Introduction
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder that is highly prevalent in children and adolescents. The difficulties in the regulation of attention, hyperactivity, and impulsivity that characterize the disorder affect different areas of the development of children and adolescents who suffer from it, specially in learning and relationships with peers and family members ( Barkley, 2006 ). ADHD is one of the main causes of consultation in child mental health. Chilean children and adolescents diagnosed with ADHD have high rates of use of services (50.9%), compared to those with other disruptive disorders (27.6%) and non-disruptive disorders (36.8%) ( de la Barra, Vicente, Saldivia, & Melipillan, 2013 ).
Follow-up studies of children diagnosed with ADHD, compared with control groups, show that they have a higher-grade retention rate, participation on special educational needs programs, school suspensions, school expulsion, and lower academic performance. Fewer children with ADHD are able to enter university, and a lower percentage of them, graduate compared with the control group. Adults with ADHD suffer higher rates of job layoffs, change jobs more frequently, and have lower scores on performance evaluations. Certain activities of daily life, such as driving, are also affected, resulting in higher incidence of traffic fines, unsafe driving habits, and increased incidence of motor vehicle accidents ( Barkley, 2002 ).
In relation to the association of ADHD with personality disorders (PDs), the life impact of ADHD was studied in a representative community sample of 34 653 adults of the U.S. population. The prevalence of ADHD was 2.51% (n = 807). They had a higher risk of presenting a diagnosis of any psychiatric disorder throughout their lives (94.98%) than the general population (64.54%), which included bipolar disorder (33.56% ADHD - 6.23% general population), generalized anxiety disorder (25.99% - 7.19%), post-traumatic stress disorder (21.99% - 6.02%), specific phobia (35.75% - 14.61%) and personality disorder (62.79% - 20.46%) (narcissistic [25.16% - 5.69%], histrionic [10.74% - 1.57%], limit [33.69% - 5.17%], antisocial [18.66% - 3.46%], and schizotypal [22.42% - 3.46%]). In addition, ADHD throughout life was associated with a series of behaviors that imply lack of planning and poor inhibitory control. A greater number of adverse events was observed, less health, social support and greater perceived stress. Less than half of the individuals with ADHD had previously consulted a specialist and only a quarter had received medication ( Bernardi et al., 2012 ).
A 10-year follow-up longitudinal study showed that ADHD onset during childhood poses risks to develop PDs later on in adulthood, such as borderline personality disorder, antisocial PD, avoidant PD and narcissistic PD ( Miller et al., 2008 ). Subjects with persistent ADHD had a greater risk of developing antisocial PD and paranoid PD ( Miller et al., 2008 ). Some authors propose that the presence of ADHD could determine certain profiles of PDs, for example, patients with borderline PD and ADHD would have a more impulsive profile, while patients with borderline PD who did not suffer from ADHD would have more mood and anxiety disorders ( Ferrer et al., 2010 ). Comorbid personality disorders may explain at least in part the psychosocial malfunction that some adults with ADHD have ( Jacob et al., 2014 ).
In Chile, research on personality profiles of adolescent ADHD population is very limited, similar to the state of art in the rest of the world. The objective of this study is to explore the personality profiles of Chilean adolescent patients diagnosed with ADHD and compare them with the baseline population for the patient and non-patient groups. The aim is to highlight the importance of considering various elements in the diagnosis of adolescents with ADHD in order to develop and implement interventions appropriate to the specific needs of each patient.
Method
Participants
A convenience sampling was conducted in two psychiatric outpatient clincs in the Metropolitan Region of Chile. One center is the outpatient psychiatric unit of a university hospital and the other one is a private outpatient center. Adolescents having ADHD as the main diagnosis were invited to participate and were evaluated through clinical interviews conducted by two experienced child and adolescent psychiatrists who used DSM-5 criteria for the diagnosis of ADHD and comorbidities. Adolescents diagnosed with autism spectrum disorders, psychosis, cognitive disability, and those who did not know how to read and write were excluded from the selection.
Instruments
MACI-A; Millon Adolescent Clinical Inventory
MACI is an inventory that measures personality profiles in adolescents between 13 and 19 years of age. It was created by Theodore Millon in 1993. It has been validated in diverse populations showing adequate indexes of validity and reliability ( Millon, 1987 ; 1993 ; Blumentritt & VanVoorhis, 2004 ; Pinto & Grillo, 2004 ; Aguirre, 2004 ). In Chile, this instrument was validated by Vinet (2006) and has been used in various studies in the country ( Vinet & Forns, 2005 ; Alarcón, Vinet, & Salvo, 2005 ; Vinet & Forns, 2006 ; Vinet & Alarcón, 2009a ; Vinet, Faúndez, & Larraguibel, 2009 ; Vinet, Alarcon, & Pérez-Luco, 2010 ). It is a self-administered written questionnaire, and its application takes approximately 30 minutes. It consists of 160 items of true/false style answers that evaluates 31 scales, which are classified into: 12 personality prototypes, eight expressed concerns, and seven clinical syndromes. Prototype personality scales measure psychological functioning styles that emerge through development and stabilize in adolescence ( Vinet, Barrera-Herrera, & Salinas-Oñate, 2014 ). The expressed scales concerns measure feelings and attitudes about specific issues that worry adolescents. The scales of clinical syndromes measure the predisposition to present probable mental disorders during adolescence ( Vinet et al., 2014 ). The present research considered the exploration of specific profiles that evaluate the psychological functioning of each adolescent and that include prototypes of personality, expressed concern, and clinical syndromes, in the same way that it has been used in other studies carried out in Chile ( Vinet & Forns, 2005 ; Alarcón, Vinet, & Salvo, 2005 ; Vinet & Forns, 2006 ; Vinet & Alarcón, 2009b ; Vinet et al., 2009 ; Vinet et al., 2010 ).
Determinants associated with mental health, comorbid disorders, and use of pharmacological treatment were recorded. This registration form was specially constructed for this research and includes the data of patient’s identification, type of school, grade retention, type of presentation of ADHD, comorbidities, adverse childhood experiences (ACEs), and use of psychotropic drugs. The determinants associated with mental health were obtained according to the international literature, among which are the early adverse experiences ( Felitti et al., 1998 ; Ramiro, Madrid, & Brown, 2010 ; Finkelhor, Shattuck, Turner, & Hamby, 2013 ; Pi, 2014 ), socioeconomic status (measured indirectly through the type of educational establishment), gender ( Costa, Terracciano, & McCrae, 2001 ; Klonsky, Jane, Turkheimer, & Oltmanns, 2002 ; Biederman, Faraone, Monuteaux, Bober, & Cadogen, 2004 ; Rucklidge, 2010 ; Weisberg, deYoung, & Hirsh, 2011 ; de Bolle et al., 2015 ), and grade retention ( Cohen, Crawford, Johnson, & Kasen, 2005 ; Kent et al., 2011 ).
Procedures
The research team agreed on the diagnostic criteria for ADHD and comorbid disorders according to DSM-5 and the criteria for ACEs. Child and adolescents psychiatry residents and adolescents from the Clínica Psiquiátrica Universitaria (CPU) were invited to participate in the recruitment of patients. Subsequently, patients from a private psychiatric center where a member of the research team works were included in order to increase the sample size. The patients participating in the study signed assent (consent in the case of adults) and their parents’ informed consent. The treating physicians applied the MACI questionnaire to adolescents who met the diagnostic criteria for the study and completed the registration form developed for this research. The later was carried out in conjunction with the principal investigator to verify that the criteria previously agreed upon were met.
Design
Empirical, non-experimental, quantitative, associative strategy research, using a cross-sectional comparative method and a design of natural groups according to the classification of Ato, López, and Benavente (2013) . We sought to explore the association between the variables studied, in which the object of the exploration is the comparison at a given time of the sample groups, with the groups of patient and non-patient population of previous studies ( Ato et al., 2013 ).
Analysis
To identify personality profiles of adolescents with ADHD, a sample T test was performed comparing the means obtained from our patients for each personality pattern to the means from each personality pattern from the reference parameters published in the Chilean validation study of standards for the MACI ( Vinet, Fort, & Santacana, 2008 ). Afterwards these profiles were compared to the patient and non-patient population referential data ( Vinet et al., 2008 ). To identify personality sub-profiles, hierarchical conglomerate analyses were used to determine the optimal number of clusters to be found. We then performed Mann-Whitney U test to compare the difference of distributions for ordinal variables and T test of two independent samples to compare the means of the two groups for quantitative variables. Finally, Biplot JH analysis was carried out, which allows the visual analysis of the matrix structure of the data, facilitating its interpretation ( Gabriel, 1971 ). To analyze if there were any differences in the cluster membership depending on the type of clinical presentation of ADHD, comorbidity, pharmacological treatment, and determinants associated with mental health (ACEs, type of school and grade retention), a chi square test was used. The variables grade retention, comorbid diagnosis, ACEs, and pharmacological treatment were considered as dichotomous variables (presence/absence). The SPSS 23 and STATA 12 programs were used to perform the analyses described. This study has the approval of the ethics committee of the Clinical Hospital of the University of Chile.
Results
Characterization of the sample
In total, 61 adolescents were surveyed (50.8% women), between 13 and 19 years of age (mean age 15.9 years, SD = 2.061). A total of 52% of the sample had a predominantly inattentive presentation of ADHD and 43% had a combined presentation (Table 1). When dividing the sample by gender, 58% of the female sample had a predominantly inattentive presentation of ADHD and 39% had a combined presentation. In the men sample, 46.6% had a predominantly inattentive presentation, 46.6% a combined presentation, and 6.6% a predominantly hyperactive/impulsive presentation. Most of adolescents did not present a history of grade retention (77%) ( Table 1 ).
Table 1. Frequency of variables of clinical presentation type of ADHD, grade retention, presence of comorbidity, presence of ACEs and use of medication for the total sample, women and men
| Total | Female | Male | ||||
|---|---|---|---|---|---|---|
| Variable | n | % | n | % | n | % |
| ADHD clinical presentation | ||||||
| Inatentive | 32 | 52% | 18 | 58% | 14 | 46.6% |
| Hyp/imp | 3 | 5% | 1 | 3% | 2 | 6.6% |
| Combined | 26 | 43% | 12 | 39% | 14 | 46.6% |
| Grade retention | ||||||
| No | 47 | 77% | 25 | 81% | 22 | 73% |
| Yes | 14 | 23% | 6 | 19% | 8 | 27% |
| Comorbidities | ||||||
| No | 26 | 43% | 9 | 29% | 17 | 57% |
| Yes | 35 | 57% | 22 | 71% | 13 | 43% |
| Presence of ACEs | ||||||
| No | 21 | 34% | 10 | 32% | 11 | 37% |
| Yes | 40 | 66% | 21 | 68% | 19 | 63% |
| Medication | ||||||
| No | 28 | 46% | 14 | 45% | 14 | 47% |
| Yes | 33 | 54% | 17 | 55% | 16 | 53% |
Regarding the presence of comorbidity, 35 adolescents (57%) had at least one comorbid diagnosis, the most frequent being the presence of one comorbidity. In women, the most frequent were anxiety disorder (29%), depressive disorder, and learning disorder (13%). In men, the most frequent comorbid disorder was anxiety disorder (13%).
Of the total sample and, disregarding gender 40 adolescents (66%) had a previous history of having suffered at least one ACE, being the most frequent to present only one of them. In the group of women, the ACEs included: living with a family member suffering from a mental disorder (39%), divorce or separation of the parents (32%), abandonment by the father (16%), intra-family violence (13%), and alcohol abuse by a relative (10%). In the group of men, living with a relative who suffers from mental disorder (20%), abandonment of the father (17%), divorce or separation from the parents (13%), intra-family violence, and physical abuse (10%). Of the total sample, 54% was under pharmacological treatment, and for both sexes the most frequently used drug was methylphenidate (76% and 75%, respectively).
Personality profiles of adolescents with ADHD
To explore the personality profiles of the adolescents with ADHD, the scores obtained from the sample were compared with those of the reference population. Because MACI standards for Chilean population are differentiated according to gender, the statistical analyses conducted in this study for groups of men and women were considered separately.
Females
The sub-sample of women with ADHD behaved similarly to the group of non-patient women when responding to the MACI questionnaire as shown in Table 2. When compared with the non-patient population from the Chilean parameters, only six (22%) of the 27 scales showed significant differences. The greatest differences were found in the scales 5 - egotistic - (t [30] = -4.02 p = < .05) and 7 - conforming - (t [30] = -3.00 p = < .05), where the studied group showed lower scores, and BB- substance abuse proneness - (t [30] = 2.27 p = < .05), where they showed higher scores. It should be noted that the egotistic and conforming scales are counter-theoretical scales used in the study of the validation of the instrument in the Chilean population, so that low scores on these scales are associated with mental health problems.
Table 2. Comparison of means of MACI’s personality patterns with patient and non-patient reference populations in the women’s sample
| Difference with | Difference with | ||||
|---|---|---|---|---|---|
| non-patient population | patient population | ||||
| Dif | t | Dif | t | ||
| Personality Pattern | |||||
| 1 | Introversive | 4.13 | 2.22* | -9.25 | -4.97*** |
| 2A | Inhibited | 3.52 | 1.78 | -9.75 | -4.93*** |
| 2B | Doleful | .39 | .24 | -15.78 | -9.74*** |
| 3 | Submissive | -1.65 | -1.19 | 1.27 | .92*** |
| 4 | Dramatizing | -3.37 | -2.05 | 5.56 | 3.38*** |
| 5 | Egotistic | -6.16 | -4.02*** | 1.63 | 1.06*** |
| 6A | Unruly | 2.58 | 1.95 | -6.37 | -4.81 |
| 6B | Forceful | 2.42 | 2.01 | -4.21 | -3.50 |
| 7 | Conforming | -4.66 | -3.00* | 7.12 | 4.58* |
| 8A | Oppositional | 2.85 | 1.95 | -12.68 | -8.66*** |
| 8B | Self-demeaning | 4.65 | 2.03 | -15.88 | -6.94*** |
| 9 | Borderline tendency | 2.63 | 2.15 | -9.02 | -7.37*** |
| Expressed Concerns | |||||
| A | Identity diffusion | 2.79 | 2.01 | -7.35 | -5.30*** |
| B | Self-devaluation | 4.61 | 1.86 | -15.40 | -6.20*** |
| C | Body disapproval | 3.12 | 1.76 | -3.67 | -2.07*** |
| D | Sexual discomfort | 1.14 | 1.24 | 4.23 | 4.57* |
| E | Peer insecurity | .78 | 0.70 | -4.77 | -4.33*** |
| F | Social insensitivity | -.22 | -.15 | -.19 | -.13*** |
| G | Family discord | 2.25 | 2.25* | -5.30 | -5.29* |
| H | Childhood abuse | .13 | .16 | -8.09 | -10.14*** |
| Clinical Syndromes | |||||
| AA | Eating dysfunctios | 4.42 | 2.23* | -4.67 | -2.36*** |
| BB | Substance abuse proneness | 2.46 | 2.27* | -7.50 | -6.90 |
| CC | Delinquent predisposition | .10 | .09 | .53 | .50*** |
| DD | Impulsive propensity | 1.41 | 1.38 | -4.01 | -3.91 |
| EE | Anxious feelings | .20 | .17 | .68 | .58*** |
| FF | Depressive affect | 2.90 | 1.63 | -11.53 | -6.47*** |
| GG | Suicidal tendency | 1.12 | .92 | -11.39 | -9.36*** |
Note: Dif = differences between the observed value and the reference value; t = t student’s statistics;
***p < .001,
**p < .01,
*p < .05.
When comparing the group of women diagnosed with ADHD with the reference group of the patient population from the Chilean parameters, differences appeared in 23 (85%) of the 27 scales. The greatest differences were found in scales 2b - doleful - (t [30] = -9.74 p = < .05), H - childhood abuse - (t [30] = -10.14 p = < .05) and GG - suicidal tendency - (t [30] = -9.36 p = <. 05), where lower scores are exhibited.
Males
The sample of male adolescents responding to the MACI questionnaire behaved similarly to the group of the patients, as shown in Table 3. When comparing male patients with ADHD with the reference non-patient population, they showed significant differences in 15 scales (56%). The greatest differences were found in the scales A – identity diffusion - (t [30] = 3.35 p = < .05), G - family discord - (t [30] = 3.69 p = < .05) and FF - depressive affect - (t [30] = 3.33 p = < .05), where men with ADHD had higher scores than non-patient men. When comparing male adolescents with ADHD with the patient population, they showed significant differences in eight scales (30%). The greatest differences were found in the scales 6A - unruly - (t [30] = -4.07 p = < .05), H- childhood abuse - (t [30] = -3.85 p = < .05), and CC –delinquent predisposition - (t [30] = -4.78 p = < .05), where they obtain significantly lower scores.
Table 3. Comparison of means of MACI’s personality patterns with patient and non-patient reference population in the men’s sample
| Difference with | Difference with | ||||
|---|---|---|---|---|---|
| non-patient population | patient population | ||||
| Dif | t | Dif | t | ||
| Personality Pattern | |||||
| 1 | Introversive | 4.47 | 2.23* | -2.42 | -1.21 |
| 2A | Inhibited | 3.47 | 1.75 | -3.87 | -1.98 |
| 2B | Doleful | 5.58 | 2.79* | -5.00 | -2.54* |
| 3 | Submissive | -1.49 | - .92 | 1.04 | .65 |
| 4 | Dramatizing | -2.19 | -1.24 | .74 | .43 |
| 5 | Egotistic | -4.23 | -2.71* | .50 | .33 |
| 6A | Unruly | 2.86 | 1.43 | -8.03 | -4.07*** |
| 6B | Forceful | 3.96 | 1.96 | -1.62 | -.82 |
| 7 | Conforming | -5.79 | -2.87* | 3.90 | 1.97 |
| 8A | Oppositional | 7.11 | 2.87* | -4.09 | -1.68 |
| 8B | Self-demeaning | 8.79 | 3.02* | -5.17 | -1.81 |
| 9 | Borderline tendency | 6.00 | 3.13*** | -2.14 | -1.14 |
| Expressed Concerns | |||||
| A | Identity diffusion | 5.32 | 3.35*** | -2.33 | -1.49 |
| B | Self-devaluation | 8.43 | 3.13*** | -5.20 | -1.96 |
| C | Body disapproval | 3.95 | 2.58* | .52 | .34 |
| D | Sexual discomfort | -.82 | -.69 | 2.85 | 2.43* |
| E | Peer insecurity | - .12 | - .11 | -1.91 | -1.84 |
| F | Social insensitivity | - .72 | - .42 | -2.94 | -1.74 |
| G | Family discord | 5.24 | 3.69*** | -.25 | -.18 |
| H | Childhood abuse | 1.51 | 1.63 | -3.52 | -3.85*** |
| Clinical Syndromes | |||||
| AA | Eating dysfunctios | 5.07 | 2.86* | .95 | .54 |
| BB | Substance abuse proneness | 5.76 | 2.52* | -6.02 | -2.68* |
| CC | Delinquent predisposition | - .47 | - .44 | -5.07 | -4.78*** |
| DD | Impulsive propensity | 3.20 | 1.81 | -2.39 | -1.38 |
| EE | Anxious feelings | .45 | .50 | 3.19 | 3.63*** |
| FF | Depressive affect | 6.18 | 3.33*** | -2.01 | -1.10 |
| GG | Suicidal tendency | 3.45 | 2.51* | -4.41 | -3.26*** |
Note: Dif = differences between the observed value and the reference value; t = t student’s statistics;
***p < .001,
**p < .01,
*p < .05.
Personality sub-profiles of adolescent consultants with ADHD
To describe personality sub-profiles within the group studied, the research team performed a hierarchical cluster analysis, which determined that the optimal number of clusters for the sample of adolescents with ADHD was two. A cluster of eight adolescents was configured for the female and male samples (cluster 1). The adolescents belonging to this cluster had higher scores on most of the MACI scales compared to cluster 2 subjects (23 women and 22 men) (Tables 4 and 5).
Table 4. Configuration of clusters for female subjects according to MACI’s Personality Patterns
| Cluster 1 (n = 8) | Cluster 2 (n = 23) | U Mann- | Asymptotic | ||||
|---|---|---|---|---|---|---|---|
| Media | DS | Media | DS | Whitney | Z | sig. (bilateral) | |
| Personality Pattern | |||||||
| PB1 Introversive | 33.38 | 10.914 | 20.78 | 8.107 | 29.5 | -2.825 | .005 |
| PB2A Inhibited | 37.88 | 7.453 | 18.26 | 6.614 | 5 | -3.933 | .000 |
| PB2B Doleful | 23.25 | 5.365 | 5.52 | 4.133 | 0 | -4.161 | .000 |
| PB3 Submissive | 55.00 | 8.848 | 52.74 | 7.43 | 77 | -.678 | .498 |
| PB4 Dramatizing | 25.88 | 7.68 | 40.13 | 6.384 | 16 | -3.439 | .001 |
| PB5 Egotistic | 19.75 | 7.146 | 31.48 | 6.781 | 22.5 | -3.142 | .002 |
| PB6A Unruly | 23.13 | 6.686 | 24.91 | 7.687 | 82.5 | -.43 | .667 |
| PB6B Forceful | 11.13 | 9.342 | 8.83 | 5.67 | 81 | -.498 | .619 |
| PB7 Conforming | 43.88 | 8.167 | 49.17 | 8.553 | 60.5 | -1.425 | .154 |
| PB8A Opositional | 25.38 | 8.262 | 15.13 | 6.363 | 28 | -2.896 | .004 |
| PB8B Self-demeaning | 35.75 | 9.677 | 15.13 | 8.756 | 11 | -3.66 | .000 |
| PB9 Borderline Tenden. | 19.38 | 5.423 | 10.35 | 5.662 | 21.5 | -3.2 | .001 |
| Expressed Concerns | |||||||
| PBA Identity diffusion | 21.63 | 6.391 | 12.17 | 6.651 | 28 | -2.895 | .004 |
| PBB Self-devaluation | 39.5 | 7.309 | 16.74 | 10.19 | 3 | -4.024 | .000 |
| PBC Body disapproval | 21.75 | 5.825 | 10.83 | 9.466 | 34 | -2.626 | .009 |
| PBD Sexual discomfort | 35.5 | 3.423 | 36.65 | 5.678 | 71.5 | -.931 | .352 |
| PBE Peer insecurity | 15.63 | 7.386 | 6.61 | 3.474 | 19.5 | -3.287 | .001 |
| PBF Social insensitivity | 16.5 | 8.229 | 23.22 | 7.045 | 40.5 | -2.337 | .019 |
| PBG Family discord | 17.25 | 6.042 | 15 | 5.427 | 73.5 | -.837 | .403 |
| PBH Childhood abuse | 10.88 | 3.482 | 3.83 | 3.114 | 12.5 | -3.613 | .000 |
| Clinical Syndromes | |||||||
| PBAA Eating dysfunct. | 25.75 | 5.497 | 14.74 | 11.096 | 45.5 | -2.102 | .036 |
| PBBB Substance abuse P. | 10.25 | 5.726 | 9.78 | 6.274 | 85.5 | -.295 | .768 |
| PBCC delinquent pred. | 13.13 | 5.463 | 20.39 | 4.822 | 30 | -2.807 | .005 |
| PBDD Impulsive prop. | 13.25 | 5.23 | 14.35 | 5.944 | 84.5 | -.34 | .733 |
| PBEE Anxious feelings | 37.63 | 6.823 | 35.61 | 6.5 | 76.5 | -.701 | .483 |
| PBFF Depressive affect | 31.5 | 5.372 | 13.52 | 6.141 | 5 | -3.93 | .000 |
| PBGG Suicidal tendency | 15.87 | 6.081 | 3.35 | 2.917 | 2.5 | -4.064 | .000 |
Table 5. Configuration of clusters for male subjects according to MACI’s Personality Patterns
| Cluster 1 (n = 8) | Cluster 2 (n = 22) | U de Mann- | Asymptotic | ||||
|---|---|---|---|---|---|---|---|
| Media | DS | Media | DS | Whitney | Z | sig. (bilateral) | |
| Personality Pattern | |||||||
| PB1 Introversive | 36.38 | 10.211 | 21.41 | 8.33 | 18.5 | -3.263 | .001 |
| PB2A Inhibited | 31.63 | 11.55 | 16.05 | 7.175 | 5 | -3.289 | .001 |
| PB2B Doleful | 26.63 | 10.155 | 8.95 | 6.608 | 0 | -3.458 | .001 |
| PB3 Submissive | 41.5 | 12.364 | 49.09 | 6.458 | 77 | -1.647 | .100 |
| PB4 Dramatizing | 34.25 | 13.885 | 41.55 | 7.062 | 16 | -1.456 | .145 |
| PB5 Egotistic | 30.75 | 12.859 | 36.05 | 6.153 | 22.5 | -.966 | .334 |
| PB6A Unruly | 41.63 | 12.637 | 25.5 | 6.375 | 82.5 | -2.934 | .003 |
| PB6B Forceful | 26.63 | 12.705 | 8.36 | 4.624 | 81 | -3.579 | .000 |
| PB7 Conforming | 31.75 | 8.812 | 50.14 | 6.923 | 60.5 | -3.873 | .000 |
| PB8A Opositional | 41.88 | 10.077 | 16.55 | 6.412 | 28 | -4.015 | .000 |
| PB8B Self-Demeaning | 39.5 | 12.604 | 14.18 | 10.852 | 11 | -3.474 | .001 |
| PB9 Borderline Tenden. | 27.13 | 11.606 | 10.45 | 5.422 | 21.5 | -3.859 | .000 |
| Expressed Concerns | |||||||
| PBA Identity Diffusion | 28 | 3.338 | 12.55 | 5.853 | 28 | -3.991 | .000 |
| PBB Self-Devaluation | 39.38 | 12.059 | 14.55 | 8.98 | 3 | -3.849 | .000 |
| PBC Body Disapproval | 17 | 6.845 | 5.73 | 6.798 | 34 | -3.174 | .002 |
| PBD Sexual Discomfort | 25 | 4.66 | 31.5 | 6.3 | 71.5 | -2.679 | .007 |
| PBE Peer Insecurity | 10.75 | 7.592 | 7.18 | 4.817 | 19.5 | -1.133 | .257 |
| PBF Social Insensitivity | 35.13 | 14.126 | 24.32 | 4.765 | 40.5 | -1.888 | .059 |
| PBG Family Discord | 26.5 | 7.54 | 15.09 | 5.309 | 73.5 | -3.432 | .001 |
| PBH Childhood Abuse | 11.25 | 5.701 | 3.14 | 2.55 | 12.5 | -3.638 | .000 |
| Clinical Syndromes | |||||||
| PBAA Eating Dysfunct. | 20.38 | 8.815 | 6.68 | 7.22 | 45.5 | -3.455 | .001 |
| PBBB Substance Abuse P. | 28.75 | 16.508 | 11.86 | 6.763 | 85.5 | -2.892 | .004 |
| PBCC Delinquent Pred. | 24.38 | 10.197 | 22.23 | 3.504 | 30 | -.636 | .525 |
| PBDD Impulsive Prop. | 26.5 | 13.32 | 15.05 | 5.753 | 84.5 | -2.632 | .008 |
| PBEE Anxious Feelings | 30 | 5.707 | 32.05 | 4.593 | 76.5 | -1.013 | .311 |
| PBFF Depressive Affect | 28.13 | 10.412 | 12.59 | 6.269 | 5 | -3.267 | .001 |
| PBGG Suicidal Tendency | 15 | 8.751 | 4 | 4.353 | 2.5 | -3.229 | .001 |
For both male and female subjects, the results of the MACI analysis in adolescents belonging to cluster 1 were found closer to the behavior of the scores of the patient population of the Chilean reference sample. In contrast, the results of the MACI analysis of adolescents belonging to cluster 2 were closer to the behavior of the scores of the non-patient population for the Chilean reference sample. Through the Biplot analysis, a visual analysis of the structure of the clusters was obtained for each sample (females and males), and the results are shown below in Figures 1 and 2.
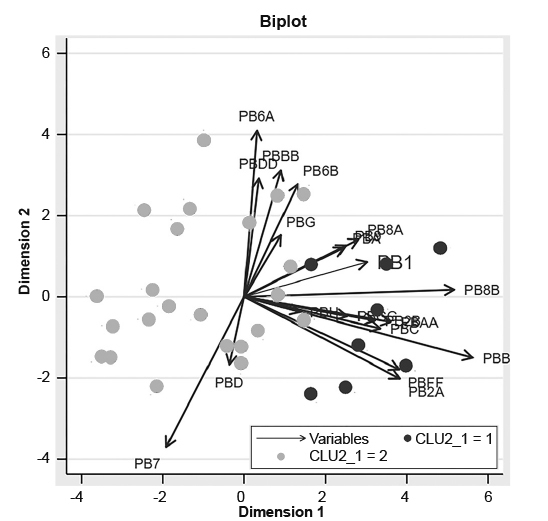
Figure 1. Biplot analysis for the female sub-sample based on the MACI’S personality patterns scales.
We used Chi-Square tests in order to analyze the independence of the variables studied (type of clinical presentation of ADHD, type of school attended, grade retention, comorbid diagnoses, ACEs, and use of medication) in relation to belonging to any of the clusters. It was only found that in the group of men, the presence of comorbidity was associated with cluster 1 membership (χ2 [1, N = 30] = 4.455 p < .05). No differences were found for the other variables.
Discussion and conclusion
This research provides a new approach to describe personality traits in Chilean adolescents diagnosed with ADHD through the MACI questionnaire. The MACI questionnaire was simple and quick to apply, and provided valuable information, not only for personality characteristics, but also for situations that require more advanced attention (expressed concerns) and for indicators of possible comorbid clinical syndromes. Despite being a small convenience sampling, adolescents with ADHD are significantly differentiated for some personality traits measured through the MACI questionnaire, when compared with the general population parameters. The personality profile for the group of women with ADHD resembles the non-patient reference group; on the other hand, the personality profile for the men’s group resembles that of the patient reference group. Based on these results, it can be stated that the group of female adolescent patients with ADHD included in this study had a more adaptive personality profile than the group of male subjects, which could lead to a lower risk of presenting personality disorder in the adulthood. On the other hand, special attention should be paid to the male patient population with ADHD to evaluate the need for preventive interventions in order to avoid the development of some type of personality disorder.
Follow-up studies of children with ADHD show that, compared with the general population, these children are at an increased risk for poorer functioning and to suffer future psychopathology ( Barkley, 2002 ; 2006 ; Biederman et al., 2006 ), including personality disorders ( Miller et al., 2008 ; Matthies & Philipsen, 2016 ). However, to our knowledge there are no studies that identify which children with ADHD are more likely to present a maladaptive personality functioning, which difficults the comparison of the results from this study with other research studies. There could be variables not studied here like the severity or persistence of the symptoms that could explain these maladaptive traits.
The cluster analysis and Biplot analysis applied to the sample detected two groups of personality sub-profiles in the adolescent patients with ADHD. Approximately 25% of the sample, for both men and women subjects, belongs to cluster 1 (women n = 8, 25.8% - men n = 8, 26.7%). Cluster 1 was characterized by higher scores on most scales in the MACI questionnaire, i.e., adolescents belonging to this cluster have a sub-profile pattern of a more maladaptive personality than the ones belonging in cluster 2. Based on these results, one could postulate that 25% of adolescents, both male and female presenting ADHD (belonging to cluster 1) may be at an increased risk of developing a personality with maladaptive traits, hindering the subject’s lifestyle. Also, the presence of these traits could be predisposing factors for the development of future psychopathology requiring further assessment to evaluate the need for more specialized interventions.
Belonging to cluster 1 or 2 is not associated with the type of clinical presentation of ADHD, use of medication, adverse childhood experiences (ACEs), grade retention, or type of school. Only the comorbidity variable in men, but not for the women, was associated with cluster 1 membership. Comorbidity is frequent in children, adolescents and adults, with ADHD, and it is likely that the presence of this trait in adolescents with ADHD impacts the natural history and prognosis of individuals, favoring the development of maladaptive personality traits. The fact that only the comorbidity variable was associated with cluster 1 membership in male adolescent with ADHD and not in females may be due to the fact that most of the women in this study had a comorbidity (71%), whereas in men it was less than half (43%), which makes comparative analysis difficult for the group of female subjects. It is possible that variables not included in this study mediate belonging to a certain type of cluster, among which could be found the severity and age of onset of ADHD symptoms, characteristics of parenting, family functioning, neurocognitive functioning, self-esteem, social competence, and genetic markers, among others ( Distel et al., 2011 ; Gómez & Corr, 2014 ; Matthies & Philipsen, 2016 ). Such variables could be included in subsequent studies and thus favor the detection of risk groups for the development of personality disorders in patients with ADHD.
Given these results and the importance of preventive interventions in the populations at risk, this research supports the suggestion to clinicians that considers the clinical characteristics of personality in the evaluation of adolescent patients with ADHD, since there would be a subgroup with maladaptive features that probably would require a meticulous detection of the factors that could be favoring the development of psychopathology. The Millon Adolescent Clinical Inventory (MACI-A) can be a useful tool in the early detection of maladaptive personality traits in adolescents with ADHD, which probably worsen the level of functioning of the individual. This study offers a tool for the evaluation and development of intervention strategies for adolescents affected by ADHD.
Limitations
The present study has several limitations that influence the interpretation of the results. The sample is not random or representative of the population and the sample size is small, which prevents the generalization of the results. Future research should include larger samples. In addition, the adolescents studied are patients, so there could be a subgroup of individuals who present severe and dysfunctional symptoms and who do not represent the population of adolescents with ADHD. Adolescents with hyperactive/impulsive ADHD are underrepresented (5% of the sample) and 57% have comorbidity, which could influence the results described. Although ADHD is highly comorbid, for future research it could be possible to compare groups of adolescents with ADHD with and without comorbidity and in this way assess whether ADHD is in itself predisposing the development of maladaptive personality traits, their comorbidities or both.
Because ADHD is a highly prevalent disorder in the child and adolescent population and is associated comorbidly with personality disorders in adulthood, it is important to consider that the approximately 25% of Chilean adolescents with ADHD present in this study, have important personality maladaptive features that could affect future functioning.











 nueva página del texto (beta)
nueva página del texto (beta)



