BACKGROUND
Cannabis is the illegal drug with the highest prevalence of use worldwide, with usage rates of 3.9% across all cultures, and representing 180.6 million users, 13.1 million of which meet dependency criteria (Degenhardt et al., 2013). The past two decades saw an increase in cannabis use that appears to have stabilized in many European countries, although there are still high levels of use, especially among the adolescent population, coupled with a lifetime prevalence of use of 23.8.% among adult Europeans (80.5 million) (European Monitoring Center for Drugs and Drug Addiction, 2010).
The problem of cannabis use in adolescents has been documented in Europe (European Monitoring Center for Drugs and Drug Addiction, 2010), North America (Currie et al., 2012), and Latin America, where marijuana is said to be the most commonly used illegal drug among high school students (Inter-American Commission for the Control of Drug Abuse, 2006). Most countries in the Americas have witnessed an increase in cannabis seizures in recent years, particularly those in South America (United Nations Office on Drugs and Crime, 2008).
Studying the child-youth population is important because early onset of use (before age 15), associated with chronic use in young people increases cognitive impairment in executive and neurocognitive functions (Curran et al., 2016; Fontes et al., 2011), and may be associated with the development of dependency in adulthood (Gonzalvo, Barral, Grau-López, Esteve, & Roncero, 2011). This high use may be partly due to the fact that people tend to consider this drug as one of the least harmful in the short and long term, compared with other substances. In addition, cannabis use at early ages could have consequences at the cerebral level since neurodevelopment continues to occur at this stage (Parolaro, 2010).
Due to the serious consequences mentioned earlier with respect to early cannabis use, a review of articles associating psychopathology with early vs. late cannabis use is proposed. It is also suggested that early cannabis use leads to greater exposure of the Central Nervous System to this substance and, therefore, a greater risk of the presence of psychopathological alterations. The purpose of this review is to describe the relationship between early cannabis use and the development of mental disorders.
METHOD
A narrative review was conducted of longitudinal studies on humans, which associated early cannabis use with mental disorders (psychosis, schizophrenia, bipolar disorder, depression, and anxiety). Given that the concept of early onset of cannabis use varies, studies were included that focused on cannabis use during adolescence and more emphasis was placed on studies that clearly distinguish between early vs. late cannabis use. On the other hand, only longitudinal studies that provide data on incidents and cause-effect correlations with greater scientific evidence than other types of studies were chosen (Bel, Inglés, & Piñol, 2009). A search of the PubMed database was conducted until December 31, 2016. Cannabis combinations have been used with other keywords: age of onset, mental disorders, psychosis, schizophrenia, depression, anxiety, and bipolar disorder. In addition, bibliographic citations from reviews and meta-analyses in this topic were manually reviewed in order to find additional studies with the characteristics we were looking for (longitudinal studies).
RESULTS
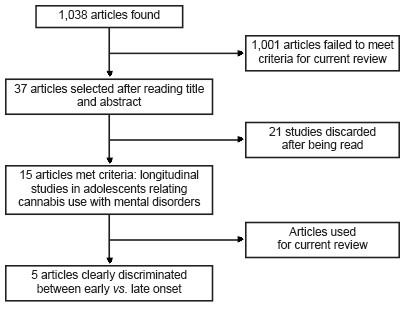
A total of 1038 articles were found, and after reviewing the titles and abstracts, 37 articles were selected for reading (Figure 1). It should be noted that seven systematic reviews and/or meta-analyses were located relating cannabis use and mental disorders (without specifying whether early cannabis use was involved). Of these publications, the studies included were reviewed to determine whether any of them met the criteria for this paper.
Thus, 15 articles were found that met the inclusion criteria. These were longitudinal articles relating cannabis use in youth to mental disorders, although only five publications made a clear distinction (including specific ages) between early vs. late onset of cannabis use and mental disorders. It should be noted that each of these five studies arbitrarily used a different age criterion to define what was an early or late onset of cannabis use; in other words, age of early onset could vary between 15 and 18 years according to the study in question. The remaining studies analyzed adolescent cohorts, in which they related the onset of cannabis use with the onset of later mental disorders (Table 1). Accordingly, it is not possible to make direct comparisons between the samples in each study, although it is possible to arrive at some conclusions when making these comparisons. Results are given and discussed in the following subsections.
Table 1 Longitudinal studies relating cannabis use in adolescence to mental disorders (psychosis, mood disorders and anxiety); studies that clearly discriminated between early and late onset of cannabis use are indicated

Note: COMT = catechol-O-methyltransferase.
Cannabis use and psychotic disorders
There are several longitudinal studies in general population, together with systematic reviews and meta-analyses of cannabis use and psychotic disorders (Andréasson, Allebeck, Engström, & Rydberg, 1987; Degenhardt & Hall, 2006; Gage, Hickman, & Zammit, 2016; Myles, Myles, & Large, 2016; Moore et al., 2007; Roncero, Collazos, Valero, & Casas, 2007), noting that cannabis use can increase the risk of developing lifetime psychotic disorders and schizophrenia two or threefold (Moore et al., 2007; Hall, 2006).
Specifically, in this correlation, we found 11 longitudinal studies evaluating cannabis use in adolescence together with the presence of psychosis, although only three clearly distinguished between early vs. late onset (Table 1). Since the definition of early onset varied between the studies, Arseneault et al. (2002) defined early onset as use before the age of 15, whereas for Zammit, Owen, Evans, Heron, and Lewis (2011) early onset of cannabis use was defined as beginning at 14. Caspi et al. (2005) described it as beginning before 18. In any case, the risk of psychosis was greater for users who started at an early age (Arseneault et al., 2002; Caspi et al., 2005; Zammit et al., 2011). Thus the lifetime risk of presenting a psychotic disorder increased between 2.5 (Zammit et al., 2011) and four (Arseneault et al., 2002) times compared to those with later onset. The other studies relating cannabis use in adolescence to lifetime presence of psychosis also supported this correlation (Andréasson et al., 1987; Ferdinand et al., 2005; Fergusson, Horwood, & Swain- Campbell, 2003; Fergusson, Boden, & Horwood, 2006; Henquet et al., 2005; Kuepper et al., 2011; Manrique-Garcia et al., 2012; Zammit et al., 2002). These findings have also been observed in retrospective studies (Veen et al., 2004).
On the other hand, some authors point out that starting at an early age not only increases the risk of presenting psychosis, but also makes it emerge at younger ages compared to later users or those who never use cannabis (Hall & Degenhardt, 2007; Helle et al., 2016; Konings, Henquet, Maharajh, Hutchinson, & van Os, 2008; Ksir & Hart, 2016; Veen et al., 2004). In a recent meta-analysis, it points out that regular cannabis use precedes the onset of psychosis by 6.3 years (Myles et al., 2016). Consequently, and predicting that early onset of cannabis use would lead to greater cumulative lifetime exposure to cannabis, some authors have found that the risk clearly increases when the number of lifetime uses of cannabis exceeds 50 (van Os et al., 2002; Zammit et al., 2002). This is consistent with data indicating that dependence would increase the risk of presenting psychotic symptoms (Fergusson et al., 2003). Thus, early onset of cannabis use is a risk due to increased exposure, but also because of the characteristics of the adolescent brain that make it more vulnerable to the effects of cannabis, producing symptoms similar to psychotic ones and possibly psychotic spectrum disorders (Parolaro, 2010). It should also be noted that the age of onset is not the only risk factor, and that, for example, some authors point out that the use of cannabis in high doses is more important (Henquet et al., 2005).
Accordingly, cannabis is possibly not a necessary or sufficient cause, but acts amplifying the genetic vulnerability of the individual with other environmental risk factors, in the development of psychotic disorders (Degenhardt, Hall, & Lynskey, 2003; Ksir & Hart, 2016; van Winkel & Genetic Risk and Outcome of Psychosis Investigators, 2011), or advance the appearance of positive psychotic symptoms by up to three years in these individuals (Helle et al., 2016). A systematic review posits the hypothesis that exposure to cannabis, especially during adolescence, could lead to immunological dysfunctions that could potentially cause latent vulnerability for psychosis and, in turn, increase the risk of schizophrenia (Suárez-Pinilla, López-Gil, & Crespo-Facorro, 2014). It has been postulated that individuals genetically predisposed to suffering from schizophrenia are more likely to use cannabis and to do so in larger amounts. This does not mean that there is no causal relationship between cannabis use and the risk of schizophrenia, but it does establish that at least part of the association may be due to the causal relationship in the opposite direction (Power et al., 2014).
It has therefore been suggested that there is a population genetically vulnerable to developing psychotic symptoms in relation to the use of cannabis (Caspi et al., 2005; De Lisi, 2008), and therefore at a higher risk of developing psychotic disorders. However, not all studies support this theory (Zammit et al., 2011). Cannabis is known to influence various systems of neurotransmitters (Colizzi, McGuire, Pertwee, & Bhattachryya, 2016; Sherif, Radhakrishnan, D’Souza, & Radhakrishnan, 2016), which, through various interactions with the glutamate, dopaminergic, gabaergic, and endocannabinoid system could explain the risk of developing psychotic symptoms (Colizzi et al., 2016; Sherif et al., 2016). Several polymorphisms could be associated, including the Val (158) Met polymorphism in the catechol-O-methyltransferase (COMT) gene, which appears to modulate the association between cannabis use in adolescence and the age of onset of psychotic disorders (Estrada et al., 2011), increasing the risk of developing psychotic disorders in the event of early onset (beginning before age 18) (Caspi et al., 2005). However, not all studies support a relationship between COMT polymorphisms and the risk of psychotic disorders in people who begin using cannabis before the age of 14 (Zammit et al., 2011). One should therefore not overlook the fact that the effects may be partly conditioned by other factors of vulnerability to suffering from psychotic disorders (Henquet et al., 2005).
Lastly, there are other factors that could be associated with cannabis use at early ages and psychosis, such as childhood trauma, and specifically, non-consensual sexual experiences. It has been said that people who have suffered sexual abuse have a six times greater risk of having a psychotic episode than those who have not and if, in addition, the subject uses cannabis, s/he has, in addition, a seven times greater risk of developing a psychotic disorder (Houston, Murphy, Shevlin, & Adamson, 2011; Sideli et al., 2015). However, some longitudinal studies indicate that the relationship between cannabis use and the subsequent presence of psychotic symptoms is unrelated to childhood trauma (Kuepper et al., 2011).
For all these reasons, and even if no definitive conclusions can be drawn about whether cannabis use is directly related to psychosis in adulthood, it seems sensible to inform vulnerable people that cannabis can cause acute psychotic symptoms, especially at high doses.
Cannabis use, mood, and anxiety disorders
Cannabis use is commonly associated with clinical depression, anxiety, and suicide (Alpert, Maddocks, Rosenbaum, & Fava, 1994; Tournier, Sorbara, Gindre, Swendsen, & Verdoux, 2003). Specifically, in this area, we found seven longitudinal studies exploring the relationship between cannabis use and mood disorders and/or anxiety. However only three papers specifically studied the presence of an early onset of cannabis use and the development of mood and anxiety disorders (Arseneault et al., 2002; Fergusson, Horwood, & Swain-Campbell, 2002; Hayatbakhsh et al., 2007), although it must be said that the study by Arseneault et al. (2002) was primarily designed to study psychosis and that the non-correlation between early onset of cannabis and depression observed was a secondary finding. The age set as early onset of cannabis use in the three studies was similar (15 years) (Arseneault et al., 2002; Fergusson et al., 2002; Hayatbakhsh et al., 2007).
Hayatbakhsh et al. (2007) report that patients who began cannabis use before age 15 experienced anxiety and depression more frequently in early adulthood, and that this association is unrelated to personal or family history (Hayatbakhsh et al., 2007). However, this finding was not obtained in two similar studies, which state that the onset of cannabis use before the age of 15 did not predict lifetime depression (Arseneault et al., 2002; Fergusson et al., 2002), although it could predict the presence of suicidal behaviors (Fergusson et al., 2002).
As a result of the above and in comparison with other studies, the results of the various studies differ regarding the most frequent type of relationship between the two pathologies. Longitudinal studies conducted on adults tend to indicate that cannabis use increases the risk of depression (Marmorstein & Iacono, 2011), while cross-sectional studies suggest that a history of depression explains the dysphoria associated with cannabis use (Bovasso, 2001; Moore et al., 2007). Research indicates a slight association between consumption and depression with a probability ratio of 1.4 or more among the most frequent users (without specifying age of onset) (Fernández-Artamendi, Fernández-Hermida, Secades-Villa, & García-Portilla, 2011). It has been pointed out that the relationship between cannabis use and the presence of depressive symptoms is more frequent in women (Patton et al., 2002; Poulin, Hand, Boudreau, & Santor, 2005), and that the earlier and more frequent the use, the higher risk of depression (Hayatbakhsh et al., 2007). However, there is less evidence in this respect than on the association with psychotic disorders (Moore et al., 2007; Kendler, Prescott, Myers, & Neale, 2003). Moreover, the psychosocial consequences of cannabis use partly explain the greater risk of developing a major depressive disorder (Marmorstein & Iacono, 2011).
On the other hand, it should be considered that patients with primary depressive symptoms are at a higher risk of using cannabis (Feingold, Weiser, Rehm, & Lev-Ran, 2015), and could use cannabis to improve their mood (Arendt et al., 2007; Kandel & Chen, 2000; Kandel, Davies, Karus, & Yamaguchi, 1986; Miller-Johnson, Lochman, Coie, Terry, & Hyman, 1998). However, it has also been suggested that the direction of this relationship is inverse, in other words, cannabis use would increase the risk of depression and anxiety, with the decrease in motivation associated with use being a symptom of depression (Bovasso, 2001; Fergusson et al., 2002; Rey & Tennant, 2002). Other authors have pointed out that there would be a common vulnerability conditioned by a genetic base and an unfavorable socio-environmental environment that would facilitate the emergence of the two pathologies in the same individual (Fu et al., 2002; Hall & Degenhardt, 2007). Accordingly, adolescents would have a high prevalence of a history of traumatic parental divorce or abuse in childhood. In these cases, the clinical order would go from the traumatic experience to the presence of depressive symptomatology with a subsequent escalation to substance use (Hayatbakhsh et al., 2007; King, Iacono, & McGue, 2004; Libby, Orton, Stover, & Riggs, 2005).
No longitudinal studies were found specifically exploring the early use of cannabis and the lifetime development of bipolar disorder (BD). A longitudinal study found an association between cannabis use and the risk of presenting BD, although this association disappeared after an adjustment of models (Feingold et al., 2015). Supporting the previous finding, several cross-sectional and retrospective studies relate the use of cannabis to BD (Feingold et al., 2015; van Laar, van Dorsselaer, Monshouwer, & Graaf, 2007), and although there could be many factors involved in the BD-cannabis relationship (van Laar et al., 2007), it is suggested that early onset of cannabis use may be related to an earlier onset of BD (Lagerberg et al., 2011), and that its use is associated with a more severe development of BD (Lagerberg et al., 2016). Cannabis use is an important factor that can trigger an early onset of BD and, by itself, is associated with higher rates of suicidal behavior in BD. However, it is unclear whether or not the effect of cannabis at the age of onset of symptoms and suicide attempts are independent of each other (Leite et al., 2015). On the other hand, patients with BD engage in up to 6.8 times more cannabis use than controls (Agrawal, Nurnberger, Lynskey, & The Bipolar Genome Study, 2011), with adolescents with BD being at a higher risk for the development of the disorder due to substance use (Wilens, 2004).
Lastly, we found a single longitudinal study relating early cannabis use (before the age of fifteen) with the presence of anxiety (Hayatbakhsh et al., 2007). This study is in line with longitudinal studies and meta-analyses that associate the use of cannabis (regardless of age at onset) with anxiety (Moore et al., 2007). However, this relationship between cannabis and anxiety is still controversial, and there are some studies where this association is not found (van Laar et al., 2007).
DISCUSSION AND CONCLUSION
The current review provides data on early cannabis use and the presence of mental disorders. Thus, use at an early age increases the risk of developing mental illnesses in adult life and/or means that they emerge earlier. This association is evident in the case of psychosis yet less clear in mood and anxiety disorders. In any case, due to the risk of developing these psychopathological disorders, it would be sensible to provide suitable psychoeducation and approaches in the presence of a patient with cannabis use disorder, especially if s/he is an adolescent. Cannabis is the most widely used illegal drug worldwide and has historically been regarded as innocuous (Fernandez, Tiffon, Solé, & San, 2003). Its use is frequently banalized by adolescents, and even by their families, forming part of their lifestyle associated with the low perception of the risk involved in its use.
The association between cannabis use and the risk of presenting psychotic symptoms is very well known, although it has not been fully studied at the ages when use could pose the greatest risk. The current review suggests that cannabis use at an early age increases the lifetime risk of suffering psychotic disorders compared with those who begin using it later (Arseneault et al., 2002; Zammit et al., 2011). This risk could be partly be explained by the greater accumulated exposure (van Os et al., 2002; Zammit et al., 2002), genetic factors (Zammit et al., 2002), the increased vulnerability of the developing brain (Parolaro, 2010), alterations in neurotransmission (Colizzi et al., 2016; Sherif et al., 2016), and even immunological alterations (Suárez-Pinilla et al., 2014).
Regarding to mood disorders, there appears to be some association (especially in depression) if there has been an early onset of cannabis use, although current results tend to be contradictory. It is striking that some studies indicate that an early onset could be associated with later suicidal ideation (Fergusson et al., 2002), so the study on how early onset of cannabis use influences the subsequent presence of psychopathology should be prioritized in the field of dual disorders. There is a dearth of specific data on the relationship between anxiety and early onset of cannabis use. Although there would appear to be a relationship, more research is needed in this area to clarify the true relationship between early cannabis use and the future development of anxiety.
The current review has certain limitations, such as the fact that only articles in English and Spanish were reviewed, meaning that articles of great interest in other languages may have been omitted. At the same time, even though the studies were longitudinal, each study had a specific design with characteristics that may not be comparable with each other. Thus, for example, some studies were only performed on men (e.g., Andréasson et al., 1987). Moreover, there were a variety of follow-up times, ranging from 2 to 35 years. Even more importantly, the early onset of cannabis use criterion was arbitrary and there was no set definition.
Moreover, some studies were not specifically designed in keeping with the purpose of the current review, in other words, the findings of some studies were more incidental or associated findings. It is also important to emphasize that some studies failed to take into account the possibility of using other substances and/or polydrug use, which is important because the possibility that cannabis increases the risk of using other substances has been mentioned (Degenhardt et al., 2010; Fergusson, Boden, & Horwood, 2006). It would therefore be useful to continue researching in this area, particularly to define various concepts such as early onset and not only to explore the correlations between early use and psychopathology, but also with associated factors (such as use of other drugs, genetic/family factors, psychosocial factors).
Although age of onset of use is a factor that influences the development of a psychosis, there is less evidence of the association between cannabis and anxiety disorder and mood. It is also important to note that there are other factors that may contribute to the development of mental disorders after an early onset of cannabis use, such as the amount of the substance used and the amount accumulated throughout one’s lifetime. However, given the risk posed by the use of cannabis for adolescent health, this should not be neglected. Treatment schemes should use a multidisciplinary perspective, in order to inform adolescents, and detect its use and the associated consequences. It is possible to conclude that cannabis use is a global problem, and that cannabis use at an early age constitutes a risk factor in the development of certain mental disorders.











 nueva página del texto (beta)
nueva página del texto (beta)