INTRODUCTION
Delirium is a neurocognitive disorder characterized by an acute or subacute onset and a fluctuating course (Meagher, 2001). Clinical features include a mix of cognitive and behavioral symptoms, including an inability to maintain focus and attention, diminished level of consciousness, global cognitive decline, delusional-hallucinatory phenomena, disturbances in the circadian rhythm, mood swings, and gross disturbances of behavior (Bush et al., 2014; Ramirez-Bermudez et al., 2006). According to its psychomotor presentation, delirium can be classified in hypoactive, hyperactive, or mixed (American Psychiatric Association, 2013). The etiologies of delirium are diverse and multifactorial, usually reflecting the combination of predisposing and precipitating (usually modifiable) causes (Fong, Tulebaev, & Inouye, 2009).
In oncology palliative care services, delirium is frequently present, with a prevalence varying from 13% to 42% on admission, 26-62% during admission, and up to 58-88% in the weeks or hours preceding death (Hosie, Davidson, Agar, Sanderson, & Phillips, 2013). In this population, delirium can be reversible in 30-50% of cases (Leonard et al., 2008), since its main etiologies include the use of medications (e.g., opiates, benzodiazepines), infections, electrolytic misbalance, and dehydration (de la Cruz, Ransing, et al., 2015). The frequency of each psychomotor subtype in palliative care patients varies among studies, probably due to different populations and classification criteria. In a sample of 556 palliative care patients (de la Cruz, Ransing, et al., 2015), using DSM-IV TR criteria, the mixed subtype was the most frequent (45%), followed by hypoactive (30%) and hyperactive (25%).
Delirium increases morbidity (Gustafson et al., 1988), causes distress to patients, family members, and health care professionals (Breitbart, Gibson, & Tremblay, 2002; Bruera et al., 2009). It increases also health expenditure (de la Cruz, Ransing, et al., 2015). Moreover, the presence of delirium diminishes survival in palliative care patients, even as early as 21 days after its onset (Caraceni et al., 2000; Lawlor et al., 2000), and next to performance scales (e.g., Karnofsky Performance Status, Eastern Cooperative Oncology Group Scale), it is an important factor in clinical indexes designed to predict mortality among the same population (Baba et al., 2015; Scarpi et al., 2011). Regardless of the high prevalence reported, delirium is still underdiagnosed and/or mistreated in patients suffering from cancer (Wada, Wada, Wada, & Onishi, 2010), perhaps because of its fluctuating course and the lack of an intentional search for the syndrome by the health care staff (Inouye, 2006). Besides the impact in patients’ outcomes (de la Cruz, Fan, et al., 2015), a non-recognized or mistreated delirium leads to unnecessary treatments and delays in end-of-life issues (Reddy, Nguyen, El Osta, & Bruera, 2008).
In order to improve the quality of care among oncologic palliative care patients, it is necessary to study the presence of delirium and its impact on survival to develop strategies aimed at prevention, opportune diagnosis, and treatment. Our main goal was to describe the frequency and clinical characteristics of delirium, as well as to analyze its impact on short-term survival (30 days), in a sample of palliative care inpatients treated in a tertiary center. As secondary objectives, we searched for the percentage of missed delirium diagnosis by the primary oncologic team; finally, we sought for correlations between performance indexes and survival rates.
METHOD
Participants
We performed a prospective study, including all the inpatients referred to the Palliative Care Service of the Instituto Nacional de Cancerología in Mexico City, from August, 2014 to March, 2015, who were not in deep sedation (Ramsay Sedation Scale ≥ 5). Informed consent was obtained from patients who were able to completely understand the purpose of the study; otherwise, informed consent was obtained from a family member. Admission to a Palliative Care Service requires a diagnosis of advanced stage cancer and: a) score ≥ 3 in the Eastern Cooperative Oncology Group Scale (ECOG) (Oken et al., 1982) or b) at least two of the next conditions: ECOG score of 2; uncontrolled pain or other significant symptom (e.g., dyspnea, seizures, persistent vomiting); family distress, which is based in clinical judgment, and includes any familiar issue that can affect negatively a patient’s wellbeing (e.g., family overload, difficulties in organizing to improve the patient’s care); frequent admissions as inpatient in the last months (≥ 2 per month); psychosocial distress, also based in clinical judgment, and includes difficulties in economic, logistic, and emotional areas of the patient (e.g., patient living far away from the hospital and needing physical assistance, psychiatric and psychological symptoms); hospitalization longer than a week without significant improvement (Allende-Pérez, Verástegui-Avilés, Chavira-Estefan, Tejeida-Bautista, & Dominguez-Ocadio, 2013). When patients are referred to the Palliative Care Service by the leader of a primary referring team (medical oncologist, oncologist surgeon, or haemato-oncologist), a medical palliative care specialist determines their acceptance and then the palliative team performs an evaluation to prescribe the initial treatment.
Instruments and procedure
Once a patient was included in the Palliative Care Service and the initial assessment was performed, we reviewed the clinical file and carried out a short interview to collect clinical and socio-demographic data. We also looked through the medical records to determine if the patient was diagnosed with delirium in the previous five days. Subsequently, the palliative care psychiatrist (OR-M), blinded to the information in the medical file, assessed the patient’s status (delirium/non-delirium) using the Spanish version of the Confusion Assessment Method (CAM) (Gonzalez et al., 2004). Patients diagnosed with delirium were also evaluated to determine its subtype in an interview based on DSM-5 criteria (hypoactive, hyperactive, or mixed). Finally, the ECOG (Oken et al., 1982) and the Karnofsky Performance Status (Yates, Chalmer, & McKegney, 1980) were applied to stablish performance status. As per protocol in the Palliative Care Service, patients were evaluated by a physician of the team on a daily basis as inpatients, and once or twice per month after discharge until death. If patients missed an appointment, a call center team (conformed by physicians) contacted them or a family member, so we could know their survival status (alive/dead). If the patient was deceased, a note was written on the electronic clinical file. In June, 2015 we reviewed the clinical files of all the patients included, so we could know their survival status. In the event that a patient had died, we investigated the date of decease to establish the survival time since the initial assessment.
Statistical analysis
We used descriptive statistics to report socio-demographic data (mean and standard deviation for continuous variables, frequencies and percentages for nominal variables). Differences among groups (delirium/non-delirium) in all categorical and numerical variables were analyzed using χ2 and independent sample t tests, respectively. Any statistically significant difference was posteriorly evaluated as a covariate in a Cox-Regression model. We used the Kaplan-Meier estimate to know the survival function of delirium and non-delirium patients at 30 days of inclusion, and performed a Log-Rank test to determine any statistical significant difference between both groups. Missed diagnosis of delirium by the primary referring team was expressed in percentage. Correlations between medical status (delirium/non-delirium) and ECOG, Karnofsky Performance Status, or site of primary tumor were performed using χ2. A cutoff point for significance was stablished at p < .05. All analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 20.
Ethical considerations
According to the Mexican Law for clinical research, the study is considered a minimum risk study (Secretaría de Salud, 2014), and was approved by the Ethics Committee of the Instituto Nacional de Cancerología in Mexico City.
RESULTS
We included 174 patients for initial assessment. Since 22 of them could not be found to determine their survival status, they were included as non-censored cases for the survival analysis. The mean age of the sample was 50.91 years (SD = 16.02) and 63.2% (n = 110) were women. Seventy patients (40.2%) were diagnosed with delirium, the most frequent subtype corresponded to hypoactive (45.7%), followed by mixed (42.9%) and hyperactive (11.4%).
Mean survival time in patients with delirium was 11 days [95% CI = 8.5, 13.9] while, in non-delirium patients, it was 21 days, [95% CI = 18.3, 22.72]; Log Rank 23.50, df= 1, p < .001. The t-test for age showed a significant difference between delirium and non-delirium groups, Ms = 55.60, 47.75 respectively, p < .001. For the latter, we conducted a Cox-Regression model using age as a covariable. In Cox-Regression, age was not a significant factor (χ2= .81, df= 1, p= .37) (Figure 1).
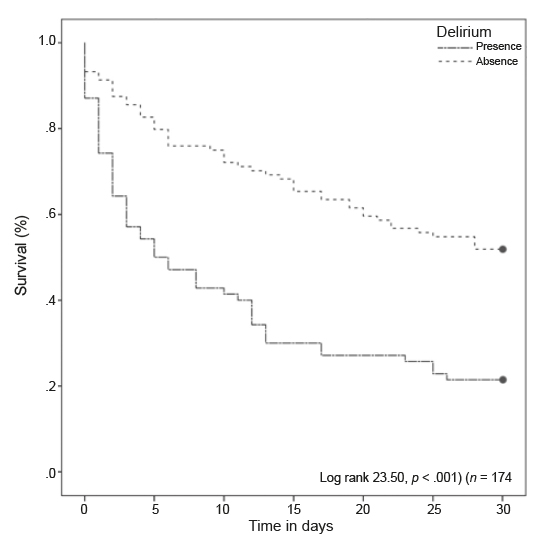
Figure 1 Kaplan-Meier curve of overall survival in patients with delirium versus those who did not had delirium.
Only 23% of delirium cases were correctly diagnosed by the primary referring team. The presence of delirium was directly associated with the ECOG score (χ2 = 24.28, df = 4, p < .001) and indirectly associated with the Karnofsky Performance Status (χ2 = 43.75, df = 9, p < .001).
DISCUSSION AND CONCLUSION
Survival in palliative care population has become an important study topic, as shown by the continuous development of indexes to predict survival (Baba et al., 2015). In our study, we found that the presence of delirium at the initial evaluation reduced life expectancy by 50% at 30 days. These numbers are also in agreement with the findings in other centers of advanced cancer patients (Caraceni et al., 2000; Hui et al., 2012). Age was found as a risk factor for the development of delirium, as previously reported (Elsayem et al., 2010); however, it was not relevant to determine survival. Other studies in advanced cancer patients have also found delirium as the main factor to predict short-term mortality, even when there are not differences between groups’ age (de la Cruz, Ransing, et al., 2015; Lawlor et al., 2000).
Our delirium prevalence is similar to those reported in acute palliative care services/units from other countries (de la Cruz, Ransing, et al., 2015; Lawlor et al., 2000). We believe this finding may be due to the fact that these populations share characteristics like advanced cancer stages, age, and low performance status. Although we used a different instrument to diagnose delirium (CAM) than the one used in other studies from acute palliative care services (Memorial Delirium Assessment Scale), previous studies have demonstrated no significant differences among different delirium diagnostic scales (Wong, Holroyd-Leduc, Simel, & Straus, 2010). The most frequent subtype of delirium was hypoactive, followed closely by the mixed subtype, a similar result to that reported in a larger series (Stagno, Gibson, & Breitbart, 2004). A possible explanation for this finding is our use of DSM criteria to classify delirium’s subtype, and similarities among populations. Other studies have found the mixed subtype as the most frequent (de la Cruz, Ransing, et al., 2015), although they use different methods to establish the delirium subtype. The reason for this discrepancy could be explained by differences in our populations.
Early identification of delirium could reduce mortality (de la Cruz, Ransing, et al., 2015), patient and family distress (Bruera et al., 2009), length and cost of hospitalization (Ely et al., 2001), and caregiver burden (Breitbart et al., 2002). Unfortunately, we found a 73% of undetected delirium diagnosis in the primary referring team, which is somewhat higher than the 61% rate found in other centers (de la Cruz, Fan, et al., 2015). This discrepancy could be explained by the sample size, but another possible reason could be that there is a less intentional search for delirium, due to a lack of training or an overload of the health staff. Nevertheless, we believe that continuous education about prevention, early detection, and thorough assessment of delirium will benefit the well-being of palliative care patients (Bush et al., 2014). We could probably benefit from the development and application of clinical guidelines for delirium diagnosis and treatment in this population, similar to those we have in other settings (Secretaría de Salud, 2016).
Finally, we also found that a low performance status (defined by the ECOG and Karnofsky scores) is associated with the presence of delirium. Other studies in palliative care and non-palliative care patients have found this association (de la Cruz, Ransing, et al., 2015), showing that the most frail and sick patients are in greater danger of presenting delirium in palliative care services.
Our study is not without limitations, starting with a relative small sample size compared to other studies (Caraceni et al., 2000; de la Cruz, Fan, et al., 2015). The sample size stopped us from performing more sophisticated analysis, combining several variables (e.g. type of primary tumor, body mass index, etc.) (Agar et al., 2017; Agar et al., 2016; de la Cruz, Ransing, et al., 2015; Maltoni et al., 2005; Perez et al., 2017) to generate a model that predicts mortality. To our knowledge, this is the first description of the prevalence and characteristics of delirium in a Mexican Palliative Care Service. We think that this effort is a step to start in the development of national statistics and new investigations in palliative care patients.











 text new page (beta)
text new page (beta)


