perception of those evaluated. These limitations were not foreseeable when first used in this study and are potential areas for future exploration regarding the usefulness of the technique used. Despite these weaknesses, the technique uses the benefits of qualitative methodology and combines them with quantitative methodology, creating an extremely robust mixed method that made it possible to identify highly specific stressors and psychosocial resources present in the contexts of the COVID-19 pandemic faced by health personnel. They also help identify their potentially harmful or protective role in mental health, where there is an obvious lack of standardized instruments that would make it possible to specifically assess such factors and their effects on the well-being and psychological health of these workers.
Although it was not a primary objective of this work, cluster analysis made it possible to identify possible sub-groups in the psychosocial categories based on their relationships with each other, and to glimpse possible structures and more general factors that can serve as conceptual frameworks for developing future standardized instruments that evaluate stressors and resources during situations of massive epidemics in health personnel, which is an additional contribution of the present study.
The main limitations of this work are that the results are susceptible to a margin of bias due to the sampling strategy used. In addition to being slightly under-representative, this strategy does not enable one to determine whether the data obtained are overestimated, when answers are obtained from participants who wish to be listened to during their current work situation or whether they are underestimated. The latter could be explained by the fact that answers tended to be obtained from workers with a lower workload, which enabled them to answer the questionnaire, thus excluding workers with an excessive workload or emerging responsibilities (such as caring for infected patients) that forced them to decline our invitation. Additionally, pandemic conditions made it impossible to include a detailed qualitative exploration through interviews or focus groups in this study that could facilitate the interpretation of results, as well as the answers of subjects. Despite these limitations, findings are similar to other studies with large samples and the theoretical coherence of most of the results justify their potential usefulness for consideration in preventive mental health programs for health personnel coping with the COVID-19 pandemic.











 nueva página del texto (beta)
nueva página del texto (beta)