Introduction
Residential treatment is an important component of the management of substance use disorders (American Psychiatric Association & Work Group on Substance Use Disorders, 2010). In Mexico, governmental resources for mental health are scarce (Berenzon, Saavedra, Medina-Mora, Aparicio, & Galván, 2013), and while some private centers offer state-of-the-art, professional residential care, cost puts this kind of treatment out of reach for many users. Peer-support non-governmental centers for the residential treatment of addictions are therefore an important resource for people with few economic resources (Garcia, 2015; Lozano-Verduzco, Marín-Navarrete, Romero-Mendoza, & Tena-Suck, 2015; Marín-Navarrete et al., 2013). These centers employ different treatment models, generally including a combination of 12-step group sessions and involvement in the everyday chores of the center (such as cleaning, cooking, etc.). Few of them have health or mental health professionals as part of their staff, and they are usually directed by former drug users. This type of residential centers, sometimes called anexos, have also been accused of mistreatment and recurring to physical and emotional violence (Marín-Navarrete et al., 2013). Despite the importance of non-governmental faith-based rehabilitation centers in providing care to a high proportion of the most vulnerable drug users, still only a few studies have addressed their therapeutic procedures and outcomes (Marín-Navarrete et al., 2013).
Baja California has one of the highest drug use rates in Mexico, with a life time prevalence of 13.5%, as compared with 9.9% at the national level in 2016 (Instituto Nacional de Psiquatría Ramón de la Fuente Muñiz, Instituto Nacional de Salud Pública, Comisión Nacional Contra las Adicciones, & Secretaría de Salud, 2017). While there is no complete record of non-governmental treatment centers in Baja California, in 2013 there were 233 of them registered with the Ministry of Health, many of which were operated by Evangelical Pentecostal (EP) groups (Galaviz & Odgers, 2014).
Retention in treatment is associated with improved long-term results in areas as diverse as employment, social networks, criminality, substance use, and need of treatment re-entry (Evans, Li, & Hser, 2009; Garnick, Lee, Horgan, Acevedo, & Washington Circle Public Sector, 2009). Rates of retention in residential treatment vary worldwide, from as much as 88% for a 28-day treatment (McKellar, Kelly, Harris, & Moos, 2006) to around 50% for three-month programs (Meier & Best, 2006; Mulder, Frampton, Peka, Hampton, & Marsters, 2009). While longer periods of treatment are associated with better outcomes, a minimum period of three months is recommended by the American Psychiatric Association for the residential treatment of patients with substance use disorders (American Psychiatric Association & Work Group on Substance Use Disorders, 2010), and this period has also been associated with a significant improvement (as measured by change in frequency of substance use) on both primary and overall drug use among long-term residential treatment clients (Zhang, Friedmann, & Gerstein, 2003).
Many factors associated with treatment retention have been reported in the literature. Among them are older age (Arndt, Acion, & White, 2013; McKellar et al., 2006), higher educational attainment (Arndt et al., 2013), social support (Lang & Belenko, 2000; Lewandowski & Hill, 2009), and court-mandated admission (Arndt et al., 2013). Psychological traits such as better cognitive functioning (Aharonovich et al., 2006; McKellar et al., 2006), problem-oriented coping style and internal locus of control (Meier, Donmall, McElduff, Barrowclough, & Heller, 2006; Tate et al., 2008) can also influence retention. The pattern of drug use is associated with retention as well, as users of alcohol, marihuana, or amphetamines tend to stay in treatment longer than those of cocaine or heroin, and poly-users are less likely to complete treatment (Arndt et al., 2013).
The outcome of faith-based residential treatment for drug use is a relatively under-researched subject. Only a few studies have addressed retention in this context (Parhami, Davtian, Collard, Lopez, & Fong, 2014; Sung & Chu, 2013), and they report retention rates similar to those of other types of centers. Besides the factors already cited, retention in faith-based centers could be associated with the client’s spirituality at entry (Parhami et al., 2014), and also with religious conversion or the renovation of faith (Sung & Chu, 2013).
The objective of this study was to assess retention, and factors associated with it, for two faith-based non-governmental residential treatment centers in Tijuana, Baja California, Mexico. Based on findings reported by the previous literature, our hypotheses were that higher odds of retention would be associated with: older age, higher educational attainment, court-mandated admission, internal locus of control, use of substances other than cocaine or heroin and single-substance use, and higher religiosity and spirituality. We also hypothesized that specific religious affiliation would interact with the center’s religious orientation, so that when the orientation of client and center coincided, retention would be more likely.
Method
Sites
The study was conducted in two centers, henceforth referred to as C1 and C2. C1 is an EP center, directed by a minister, and the religious practices and belief system of Evangelical Pentecostalism form the chore of its treatment model (Odgers, Galaviz, & Hernandez, 2009; Stoll, 1990). C2 is 12-step based, and while spiritual aspects are considered central, it is not guided by a specific religion. Evangelical and Jehovah’s Witnesses services are common but not mandatory, and Catholic altars and images are present in the facilities. Both centers accept male drug and alcohol users from 18 years of age. They have weekly visits by physicians, who are available for emergency calls, but no mental health professionals. Both centers provide free (or payable with work at the center) attention to clients in need, and charge a fee to those who can pay that varies depending on the length of treatment and the client’s (or his family’s) ability to pay. During the study, fees varied from roughly $1,000 to $6,000 Mexican Pesos (≈ $50 - $300 US at the time of the study) for a three-month stay. This article is part of a wider study of the EP rehabilitation centers in Tijuana, and details of the story, characteristics, and treatment model of the centers can be consulted in previous articles (Galaviz & Odgers, 2014; Hernández & Ortiz, 2015). Recruitment for the study began in September 2014 and continued till June 2015.
Participants
All newly admitted clients (i.e., clients who were not already in the center at the time the study began) who fulfilled inclusion criteria and were willing to participate during the recruitment period. Inclusion criteria were: 1. age 18 years or older; 2. first admission at the center during the study period (i.e., no readmissions were included); 3. having no cognitive, language or other impediments to understand the informed consent procedure and answer the questionnaires; 4. agree to participation after an informed consent procedure.
Measures
We defined our outcome measure, retention, as having stayed in the center for at least 90 days. This was based on the one hand on the literature that suggests 90 days to be the minimum stay that provides significant benefits, and on the other because both centers defined their treatment as completed if the client had stayed for that period. We considered as retentions all clients who at the time of the 90-day follow-up either: 1. were still at the center; 2. had left the center because of conclusion of their treatment period (self-reported or according to the center’s records); 3. were at a different unit of the same center.
All independent variables were measured at baseline. Socio-demographic characteristics included age, education, marital status, and migratory experience in the United States. The last variable was included because in Tijuana some clients live in the United States and have come across the border for treatment, and some are return Mexican migrants (either voluntary or deported). Participants were also asked the motive of admission (response categories: voluntary, court-mandated, medical referral, school or workplace referral, and admitted at the request of family or friends).
We measured social support with the question “At the time of admission, were you in touch with your family?” (yes/no), and with the sum of four questions about perceived social support (e.g., “Do you usually have someone to show you love and affection?”) with answers ranging from “never” to “always”. Possible scores in the later ranged from 0-16, with a higher score indicating more perceived support.
We assessed cognitive state with the Mini-Mental State Examination (MMSE), in the Spanish version employed by Mexico’s Secretaría de Salud (Folstein, Folstein, & McHugh, 1975). Scores range from 0-30, with higher score indicating a better state. The MMSE has good sensitivity for the detection of cognitive impairment (77% in a study with older adults, with a false-positive rate of 16%) (Borson, Scanlan, Watanabe, Tu, & Lessig, 2005). Having no standardized cutoff points for adult Mexican population, we employed the 25th percentile of a Mexican older adult population (Mokri, Ávila-Funes, Meillon, Gutierrez, & Amieva, 2013), and excluded participants scoring 22 points or less.
Participants also completed the Brief Cope questionnaire in the Spanish version (Carver, 1997). The 24 items of the Brief Cope describe possible ways of responding to difficult or stressful situations, which are classified in 12 coping styles (Self-Distraction, Active Coping, Denial, Substance Use, Use of Emotional Support, Behavioral Disengagement, Venting, Positive Reframing, Planning, Humor, Acceptance, and Religion). The items corresponding to each style are summed to obtain style scores ranging from 2-8 (higher score indicates more frequent use of the coping style). The reliability of the 12 subscales included in the 24-item version of the Brief Cope ranges from Cronbach’s α = .50 to α = .82 (Carver, 1997). Following the Brief Cope authors’ recommendation, we employed for the analysis the score in each of the 12 styles as separate independent variables.
We evaluated locus of control with the Drug Related Locus of Control (DRLOC) questionnaire, a 15-item instrument that measures the perceived ability to control drug use, with a reliability coefficient Cronbach’s α = .81 and significant correlations with measures of addiction severity and self-esteem (Hall, 2001). The DRLOC consists of pairs of affirmations from which the participant must choose, one representing internal (scored as 1), and the other external locus of control (scored as 2). Following the authors recommendation, we averaged all 15 items for the analysis, for a resulting continuous score of 1-2, with a value closer to 1 indicating internal locus of control, and a value closer to 2 indicating an external locus of control.
To evaluate drug use in the previous month, participants were asked whether they had used each one of a list of substance types in the 30 days before admission to the center. We explored the association between each substance and retention, as well as the association between number of substances (1 vs. 2 or more) and retention. We also evaluated the association of retention with the number of previous residential and outpatient drug treatments.
To assess religiosity and spirituality, we employed the Duke University Religion Index (DUREL), a five-item inventory of participation in organized religious activities, participation in non-organized religious activities, and intrinsic religiosity (i.e., importance of spiritual aspects in the subject’s life). The three dimensions are scored and analyzed separately, with higher scores indicating more religiosity/spirituality. The score for organized religious activities is the answer to the first question (response range 1-6); the score for non-organized religious activities is the answer to the second question (response range 1-6, reverse coded); and the score for intrinsic religiosity is the average of the three remaining questions (range 1-5). In diverse studies, Cronbach’s α for DUREL ranges from .78-.91, and it has values of convergent validity with other measures of religiosity ranging from .71-.86 (Koenig & Büssing, 2010). Lastly, we analyzed the response to a question about religious affiliation at the time of admission. The responses to this question were classified as no religious affiliation, Catholic, Non-Catholic Christian, and other.
Procedures
During the recruitment period, research assistants visited the centers weekly, recording the number of new admissions from the centers’ registers and listing clients who had finished detox during the past seven days. Those who had finished detox in the previous seven days were invited to participate if they fulfilled the inclusion criteria. Those who agreed were screened with the MMSE (Folstein et al., 1975).
Follow-up interviews were conducted at 30, 60, 90, 120, and 180 days, from the date the participant had finished his detox period. A range of ± 10 days around the programmed date was accepted for the interview. Follow-ups took place either at common areas of the centers (taking care that no third person was within hearing distance), or by phone when the participant had already left the center. Although the follow-up questionnaires included the baseline instruments, however in this article our dependent variable of interest is retention and the baseline characteristics associated with it. Therefore, we use information only from the baseline questionnaire and data on retention at the 90-day follow-up.
All field procedures were conducted by previously trained research assistants with at least some college education. The training included reviewing the aims of the project and the objective of each part of the questionnaire and practicing the application of questionnaires with members of the research group. A psychologist with a PhD in Neurosciences and experience in the application and research-related use of the MMSE provided training for the application of that instrument.
Statistical analysis
First, we conducted descriptive analyses of retention and of baseline characteristics of participants, overall and by center. To further explore the association between each independent variable and the dependent variable, we fitted bivariate models, stratified by center. As retention is a dichotomous outcome, with value of one if the participant had completed three months in treatment, and zero if he had not completed that period, we employed logistic regression to model the association.
Our main purpose in the statistical analysis was to assess the association between the independent variables and retention in treatment. We began with a model with all independent variables, and then sequentially eliminated variables with the higher p-values. We first obtained one model for each center, to observe if the independent variables associated with retention differed by center. Afterwards, we fitted a model for both centers, with the center as a further independent variable. We explored interaction terms of center-by-independent variable, for those independent variables that had shown differential effects between centers in the previous steps, and retained interactions with p < .05. We assessed the fit of the model for both centers with the same criteria as above. Missing data were handled with case-wise deletion. All analyses were conducted with Stata (Version 13) (StataCorp, 2013).
Ethical considerations
The Ethics Committee reviewed and approved all procedures in the study, and participants read and signed an informed consent form. The confidentiality of participants was guaranteed using an identification number in questionnaires (i.e., no name was registered in the questionnaires or data bases). Names and contact data of participants were kept in a password-protected file. Consent forms were kept in a locked drawer.
Results
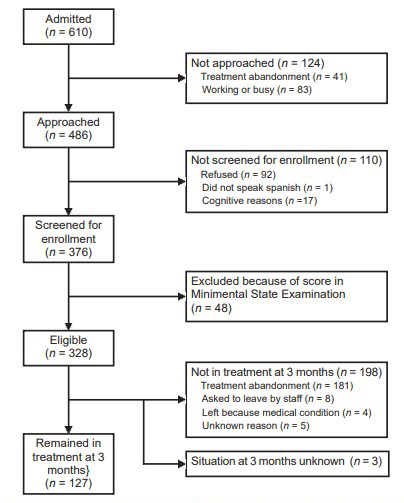
During the recruitment period, 610 clients were admitted to the centers, of which 486 (79.7%) were invited to participate (Figure 1). Of those admitted, 6.7% (41/610) abandoned treatment less than seven days after admission, so it was not possible to approach them during the weekly visits of the research team. A further 83 clients (13.6% of those admitted) were not approached because the staff reported they were working or otherwise engaged at the time of the research team visit. According to the researchers’ observations, some of them might have already left the center at the time, while others would be best described as polite refusals. The baseline questionnaire was responded by 328 participants (53.8% of admissions). At the 90-days follow-up, 127 of them were still in or had completed treatment, for a retention rate of 38.7% (127/328). Assuming a scenario where all admissions for which there was no information had completed or were still in treatment at three months, the retention rate would have been 60.8% (371/610). Conversely, on a worst-case scenario, where all of them had abandoned treatment, the retention rate would have been 20.8% (127/610). The retention rate among those who completed the baseline interview was 32.5% (52/160) for C1, and 44.6% (75/168) for C2. Regretfully, the centers do not keep complete records on all admissions, so it is not possible to compare the characteristics of those who answered the baseline questionnaire, with those of all admitted.
In Table 1 we show the baseline characteristics of the 328 eligible participants. Mean age was 33.1 years, and the more frequently consumed drug was methamphetamine. Those who started treatment at C2 were slightly older, a higher percentage had lived in the United States, and the prevalence of heroine/opioid use in the last 30 days was also higher. The average score in the Intrinsic Religiosity sub-scale of the DUREL was higher in C1. A higher percentage of participants self-declared as Non-Catholic Christian in C1, while a lower percentage of participants had no religious affiliation. Scores in the Brief Cope subscales were similar between centers, except for a higher score in the Venting copying style (e.g., “I expressed my negative feelings”) in C2 (not shown in Table 1). Of notice, none of the participants had been admitted by legal request (court-mandated admission): the only observed motives of admission were either voluntary or at the request of family or friends.
Table 1 Baseline characteristics of participants, total and by center
| Variable | Center 1 (n = 160) | Center 2 (n = 168) | Total (n = 328) | p-value 1 |
|---|---|---|---|---|
| Age (M, S.D.)2 | 31.9 (11.0) | 34.2 (10.7) | 33.1 (10.9) | .052 |
| Education (%) | ||||
| Elementary or less | 24.5 | 25.6 | 25.1 | .623 |
| Junior high | 39.0 | 32.7 | 35.8 | |
| High school | 33.3 | 36.9 | 35.2 | |
| College or more | 3.1 | 4.8 | 4.0 | |
| Marital status (%) | ||||
| Single | 56.9 | 46.7 | 51.7 | .177 |
| Married/common law | 30.0 | 35.9 | 33.0 | |
| Separated/divorced/widowed | 13.1 | 17.4 | 15.3 | |
| Ever lived in the United States (%) | 48.1 | 62.3 | 55.4 | .010 |
| In touch with family (%) | 84.9 | 80.7 | 82.8 | .318 |
| Social support score (M, S.D.) | 12.4 (3.5) | 12.1 (3.6) | 12.3 (3.6) | .413 |
| Motive of admission (%) | ||||
| Voluntary | 66.0 | 56.0 | 60.9 | .062 |
| At request of family/friends | 34.0 | 44.1 | 39.1 | |
| MMSE2 (M,S.D.) | 26.7 (2.2) | 26.9 (2.2) | 26.8 (2.2) | .470 |
| Previous month use (%) | ||||
| Alcohol | 69.6 | 63.2 | 66.4 | .223 |
| Cocaine/crack | 19.1 | 17.2 | 18.1 | .654 |
| Metamphetamine/amphetamine | 81.7 | 81.6 | 81.6 | .991 |
| Heroine/opioids | 8.3 | 27.6 | 18.1 | < .001 |
| ≥ 2 drugs | 59.5 | 66.9 | 63.2 | .171 |
| Previous treatment (median, IQR2) | ||||
| Residential | 1 (0-3) | 2 (0-5) | 1 (0-4) | .109 |
| Outpatient | 0 (0-1) | 0 (0-1) | 0 (0-1) | .075 |
| Previous treatment (median, IQR2) | ||||
| Organized religious activities | 2.8 (1.8) | 2.5 (1.5) | 2.7 (1.7) | .173 |
| Non-organized religious activities | 2.6 (1.8) | 2.9 (1.8) | 2.8 (1.8) | .276 |
| Intrinsic religiosity | 4.0 (1.2) | 3.7 (1.4) | 3.8 (1.3) | .042 |
| DUREL2 | ||||
| None | 31.8 | 39.5 | 35.8 | .004 |
| Catholic | 19.5 | 29.6 | 24.7 | |
| Non-Catholic Christian | 42.9 | 24.1 | 33.2 | |
| Other | 5.8 | 6.8 | 6.3 | |
Note: 1 p-value for difference between centers. χ2 test for difference of percentages, t test for difference of means, rank sum test for variables with non-normal distribution; 2MMSE = Mini-mental State Examination; IQR = inter-quartile range; DUREL = Duke University Religion Index.
In Table 2 we show the associations of the independent variables with retention, stratified by center. In C1, older age was associated with higher odds of retention, while the Behavioral Disengagement copying style (e.g., “I gave up”) was associated with lower odds. There was a significant bivariate association between retention and the religion copying style (e.g., “I prayed or meditated”), but it disappeared after adjusting for other variables. Methamphetamine use was associated with higher odds of retention. Catholic and Non-Catholic Christian religious affiliation were also associated with retention. In C2, having lived in the United States and having been admitted at the request of family or friends were associated with higher odds of retention, while using heroin/opioids was associated with lower odds.
Table 2 Association of baseline characteristics with retention in treatment at three months (stratified by center)
| Center 1 | Center 2 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Crude OR1 |
95% CI | 95% CI | p value | Adjusted OR2 |
95% CI | 95% CI | p value | Crude OR1 |
95% CI | 95% CI | p value | Adjusted OR2 |
95% CI | 95% CI | p value |
| Age | 1.04 | 1.01 | 1.07 | .010 | 1.04 | 1.00 | 1.08 | .036 | 1.02 | .99 | 1.05 | .143 | ||||
| Education | ||||||||||||||||
| Elementary or less | Ref. | Ref. | ||||||||||||||
| Junior high | .9 | .38 | 2.13 | .819 | 1.49 | .65 | 3.42 | .349 | ||||||||
| High school | 1.12 | .47 | 2.67 | .802 | 2.61 | 1.16 | 5.89 | .021 | ||||||||
| College or more | .67 | .06 | 7.05 | .736 | 2.07 | .45 | 9.52 | .350 | ||||||||
| Marital status | ||||||||||||||||
| Single | Ref. | Ref. | ||||||||||||||
| Married/common law | .76 | .35 | 1.66 | .497 | .75 | .38 | 1.48 | .402 | ||||||||
| Separated/divorced/widow | 1.50 | .57 | 3.95 | .412 | 1.25 | .53 | 2.94 | .608 | ||||||||
| Ever lived in the United States | 1.21 | .62 | 2.35 | .575 | 2.12 | 1.11 | 4.06 | .024 | 3.32 | 1.58 | 6.99 | .002 | ||||
| In touch with family | 2.82 | .91 | 8.74 | .072 | 2.30 | .99 | 5.37 | .053 | ||||||||
| Social support score | 1.00 | .91 | 1.10 | .999 | .99 | .91 | 1.08 | .851 | ||||||||
| Motive of admission | ||||||||||||||||
| Voluntary | Ref. | Ref. | Ref. | |||||||||||||
| At request of family/friends | .72 | .35 | 1.47 | .363 | 2.64 | 1.41 | 4.96 | .002 | 2.67 | 1.34 | 5.33 | .005 | ||||
| MMSE 3 | .99 | .85 | 1.15 | .926 | .99 | .86 | 1.14 | .906 | ||||||||
| Brief Cope | ||||||||||||||||
| Self distraction | .99 | .83 | 1.18 | .943 | 1.11 | .94 | 1.31 | .233 | ||||||||
| Active coping | .99 | .83 | 1.19 | .915 | 1.00 | .85 | 1.18 | .995 | ||||||||
| Denial | .94 | .79 | 1.12 | .465 | .90 | .77 | 1.05 | .166 | ||||||||
| Substance use | .98 | .84 | 1.16 | .852 | .93 | .80 | 1.08 | .331 | ||||||||
| Use of emotional support | 1.03 | .88 | 1.19 | .736 | 1.07 | .93 | 1.23 | .323 | ||||||||
| Behavioral disengagement | .85 | .73 | 1.00 | .047 | .82 | .68 | .98 | .030 | .95 | .82 | 1.09 | .434 | ||||
| Venting | .96 | .82 | 1.13 | .604 | 1.07 | .91 | 1.28 | .413 | ||||||||
| Brief Cope | ||||||||||||||||
| Positive reframing | .98 | .82 | 1.16 | .796 | 1.05 | .90 | 1.24 | .533 | ||||||||
| Planning | 1.16 | .97 | 1.40 | .107 | .92 | .78 | 1.09 | .334 | ||||||||
| Humor | .90 | .77 | 1.06 | .212 | 1.03 | .90 | 1.18 | .675 | ||||||||
| Acceptance | 1.19 | .95 | 1.49 | .132 | .90 | .74 | 1.10 | .301 | ||||||||
| Religion | 1.19 | 1.03 | 1.39 | .022 | .96 | .83 | 1.11 | .567 | ||||||||
| DRLOC3 | .87 | .18 | 4.09 | .859 | .24 | .06 | 1.00 | .050 | ||||||||
| Previous month use | ||||||||||||||||
| Alcohol | 1.38 | .65 | 2.92 | .400 | 1.24 | .65 | 2.37 | .506 | ||||||||
| Cocaine/crack | .45 | .17 | 1.18 | .105 | .67 | .29 | 1.57 | .360 | ||||||||
| Metamphet/amphetamine | 2.08 | .79 | 5.48 | .139 | 3.95 | 1.17 | 13.27 | .026 | 1.29 | .58 | 2.89 | .538 | ||||
| Heroine/opioids | .59 | .16 | 2.26 | .444 | .39 | .18 | .81 | .012 | .35 | .15 | .78 | .011 | ||||
| ≥ 2 drugs | .61 | .31 | 1.19 | .146 | .74 | .39 | 1.43 | .372 | ||||||||
| Previous treatment | ||||||||||||||||
| Residential | 1.00 | .93 | 1.07 | .981 | 1.01 | .97 | 1.06 | .509 | ||||||||
| Outpatient | .97 | .82 | 1.16 | .753 | 1.02 | .97 | 1.08 | .392 | ||||||||
| DUREL3 | ||||||||||||||||
| Organized religious acts | 1.16 | .96 | 1.39 | .115 | .98 | .80 | 1.20 | .832 | ||||||||
| Non-organized religious acts | 1.33 | 1.10 | 1.60 | .003 | 1.22 | .97 | 1.53 | .084 | 1.04 | .88 | 1.24 | .625 | ||||
| Intrinsic religiosity | 1.28 | .95 | 1.73 | .107 | .99 | .79 | 1.24 | .927 | ||||||||
| Religious affiliation | ||||||||||||||||
| None | Ref. | Ref. | Ref. | |||||||||||||
| Catholic | 3.62 | 1.26 | 10.42 | .017 | 3.24 | 1.03 | 10.13 | .044 | .97 | .46 | 2.07 | .942 | ||||
| Non-Catholic Christian | 3.33 | 1.35 | 8.23 | .009 | 2.70 | 1.01 | 7.21 | .047 | 1.19 | .53 | 2.64 | .674 | ||||
| Other | 1.46 | .26 | 8.38 | .668 | 1.67 | .26 | 10.80 | .592 | 1.04 | .29 | 3.77 | .950 | ||||
Note: 1Bivariate logistic regression, dependent variable: three-month retention. Sample size varies depending on missing data; 2Multivariate logistic regression, dependent variable: three-month retention, adjusted by all variables with coefficients in column. C1 n = 149, C2 n = 162. 3MMSE: Mini-mental State Examination; DRLOC: Drug Related Locus of Control; DUREL: Duke University Religion Index.
In the final model combining data from both centers (Table 3), older age was associated with higher odds of retention, and using heroin/opioids with lower odds. As shown by the center-by-referral source interaction, having been admitted at the request of family or friends was associated with retention in C2, while no association was observed in C1. The center-by-religious affiliation interaction coefficient shows that in C1 being Catholic or Non-Catholic Christian was associated with retention, while in C2 religious affiliation had no observable effect. The interaction term can also be read as showing that those with no religious affiliation were more likely to stay in treatment in C2 than in C1, while for those with a religious affiliation the odds of staying were similar between centers.
Table 3 Association of baseline characteristics with retention in treatment at three months (both centers)
| Variable | OR 1 | 95% CI | 95% CI | p-value |
|---|---|---|---|---|
| Center (reference C1) | 2.74 | .95 | 7.85 | .061 |
| Age | 1.04 | 1.01 | 1.06 | .002 |
| Motive of admission | ||||
| Voluntary | Ref. | |||
| At request of family/friends | .85 | .38 | 1.87 | .680 |
| C2* Admitted at request of family/friends | 3.41 | 1.19 | 9.72 | .022 |
| Used heroine/opioids in past month | .50 | .25 | 1.00 | .049 |
| Religious affiliation | ||||
| None | Ref. | |||
| Catholic | 3.77 | 1.27 | 11.20 | .017 |
| Non-Catholic Christian | 3.03 | 1.19 | 7.74 | .020 |
| Other | 2.11 | .35 | 12.71 | .415 |
| C2*Catholic | .19 | .05 | .74 | .017 |
| C2*Non-Catholic Christian | .40 | .11 | 1.40 | .150 |
| C2*Other | .61 | .06 | 5.92 | .670 |
Note: 1Multivariate logistic regression, dependent variable: three-month retention, adjusted by all variables in Table. N = 313.
Discussion and conclusion
The 38.7% three-month retention rate in this study is low, but within previously reported ranges. Although differences in follow-up time make comparisons difficult, in the Christian residential treatment studied by Sung and Chu (2013), the 18-month retention was 18%, and in the study by Parhami et al. (2014) of a Jewish religious treatment center the six-month rate was 55%. In non-religious centers, retention rates also vary widely (McKellar et al., 2006; Meier & Best, 2006; Mulder et al., 2009).
Similar to the findings of another study (Arndt et al., 2013), age had a direct association with retention. We cannot explain this finding, but from field observations we believe that it might be the case that older drug users are readier for a “time out” of drug use due to the physical consequences of it. However, the association could also be due to confounding by unmeasured variables.
On the other hand, social support has been shown to increase drug treatment retention (Lang & Belenko, 2000; Lewandowski & Hill, 2009). While we did not find an association with contact with family or perceived social support, the association between admission at family/friends request and retention might in part be explained by closer social relationships. Field observation in C2 showed that those admitted at family request were placed in a more closely monitored sleeping area within the center. However, an analysis adjusting for sleeping area still showed a significant association between admission at request of family/friends and retention in C2, so we might speculate that for this study the variable was a proxy, either of special living conditions within the center, or of other effects of family involvement in the client’s treatment.
As opposed to other studies (Meier et al., 2006; Tate et al., 2008), none of the psychological variables explored had an association with retention in the multivariate model. On the other hand, heroin/opioid use was associated with lower odds of retention, as has been reported before (Arndt et al., 2013). This might be due to the strong addictive properties of this group of substances, combined with the lack of a specific therapy for the management of withdrawal in the participant centers. In future studies, it will be interesting to continue exploring if and which psychological traits are associated with retention in this population, and how to address the needs of clients with different drug use patterns.
Regarding the religious aspects, it is interesting to notice that C1, the EP center, received more clients who were affiliated with a religion and spiritually oriented. In addition, those who started treatment at C1 were more likely to stay if they were either Non-Catholic Christian or Catholic, as compared to those without religious affiliation. The association was more marked amongst Catholics. Although any interpretation is speculative, we think this indicates that having a religious or spiritual disposition facilitated retention in C1, where religious aspects were a more salient part of the treatment. While it could be hypothesized that the concordance between the specific religious affiliation of center and client would be important in this regard, according to our data it was not concordance in affiliation (i.e., being a Non-Catholic Christian in a Non-Catholic Christian center), but the agreement between the general religious orientation of client and center, that was associated with increased retention. At C2, where religion has a less salient place in the treatment model, most clients had no religious affiliation, and affiliation made no difference in terms of retention. Conversely, for those with no religious affiliation retention was significantly higher at C2. These results suggest that the outcome of treatment in faith-based centers might depend on the initial religious/spiritual condition of the client. However, the interrelations between religion and spirituality, and mental health treatment, are very complex (Vanderpot, 2014), and more in-depth exploration is guaranteed.
An important limitation of our data is the high proportion of those admitted at the centers that were not enrolled in the study. Given the lack of information about those not enrolled, it is difficult to assess the representativeness of our sample. The participants’ distribution by age and drug of use was similar to what is reported for Baja California by the national addiction surveillance system (Secretaría de Salud, 2015), but we cannot assess if they were comparable in terms of other characteristics. Thus, a recommendation for future studies in this type of centers is that the research team collects its own statistics of admissions to assess selection bias. Another limitation of our study was that, having collected data in only two centers, the results cannot be generalized to the population of non-governmental centers in either Tijuana or Mexico.
To conclude, the faith-based centers in this study had a low retention rate that was associated with personal religious affiliation in the EP center. This suggests that a match between a person’s religious convictions and those of the center could be important for retention. In the absence of sufficient public services for substance use disorders in Mexico’s health system (Garcia, 2015; Lozano-Verduzco et al., 2015; Marín-Navarrete et al., 2013), the initiatives of civil society and religious groups will continue being the main source of attention for the most vulnerable population. In this context, more research is needed to clarify the utility of faith-based centers for religious and non-religious drug users, and to suggest ways of improvement.











 nueva página del texto (beta)
nueva página del texto (beta)