Introduction
Population aging is associated with an increase in cognitive impairment cases. In Latin America, a prevalence of 11% is estimated in adults aged 60 and over (Consejo Nacional de Población, 2013; Organización Panamericana de la Salud, 2001) compared with 8% in Mexico (Mejía-Arango, Miguel-Jaimes, Villa, Ruiz-Arregui, & Gutiérrez-Robledo, 2007; Wong, Espinoza, & Palloni, 2007). The Dementia Research Group 10/66 multicentric, population-based studies on adults aged 65 and over found an 8.6% prevalence of dementia for Mexico in urban areas and an 8.5% prevalence in rural areas, both adjusted for sex, age, and educational attainment (Rodriguez et al., 2008). Studies with data on dementia incidence in Mexico include the ENASEM (Encuesta Nacional de Salud y Envejecimiento en México) which, after a two-year follow-up (2001-2003), estimated an overall incidence rate of 27.3 cases per 1 000 person-years (Mejía-Arango & Gutierrez-Robledo, 2011). The 10/66 GID study also has estimates of dementia incidence in Mexican population based on an initial three-year follow-up. It reports an overall incidence of 30.4 cases per 1 000 person-years (Prince et al., 2012). Despite its higher incidence, however, less than half of the cases are diagnosed (particularly Alzheimer’s disease) (Wong, Michaels-Obregon, & Palloni, 2015). Among other factors, underestimation of cognitive impairment or dementia cases is due to the lack of systematic screening owing to limited consultation lengths (Navarrete & Rodríguez-Leyva, 2003), the absence of validated, easily-applied tools for timely detection and the minimization of the importance of cognitive and functional changes that occur in older adults (Bush, Kozak, & Elmslie, 1997; Doraiswamy, Steffens, Pitchumoni, & Tabrizi, 1998; Grober, Buschke, Crystal, Bang, & Dresner, 1998). However, early diagnosis of these diseases continues to be very important since it enables measures to be implemented to maintain patient safety and support and to educate caregivers, plan for the future and initiate appropriate pharmacological and non-pharmacological treatment.
“Episodic” memory problems are common in people with cognitive impairment due to Alzheimer’s disease and tend to appear early. Moreover, their effect on memory-which translates hippocampal damage-is key to establishing an early diagnosis of Alzheimer’s disease (AD), the most frequent form of major neurocognitive disorder (ND) in Mexico and the world (American Psychiatric Association, 2014; Dubois et al., 2010; Grober et al., 2016). A simple test evaluating episodic memory could therefore be useful in clinical practice. So, Dubois et al. (2002) developed the Five-Word Test (5WT) to assess verbal episodic memory to obtain a cortical neuroanatomical profile. This tool has proven to be simple and valid for the identification of cognitive disorders such as Alzheimer’s disease. However, its application outside its country of origin is limited. Accordingly, the main objective of the present study was to determine the concurrent validity of the 5WT for screening minor and major ND and culturally adapt it for Mexican older adults.
Material and methods
Study design
Validation and cultural adaptation study conducted between March 2017 and March 2018 at the Memory Clinic of a tertiary-level university hospital in Mexico City.
Participants
The study included men and women aged 60 and older, who lived in community and agreed to participate after signing an informed consent form. The sample size was calculated from the nomogram proposed by Carley, Dosman, Jones, and Harrison (2005), where a prevalence of ND of over 8%, confidence intervals (CI) of 95% and a test specificity of 90% were considered. Accordingly, at least 70 participants were required for each group with a 5% alpha and 80% power. Participants completed a standardized clinical and neuropsychological interview for age, sex, and educational attainment conducted by a specialist in geriatrics and/or neurology. The Mini-Mental State Examination (MMSE) (Folstein, Folstein, & McHugh, 1975) with a score of 0-30, where a higher score indicates better cognitive functioning and the clock face drawing test with a score of 0-14, where a lower score indicates better cognitive functioning (Aguilar-Navarro et al., 2018; Eknoyan, Hurley, & Taber, 2012) were applied.
Clinical diagnosis: Minor, major ND, and cognitively Healthy group
A diagnosis of Alzheimer’s disease or ND was established on the basis of the criteria of the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association NINCDS/ADRDA (McKhann et al., 1984), and the Clinical Dementia Rating Scale (CDR; Morris, 1993). The criteria established in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5, American Psychiatric Association (2014) were also used to establish a diagnosis of minor ND. The comparison or cognitively healthy group, comprising those with cognitively normal performance, who had no subjective memory complaints, scored over 26 in the MMSE and obtained a CDR = 0.
Functional status was assessed using the Katz Index with a score of 0-6, where a higher score indicated greater independence for basic activities of daily living (BADLs; Katz & Akpom, 1976) and the Lawton & Brody Index with a score of 0-8, where a higher score indicated greater independence in instrumental activities of daily living (IADLs; Lawton & Brody, 1969).
Exclusion criteria were: fewer than or equal to two years of schooling, presenting heart, liver, or kidney disease, cancer or another uncontrolled systemic disease, or a severe visual or auditory deficit in the clinical evaluation, which would make it impossible to apply the tests, presence of serious neurological diseases (toxic, metabolic, infectious), significant depressive symptomatology with a score of > 5/15 on the Geriatric Depression Scale (Sheikh & Yesavage, 1986), vascular and/or mixed dementia, and severe major ND according to the Clinical Dementia Rating Scale (CDR; Morris, 1993).
Five-word test (5WT)
Cultural adaptation of the 5WT
The cultural adaptation of this test was undertaken by linguistic experts from El Colegio de México. Five nouns from the Spanish language (Mexico) were selected, with a similar meaning in different regions of the country, with a length of two to three syllables and beginning with different letters of the alphabet. The five words belong to different semantic categories (Bus - transport, Glove - clothing, Pigeon - animal, Tooth - body part, Market - place). Understanding of the chosen words was tested in small groups of older adult volunteers who attended the memory clinic of the study site.
The 5WT involves two general stages: immediate recall and deferred recall. The first stage includes a Registration Phase, in which words printed on a sheet are presented (written in capital letters, with a 36-point font size): “Read this list of five words aloud and try to learn them because I will ask you for them later.” After the list had been read and with the list still in front of the patients, they are asked to point to and name each of the words, indicating the semantic category to which they belong. For example, “Could you point to and say which of these words is an animal?” and so on with each of them in the following order: animal, place, means of transport, body part, and clothing (in order to create a semantic association between the word and the category to which they belonged). This is followed by an Immediate Recall Phase in which, once the list has been removed, participants are asked to say the words they have just read in the order they remember them. The number of correctly remembered words constitutes the Immediate Free Recall score (IFR). Afterwards, if a word is not remembered, the examiner provides the semantic category to facilitate recall. The number of words recalled by using the semantic category constitutes the Immediate Recall with Clue (IRC) score. If the person fails to remember a particular word even with the semantic clue, its learning must be reinforced by showing him/her the list again and pointing to each unlearned word, naming both the semantic category to which they belonged and the word itself, for example, “The animal’s name is a dove.” The list is removed again, and the participant is asked about the word using its semantic clue to ensure its coding, for example, “What was the name of the animal?” This step can be repeated up to three times if necessary. Words learned in this way are not included in the score for this phase.
Before moving on to the second stage of the 5WT, a nonverbal cognitive task (such as the clock face drawing test) is performed, which acts as interference for three to five minutes. Participants subsequently proceed to the second stage.
During this stage, participants are asked to recall the five words on the list. The number of correctly remembered words constitutes the Deferred Free Recall (DFR) score. For each word not spontaneously recalled, participants are prompted with its semantic clue. The number of words recalled using the semantic category constitutes the Deferred Recall with Clue (DRC) score. This marks the end of the test.
Three scores can be estimated from the 5WT: a Free Recall Score (FRS) by adding the IFR + DFR, a Total Recall Score (TRS) from the sum of IFR + IRC + DFR + DRC (both scores with a range of 0 to 10), and a Weighted Total Score (WTS) calculated by using the following formula: [(IFR x 2) + IRC] + [(DFR x 2) + DRC] (range 0 to 20) (Croisile, Astier, & Beaumont, 2007). The estimated average time of application of the 5WT is five minutes.
Statistical analysis
A descriptive analysis of the sample was performed, registering frequencies, percentages, means, and standard deviations (SD) according to the type of variable. For the comparative analysis of the categorical variables, the Chi2 test and the Kruskal-Wallis test were used for continuous variables. The concurrent validity was established by comparing the 5WT with the MMSE and the clock face drawing test and the Spearman correlation coefficient estimate (rs).
Multinomial logistic regression models were constructed to determine the discriminative capacity of the 5WT of the three groups included, considering the effect of participants’ age, sex, and educational attainment. To establish the accuracy of the 5WT for the diagnosis of minor and major ND, the area under the curve was estimated, as well as its sensitivity and specificity. A p value of less than .05 was considered statistically significant. The analyses were performed using SPSS Statistics 20.0 (SPSS Inc., Chicago, Illinois). The protocol was approved by the ethics committee of the institution.
Results
Of the 215 participants included, 70 were classified as cognitively healthy (CH), 73 with minor ND and 72 with major ND. The average age was 78.9 years (SD = 7.8), 59% were women and average educational attainment was 9.9 years (SD = 5.2). Although participants with minor ND were older than the other two groups, there was no statistically significant difference with respect to sex or educational attainment. As expected, participants with minor and major ND performed worse on all cognitive tests compared with the CH group (both p ≤ .001). The sociodemographic data and cognitive performance of the participants are shown in Table 1.
Table 1 Comparative analysis between the three cognitive groups by sociodemographic and health variables
| CH | Minor ND | Major ND | ||
|---|---|---|---|---|
| n = 70 | n = 73 | n = 72 | p | |
| Age in years, average (SD) | 75.1 (6.9)a | 82.3 (7.7)b | 79.2 (7.2)c | ≤ .001 a,b,c |
| Female gender (%) | 65.7 | 53.42 | 58.3 | .324 |
| Schooling in years, average (SD) | 10.1 (5.1) | 10.6 (5.6) | 8.9 (4.8) | .118 |
| GDS, mean (SD) | 2.6 (2.7) | 2.93 (2.0) | 3.1 (1.6) | .318 |
| MMSE, mean (SD) | 27.7 (1.8)a | 26.1 (3.1)b | 20.7 (3.9)c | ≤ .001 |
| Clock face test, mean (SD) | 1.0 (1.7) to | 2.2 (1.98)b | 4.2 (3.5)c | ≤ .001 |
| Five-word test | ||||
| Free recall score, mean (range) | 8.8 (7-10)a | 6.9 (4-9)b | 4.1 (2-6)c | ≤ .001 |
| Total recall score, mean (range) | 9.7 (9-10)a | 8.8 (7-10)b | 6.5 (4-9)c | ≤ .001 |
| Weighted total score, mean (range) | 18.6 (16-20)a | 15.7 (12-19)b | 10.7 (6-15)c | ≤ .001 |
Notes: CH:Cognitively health, ND:Neurocognitive Disorder, GDS:Geriatric Depression Scale, MMSE:Mini-Mental State Examination.
Data are presented as means, ranges and standard deviations.
The analysis shows the differences between groups using the ANOVA, post-hoc DSM test.
a p ≤ .001 between control and minor ND;
b p ≤ .001 between control and major ND;
c p ≤ .001 between minor and major ND.
A moderate positive correlation was observed between the 5WT score and the MMSE (rs = .58; p < .001) and a low negative correlation between the 5WT and the clock face drawing test (rs = -.37; p < .001).
The multinomial logistic regression showed that the various 5WT scores (FRS, TRS and WTS) discriminated between the different groups (p < .001) even after considering the effect of age, sex, and educational attainment.
Finally, the area under the curve for the FRS, TRS, and WTS was estimated. This was .97 (95% CI [.94, .99]) for the WTS with a cut-off point of ≤ 16, 89% sensitivity and 98% specificity for the diagnosis of major ND (Figure 1).
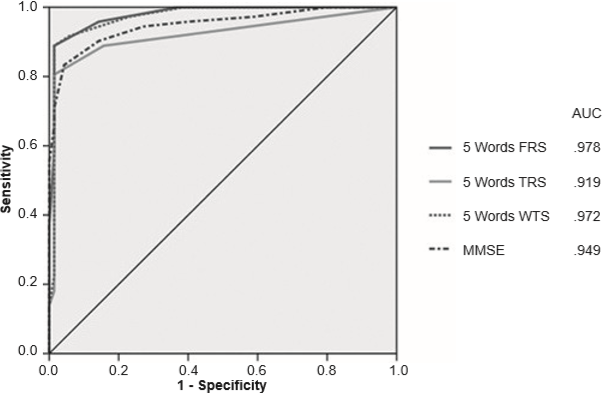
Figure 1 The area under the curve of the Mini-Mental State Examination (MMSE) and the free recall score (FRS), the total recall score (TRS), and the weighted total score (WTC) of the Five-Word Test for the diagnosis of major ND compared to cognitively healthy participants. AUC indicates the area under the curve.
Conversely, for the diagnosis of minor ND, the area under the WTS curve was smaller, .77 (95% CI [.70, .85]) with a cut-off point of ≤ 18, 66% sensitivity and 77% specificity (Figure 2).

Figure 2 The area under the curve of the Mini-Mental State Examination (MMSE) and the free recall score (FRS), the total recall score (TRS), and the weighted total score (WTC) of the Five-Word Test for the diagnosis of minor ND compared to cognitively healthy participants. AUC indicates the area under the curve.
Finally, Table 2 shows and highlights the sensitivity and specificity for the detection of major ND and minor ND with the optimal cut-off values of FRS, TRS, and WTS.
Table 2 Optimum cut-off points, sensitivity and specificity of 5WT
| CH vs Major ND | CH vs Minor ND | ||||||
|---|---|---|---|---|---|---|---|
| Cut-off point | Sensitivity | Specificity | Cut-off point | Sensitivity | Specificity | ||
| FRS | ≤ 7 | 88.9% | 98.6% | ≤ 6 | 74.0% | 62.9% | |
| TRS | ≤ 9 | 80.6% | 98.6% | ≤10 | 56.2% | 84.3% | |
| WTS | ≤ 16 | 88.9% | 98.6% | ≤18 | 64.4% | 77.1% | |
Notes: CH:Cognitively healthy, ND:Neurocognitive disorder, FRS:Free recall score, TRS:Total recall score, WTS:Weighted total score.
Discussion and conclusion
The present study shows that the 5WT can be culturally adapted to a different environment from the one in which it was developed and without losing its psychometric qualities for screening neurocognitive disorders in older adults. The results show that the 5WT is useful for discriminating between people with and without cognitive impairment.
In the case of major ND (dementia), the areas under the curve estimated by the different components of the 5WT are larger than those of the MMSE, which is a common global screening instrument, while its sensitivity and specificity are similar to those of previous studies (Croisile et al., 2007; Mormont, Jamart, & Robaye, 2012). These areas are not statistically different from each other, however, suggesting that the 5WT alone is no more useful for screening for major ND than the MMSE. Nevertheless, using the 5WT (with a cut-off point of ≤ 16; 89% sensitivity and 98% specificity) together with the MMSE (with a cut-off point of ≤ 24; 83% sensitivity, and 96% specificity) could be a strategy for increasing the diagnostic accuracy of major ND with neurodegenerative etiology (Alzheimer’s disease) because the nature of the 5WT allows an analysis of the amnesic mechanisms that are only superficially explored by the MMSE.
On the other hand, as in the study by Rozzini et al. (2017), the 5WT proved to be useful for identifying subjects with minor ND or mild cognitive impairment (MCI), albeit with lower sensitivity and specificity and area under the curve, which was .77 (95% CI [.70, .85]) with a cut-off point of ≤ 18, 66% sensitivity and 77% specificity, which can be attributed to the subtlety and heterogeneity of the cognitive alterations present in subjects with MCI. Accordingly, the use of such a screening tool could be insufficient for identifying minor ND due to the false positives it contains. However, when attempts have been made to analyze the various types of MCI (for example, single domain versus multiple domains; Bolívar & Saladie, 2016), it has proved to discriminate between them.
Thus, the 5WT is a test that is valid for assessing verbal episodic memory, which is the specific element of amnesic cognitive impairment and is usually an initial clinical finding of the most frequent form of major degenerative ND (Alzheimer’s disease). Consequently, poor performance in the 5WT would translate the functional disconnection of the hippocampus from neocortical regions (American Psychiatric Association, 2014; Dubois et al., 2010).
The 5WT appears to be a useful instrument for both clinical practice and research since, in addition to obtaining a score that makes it possible to discriminate different states of a patient’s cognitive function, it also offers complementary qualitative elements (such as type of errors and dissociation between the performance of the various memory mechanisms), which could be used for subjective analysis and contribute to accuracy when establishing a clinical diagnosis. Although the educational attainment of the participants in this study was lower than that of the original French study (Dubois et al., 2002), the 5WT maintains its discriminative qualities.
However, this study has some limitations. Participants were recruited at a memory clinic of a single tertiary level health center, and those with a degenerative cognitive profile were selected, which excludes all the vascular or mixed forms of cognitive impairment also common in Mexico, suggesting a potential selection bias. Consequently, its results should be interpreted with caution when it is used as a screening tool in the general population. In addition, the inter- or intra-rater reliability of the 5WT was not evaluated in this study, which would have been desirable.
Despite its limitations, the present study offers the first Spanish validation and cultural adaptation of the 5WT, which will encourage its widespread use and therefore a better understanding of its qualities for screening for cognitive problems in older adults.











 nova página do texto(beta)
nova página do texto(beta)


