Introduction
Providing health services to the entire population and ensuring financial protection is one of the main objectives of a health system. The 2030 Sustainable Development Goals highlight the importance of protection against financial risks as part of a universal health coverage (Union Nations Organization, 2012). Mental disorders have an economic impact on the labor productivity of individuals, so that investing in them influences economic growth, hence the importance of evidencing which interventions must be adopted so that the health system manages to provide necessary services for the entire population. This means that interventions should be cost-effective, feasible, and affordable (World Health Organization, 2013).
In low and middle income countries, it is particularly difficult to decide which interventions should be included in the service packages in the absence of cost-effectiveness evidence. In this sense, interventions that include typical and/or atypical antipsychotic medication and psychosocial treatment are considered affordable, feasible, and effective (Patel, 2016; Chisholm & Saxena, 2012). Applying these interventions would contribute to reducing the gap in mental health care, which in Latin America is currently from 58.0 to 44.4% (Kohn et al., 2005).
In Mexico, since 2003, the Social Protection System in Health (SPSS, initials for Sistema de Protección Social en Salud) in Spanish was established. Its main objective is to guarantee the financial protection of the population without social security. The SPSS provides health care services in the first and second levels of care through “Popular Insurance” (SP, initials of Seguro Popular). The health interventions for psychotic disorders (schizophrenia, delusions and schizotypal disorder) include a quarterly consultation, one to two annual hospitalizations, antipsychotic medication (risperidone, olanzapine, haloperidol, perphenazine, quetiapine, clozapine, levomepromazine, aripiprazole, trifluoperazine), and auxiliary diagnostic studies (laboratory and imaging) (Secretaría de Salud, 2005). Those interventions were integrated on the basis of recommendations from the WHO CHOICE project whose objective is to provide information on cost-effective interventions based on three key criteria: public health burden and importance; the availability of effective and potentially profitable interventions; and the availability of data on epidemiology, clinical effectiveness, use of resources and costs (Chisholm, 2005).
The cost-effectiveness analysis is an adequate economic evaluation method to provide relevant information to decide which interventions should be adopted. In Mexico there have been few cost-effectiveness studies of the interventions for the treatment of schizophrenia. For example, the evaluation of the effectiveness of different care strategies reported that psychosocial intervention without medication is less cost-effective than a comprehensive care strategy (psychosocial treatment + antipsychotic medication + psychoeducational treatment) and even interventions in which the hospital provided antipsychotic medication (Cabello-Rangel, Díaz-Castro, & Arredondo, 2011). Another study considered the effectiveness as DALYS avoided based on a hypothetical coverage of 80% the cost of DALY avoided was $ 1,135,516. 00 Mexican pesos, with antipsychotic treatment only, when adding psychosocial treatment, the cost is $ 390,892.00 Mexican pesos (Lara-Muñoz et al., 2010).
The extended cost effectiveness analysis (ECEA) approach stems from the idea of providing protection against financial risks and consequently distribution of health benefits in population subgroups (quintiles), that is, it assesses the cost-effectiveness effect of a Universal Public Finance (UPF). It is a method that incorporates financial protection measures within economic evaluations of health policies. Its fundamental premises is that the UPF reduces the private expense and may influence the equalization between income groups for both financial and health outcomes (Verguet, Laxminarayan, & Jamison, 2015).
The objective of this work is to perform an extended cost-effectiveness analysis and pharmacological and psychosocial treatment interventions afore mentioned for patients diagnosed with schizophrenia, as well as “Early Intervention in Psychosis Program” (EIP).
The EIP is a novel program of psychiatric hospital to treat first episode of psychosis with the aim of reducing medical and social complications as well as the comorbidities which flourish as a long-term result of the first episode of psychosis, through efficient treatment, focused on the patient and the family, the intervention of social workers, clinical psychologists, psychiatry and specialized nurses is necessary. Similar programs have been established and evaluated in other countries (McCrone, Knapp, & Dhanasiri, 2009). Therefore, it is of interest to evaluate them considering the available resources of an economic middle-income country.
Method
An extended cost-effectiveness analysis study (ECEA) was designed in which the variable and fixed costs of outpatient care for schizophrenia interventions were analyzed and quantified. This is an atypical or typical antipsychotic medication and psychosocial treatment; in this model all medications will be provided to the patient.
Interventions
Intervention 1 (T1): Typical or atypical antipsychotic with same effectiveness (haloperidol 5 mg and/or risperidone 2mg) + biperiden 2mg + basic psychosocial treatment (outpatient).
Intervention 2 (T2): Atypical antipsychotic (olanza- pine 10mg) + basic psychosocial treatment (outpatient).
Intervention 3 (T3): Atypical antipsychotic (olanza-pine 10mg) + Early Intervention in Psychosis Program that includes: 1. intensive stage: management of the prodromal stage, acute and recovery of psychotic syndrome that includes psychiatric, and psychotherapeutic treatment for the patient and the family for nine months. 2. follow-up stage: scheduled appointments on a regular basis, but with a longer time interval, to monitor the established treatment.
Variables
Following the method developed by Verguet, the ECEA is based on a hypothetical population of one million inhabitants distributed in quintiles of 200,000 people, in which parameters that are assumed, and others used in previously published studies are applied, the risk aversion coefficient was estimated at 3% (Verguet et al., 2015). According to the Institute for Health Metrics, the weight of disability for chronic cases is .576 and for acute cases .756, and the estimated prevalence for schizophrenia in Mexico is .22%, according to the latest reports (Institute for Health Metrics, 2010).
The effectiveness of antipsychotic and psychosocial treatments is 46% and 49% for haloperidol and/or risperi-done and olanzapine, respectively, at an equivalent dose of 15 mg/day of haloperidol (olanzapine 20 mg/day or risperidone 4 mg/day) (Leucht, Pitschel-Walz, Abraham, & Kissling, 1999). Adherence to treatment is 76% for all interventions (Chatterjee et al., 2014; Thieda, Beard, Richter, & Kane, 2003). Early intervention in psychosis has a therapeutic adherence of 53% (Solmi et al., 2018).
The percentage of current coverage of care by quintile and the Gross National Income per capita (GNI) is US $ 815.61; the participation in the GNI by income of quintile is 5.4% on the lowest and 52.2% on the highest, which represents that the lowest quintile of the population has a weighted income of US $ 398.90 and the highest quintile of US $ 3859.08, for the year 2014, so that a population of one million inhabitants would have an income of US $ 851,660,000.00 and was based on that reported for Mexico by the World Bank (World Bank, 2018) (Table 1).
Table 1 Variables for model Extend Cost-Effectiveness Analysis (ECEA)
| Inputs | Value | Reference | ||||
|---|---|---|---|---|---|---|
| Demography inputs | ||||||
| Cohort size | 1000000 | |||||
| I | II | III | IV | V | ||
| Cohort size per quintile | 200000 | 200000 | 200000 | 200000 | 200000 | |
| Current coverage with social insurance | .16 | .344 | .636 | .716 | .492 | 17 |
| Target coverage | .8 | .8 | .8 | .8 | .8 | |
| Prevalence rate per quintile | .22 | .23 | .25 | .26 | .27 | 12 |
| Overall probability of seeking care | .0352 | .07912 | .159 | 0.18616 | 0.13284 | Prevalence * Current coverage with social insurance |
| Income inputs | $851.66 | 17 | ||||
| % of participation of income per quintile | 5.4 | 9.4 | 13.4 | 19.6 | 52.2 | 17 |
| Average monthly GDP per capita (US $ at 2014) | 398.9 | 694.93 | 990.64 | 1449 | 3859.08 | 17 |
| Average out-pocket expenditures. | 66% | 19 | ||||
Source: Authors.
Note: Project: Cabello-Rangel H, Diaz-Castro L, Pineda-Antúnez C. Extended cost-effective interventions for schizophrenia to achieve universal health coverage in Mexico.
We consider that the population with Social Security has access to medicines and psychosocial care in the first and second level of medical care, which is concordant with the prevalence of coverage for low incidence mental disorders (Whiteford et al., 2013). For the present study, it is considered that in the highest income quintiles the prevalence is higher, given that they have better access and use of health care services, so that the probability of seeking care results from the product of the prevalence and the percentage of coverage in each quintile. The out-of-pocket expenditure for care medical is 66% of the monthly income (Wirtz, Santa-Ana-Tellez, Servan-Mori, & Avila-Burgos, 2012).
Treatment costs
It includes variable and fixed costs; the variable costs (food, laundry, laboratory, water, electric power, municipal waste, cleaning, private security) derived from the current expenses incurred for the operation of the service were determined by the Primary Cost system. The fixed costs derived from human resources (medical, nursing, social work, psychology, and intendancy) were obtained from the coefficient of the annual gross salary between the annual workday in minutes for the time allocated to the care of each patient, both cost were published in a previous study (Cabello-Rangel et al., 2011).
The present value of these costs was calculated with compound interest:
Where:
VF: Future value
VP: Present value
i = Interes rate, (the rate that approximates the time preference of people, commonly used as 3% or 5%)
n = Number of periods between present value and future value (Brigham & Houston, 2005).
The cost of medications was based on current prices according to the purchase price of the IMSS International Public Bid for 2017 in Mexico (Instituto Mexicano del Seguro Social, 2017) (Table 2).
Table 2 Cost of interventions to treatment schizophrenia
| Percent of cases | Average annual of out care consultations | Unitary Cost US $ (June 2018) | Cost per case US $ (June 2018) | |
|---|---|---|---|---|
| T1 = Psychosocial treatment + typic or atypical antipsychotic (Haloperidol/risperidone) | 100% | 4 | $1.78 | $7.12 |
| T2 = Psychosocial treatment + atypical antipsychotic (Olanzapine) | 100% | 4 | $1.78 | $7.12 |
| T3 = Early Intervention in Psychosis + atypical antipsychotic (Olanzapine) | 80% | 15 | $35.70 | $535.48 |
| Antipsychotics | ||||
| Haloperidol 5mg (1) | 40% | 1095 | $0.07 | $29.88 |
| Risperidone 2mg (2) | 30% | 2190 | $0.02 | $13.80 |
| Olanzapine 10mg (3) | 20% | 730 | $1.75 | $60.35 |
| Biperiden 2mg (T1) | 40% | 365 | $0.04 | $13.09 |
| Laboratory test | 100% | 1 | $14.04 | |
| Total, T1 | $77.93 | |||
| Total, T2 | $81.51 | |||
| Total, T3 | $606.29 |
Source: Authors.
Note: Project: Cabello-Rangel H, Diaz-Castro L, Pineda-Antúnez C. Extended cost-effective interventions for schizophrenia to achieve universal health coverage in Mexico.
Disability Adjusted Life Years (DALYs) were used as the measure of effectiveness of the interventions, the DALYs were calculated with the method to determine the prevalence Years Lost by Disability, that is: YLD = prevalent cases * (size of the effect * adherence) * weight of disability * average duration of illness * target coverage (Raykar, Nigam, & Chisholm, 2015).
Considering a population of one million people, a prevalence of 2 200 cases of schizophrenia is estimated. It is assumed that 80% of the population would be covered with UPF, that is, 1 760 cases.
Finally, the insurance value was calculated, which is the amount that an individual is willing to pay to receive health protection. For this, we estimated the expected value of the cost of treating schizophrenia without UPF at an individual level, using the following equation:
Where:
p = probability of receiving attention for Schizophrenia.
c = cost of treatment.
y = income.
Following the estimation of the insurance value of Verguet et al. (2015), the following equation of certainty is considered:
Where r is the coefficient of risk aversion (value 3%).
At the individual level, the delta in the monetary value is:
The insurance value at the population level by income quintile is:
Results
Ensuring a coverage of 80% of the population has an impact of 98 and 106 DALYs are avoided in the poorest quintile for T1 and T2, respectively, and even in the richest quintiles it has a positive effect (Table 3).
Table 3 DALYs evicted with interventions to treatment schizophrenia
| Income quintile | ||||||
|---|---|---|---|---|---|---|
| I | II | III | IV | V | Total | |
| DALY current burden | 465 | 515 | 611 | 1790 | 1153 | 4534 |
| T1 DALY evicted | 98 | 73 | 28 | 42 | 106 | 347 |
| T2 DALY evicted | 106 | 81 | 38 | 68 | 124 | 417 |
| T3 DALY evicted | 67 | 40 | 7 | 60 | 35 | 209 |
Source: Authors.
Note: Project: Cabello-Rangel H, Diaz-Castro L, Pineda-Antúnez C. Extended cost-effective interventions for schizophrenia to achieve universal health coverage in Mexico.
In the current situation, the cost of intervention financed by the government to the population with social security is up to 80% higher for the quintiles with higher income compared to the poorest quintile. In the present analysis, the out-of-pocket expense for the cost of intervention and the prevalence of the disease by income quintile ranged from US $ 60,930.00 to US $ 474,035.43 (Table 4).
Table 4 Cost of intervention to treatment schizophrenia with current coverage
| I | II | III | IV | V | Total | |||
|---|---|---|---|---|---|---|---|---|
| Intervention | T1 | Total cost of intervention | $5,486.27 | $12,331.64 | $24,781.74 | $29,014.90 | $20,704.44 | $92,319.00 |
| Private expenditure | $3,620.94 | $8,138.88 | $16,355.95 | $19,149.83 | $13,664.93 | $60,930.54 | ||
| Cost financial by government | $1,865.33 | $4,192.76 | $8,425.79 | $9,865.07 | $7,039.51 | $31,388.46 | ||
| T2 | Total cost of intervention | $5,738.21 | $12,897.92 | $25,919.74 | $30,347.28 | $21,655.21 | $96,558.35 | |
| Private expenditure | $3,787.22 | $8,512.63 | $17,107.03 | $20,029.21 | $14,292.44 | $63,728.51 | ||
| Cost financial by government | $1,950.99 | $4,385.29 | $8,812.71 | $10,318.08 | $7,362.77 | $32,829.84 | ||
| T3 | Total cost of intervention | $42,682.86 | $95,939.42 | $192,800.40 | $225,734.11 | $161,079.28 | $718,236.07 | |
| Private expenditure | $28,170.69 | $63,320.02 | $127,248.27 | $148,984.51 | $106,312.33 | $474,035.81 | ||
| Cost financial by government | $14,512.17 | $32,619.40 | $65,552.14 | $76,749.60 | $54,766.96 | $244,200.26 | ||
Source: Authors.
Note: Project: Cabello-Rangel H, Diaz-Castro L, Pineda-Antúnez C. Extended cost-effective interventions for schizophrenia to achieve universal health coverage in Mexico.
The effect of ensuring coverage for 80% of the population through UPF avoids out-of-pocket expenses in direct proportion to the percentage of increase in coverage capacity, ensuring medication, and psychosocial treatment for patients with schizophrenia. It has a positive effect in the avoided pocket expense from US $ 101,221 to US $ 787,498 according to the type of intervention.
Increasing coverage generates an additional cost for the government that is not directly related to the reduction of DALYs by quintile, that is, increasing government spending has a greater impact on the poorest quintile since the cost-effectiveness ratio is higher in this one quintile given that the DALYS avoided are greater with very little difference compared to the quintiles of higher income, that is, a distributive effect of the budget is generated (Table 5).
Table 5 Cost of intervention to treatment schizophrenia with coverage 80%
| I | II | III | IV | V | Total | |||
|---|---|---|---|---|---|---|---|---|
| Intervention | T1 | Total de cost of intervention | $27,431.36 | $28,678.24 | $31,172.00 | $32,418.88 | $33,665.76 | $153,366.24 |
| Additional cost for the government | $21,945.09 | $16,346.60 | $6,390.26 | $3,403.98 | $12,961.32 | $61,047.24 | ||
| Out-of-pocket averted | $18,104.70 | $18,927.64 | $20,573.52 | $21,396.46 | $22,219.40 | $101,221.72 | ||
| Ratio cost-effectiveness (Cost/DALY averted) | $223.93 | $223.93 | $228.22 | $81.05 | $122.28 | |||
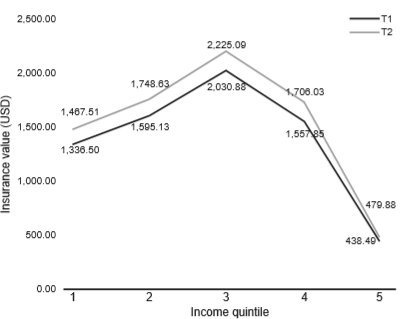
| Value insurance | $1,336.50 | $1,595.13 | $2,030.88 | $1,557.85 | $438.49 | $6,958.86 | ||
| T2 | Total de cost of intervention | $28,691.03 | $29,995.17 | $32,603.44 | $33,907.58 | $35,211.72 | $160,408.94 | |
| Additional cost for the government | $22,952.82 | $17,097.25 | $6,683.71 | $3,560.30 | $13,556.51 | $63,850.58 | ||
| Out-of-pocket averted | $18,936.08 | $19,796.81 | $21,518.27 | $22,379.00 | $23,239.73 | $105,869.90 | ||
| Ratio cost-effectiveness (Cost/DALY averted) | $216.54 | $211.08 | $175.89 | $52.36 | $109.33 | |||
| Value insurance | $1,467.51 | $1,748.63 | $2,225.09 | $1,706.03 | $479.88 | $7,627.14 | ||
| T3 | Total de cost of intervention | $213,414.28 | $223,114.93 | $242,516.23 | $252,216.88 | $261,917.53 | $1,193,179.86 | |
| Additional cost for the government | $170,731.43 | $127,175.51 | $49,715.83 | $26,482.77 | $100,838.25 | $474,943.79 | ||
| Out-of-pocket averted | $140,853.43 | $147,255.86 | $160,060.71 | $166,463.14 | $172,865.57 | $787,498.71 | ||
| Ratio cost-effectiveness (Cost/DALY averted) | $2,548.23 | $3,179.39 | $7,102.26 | $441.38 | $2,881.09 | |||
| Value insurance | NA | $155,178.57 | $162,797.95 | $112,351.84 | $28,069.55 | $458,397.91 | ||
Source: Authors.
Notes: NA: This value was not estimated since the treatment cost was higher than income therefore the negative difference could not be used in the Value Insurance equation. Project: Cabello-Rangel H, Diaz-Castro L, Pineda-Antúnez C. Extended cost-effective interventions for schizophrenia to achieve universal health coverage in Mexico.
The cost per capita of implementing each intervention, as the quantity of the total cost and the hypothetical population, is US $ 0.15, US $ 0.16 and US $ 1.19 for T1, T2 and T3 respectively. This means that T1 and T2 are highly affordable and low cost, while option T3 is possibly affordable, according to the criteria to identify investment priorities in mental health (World Health Organization, 2013).
The value of the annual assurance at the population level is US $ 7,627.14 for T2 and US $ 6,958.86 for T1. This valuation is not homogeneous among the quintiles, since quintile III is the one which is most willing to pay for insurance with respect to the other quintiles. On the other hand, in the highest income quintile, the minimum assurance valuation was observed. In the case of T3, it was found that this option is highly expensive, with a monthly treatment cost seven times higher than the other two options (Table 2). In turn, T3 is not available for all the quintiles because the insurance cost exceeds the income. In fact, for quintile I the treatment cost is 50% higher than the income and for this reason, it was not possible to estimate the insurance value, since the term (y-c) must be positive. Figure 1 shows the insurance value for the five quintiles of the two most cost-effective treatments.
Discussion and conclusion
In terms of the global burden of the disease, in 2016 in Mexico mental disorders were the fourth cause within the category of disability-adjusted life years (DALYs). However, the organized social response has been inadequate. Most people suffering from mental disorders, such as schizophrenia, do not seek or receive care due to lack of services and/or stigma, reflecting the huge attention gaps observed: around 69% for people with severe mental disorders (such as schizophrenia) in low-middle income countries do not receive treatment (Lora et al., 2012).
In the specific case of universal health coverage for schizophrenia, it was necessary to know the prevalence and cost of care to plan health care service, prioritize available resources, and establish the cost-effectiveness of current and future interventions.
In Mexico, under current conditions, the distribution of the budget for the care of patients with schizophrenia is inequitable. It is up to five times higher in the richest quintile than in the poorest one. The research carried out shows the approach to reduce the existing inequity in the population suffering from schizophrenia, given the current modalities of care in the country.
Under the premise of establishing a UPF to ensure that the population with schizophrenia receives available and affordable treatment, our research showed that two basic interventions such as typical or atypical antipsychotic treatment with same effectiveness + psychosocial treatment (T1) or atypical antipsychotic treatment + psychosocial treatment (T2), have a positive effect on the distribution of health spending, as evidenced by the extended cost-effectiveness analysis in the DALYs avoided. This interventions would create a more equitable health system, by systematically incorporating the health care required and accessible to this population, which would impact on patient, family, and social costs. In our opinion, the results serve as a substrate for the planning of mental health services with an effect of distributive justice of wealth.
If it is analyzed from the point of view of the value of the assurance, that is, of the user’s willingness to pay for interventions for T1 and T2, it is very similar, and is below the average level of income for each quintile, so they are very affordable.
Other currently available interventions, which require a higher degree of specialization and human resources per case, are not viable in middle-income countries such as Mexico. For instance, the EIP is not viable at population level, and the cost of treatment and willingness to pay is only feasible for the richest quintiles.
The extended cost-effectiveness analysis is essential before funding a health intervention to avoid incurring in the error of allocating budget to non-cost-effective interventions for the system. In the specific case of Mexico, it is necessary to reevaluate health interventions, particularly medicines. This in the understanding that the highest out-of-pocket expenses incurred by users of services, and the one that generate catastrophic health expenditure, is in the purchase of medicines. In this sense, T2 proves to be a viable option to expand treatment coverage in schizophrenia, because it is a highly cost-effective strategy and the most efficient of the three treatments analyzed in the present work, in addition to showing a greater value of population insurance.
Finally, the ECEA is an accessible method to generate information that allows decision makers to incorporate or exclude therapeutic interventions to achieve universal health coverage, as demonstrated in the present investigation.











 nueva página del texto (beta)
nueva página del texto (beta)