Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Salud mental
versión impresa ISSN 0185-3325
Salud Ment vol.38 no.2 México mar./abr. 2015
Original article
The emotional and behavioral problems of children exposed to poverty and/or collective violence in communities at the Mexico-United States border: A comparative study
Problemas emocionales y de comportamiento entre niños expuestos a la pobreza y/o la violencia colectiva en comunidades en la frontera México-Estados Unidos: Un estudio comparativo
Marie Leiner,1,3 María Theresa Villanos,1 Héctor Puertas,2 Jesús Peinado,1 Carmen Ávila,3 Alok Dwivedi4
1 Department of Pediatrics, Texas Tech University Health Sciences Center, El Paso, Texas.
2 Jurisdicción Sanitaria de la Secretaría de Salud I, Ciudad Juárez, Chihuahua.
3 El Colegio de Chihuahua, Ciudad Juárez, Chihuahua.
4 Division of Biostatistics and Epidemiology. Texas Tech University Health Sciences Center.
Correspondence:
Marie Leiner, PhD.
4800 Alberta El Paso, Texas 79905, USA.
Tel: (915) 215 - 5831.
E-mail: marie.leiner@ttuhsc.edu
Received: April 3, 2014.
Accepted: July 17, 2014.
ABSTRACT
Background
Collective violence attributed to organized crime has shown to be responsible for a considerable burden of physical and mental health morbidity among youth.
Objective
To compare the emotional and behavioral problems of children exposed to early childhood poverty and/or collective violence in communities at the Mexico-United States border to children exposed to other social and health risks.
Method
A cross-sectional study was carried out with individuals living in poverty at two sites at the Mexico-United States border. Individuals who responded once to the Pictorial Child Behavior Checklist (P+CBCL) in Spanish were selected randomly from clinics in a metropolitan area of El Paso, Texas, United States (poverty alone group), and Ciudad Juarez, Chihuahua, Mexico (poverty plus collective violence group). In addition, emotional and behavioral problems present in these groups were compared with available published emotional and behavioral CBCL scales of children exposed to other social and health risks.
Results
Children exposed to both poverty and collective violence had higher emotional and behavioral problem scores as measured by the P+CBCL than those exposed to poverty alone. In addition, compared with children who were brain-injured, hearing impaired, or whose parents were exposed to drugs or alcohol, the poverty and collective violence group had higher levels of emotional and behavioral problems.
Discussion and conclusion
Systematic detection and treatment of children as young as 18 months exposed to trauma are necessary to diminish the mental health problems caused by the collective violence attributed to organized crime.
Key words: Health communication, children, collective violence, mental health, poverty, violence, organized crime.
RESUMEN
Antecedentes
La violencia colectiva atribuida al crimen organizado ha mostrado causar considerables daños en la salud mental de jóvenes.
Objetivo
Comparar los problemas emocionales y de comportamiento de niños expuestos a la pobreza y/o violencia colectiva en comunidades localizadas en la frontera México-Estados Unidos, así como con niños expuestos a otros riesgos.
Método
Estudio transversal con participantes viven en la pobreza en ambos lados de la frontera de México y Estados Unidos. Los participantes respondieron a la versión con pictogramas en español del Cuestionario de Comportamientos de Niños (P+CBCL) en clínicas localizadas en El Paso, Texas (grupo expuesto a la pobreza), y en Ciudad Juárez, Chihuahua, México (grupo expuesto a la pobreza + violencia colectiva). De forma adicional se compararon los problemas emocionales y de comportamiento de estos grupos con resultados históricos obtenidos a partir de la evidencia científica.
Resultados
Los niños expuestos a la pobreza/violencia colectiva registraron resultados más altos en las escalas de problemas emocionales y de comportamiento al medirlos con el P+CBCL cuando se compararon con el grupo expuesto solamente a la pobreza. De forma adicional, al comparar los grupos con niños con problemas cerebrales, de audición, o con padres expuestos a drogas y alcohol, el grupo expuesto a la pobreza y a la violencia registró mayores problemas emocionales y de comportamiento.
Discusión y Conclusión
La detección sistemática y el tratamiento de niños desde los 18 meses expuestos a trauma son necesarios para disminuir los problemas mentales causados por la violencia colectiva atribuida al crimen organizado.
Palabras clave: Comunicación en salud, niños, violencia colectiva, salud mental, pobreza, violencia, crimen organizado.
BACKGROUND
Direct (as victims) and indirect (as witnesses) youth exposure to violence has undoubtedly played a role in creating the conditions for the development of many emotional and behavioral problems.1-4 Individuals facing these types of victimization experience short- and long-term effects that often have an immediate and sustained impact on their lives. Aggression, depression, anxiety, academic failure, isolation, suicide, running away from home, dropping out of high school, and coming into contact with the criminal justice system during adolescence and adulthood are some of the most prevalent outcomes.5-10
A sub-type of direct and indirect violence, known as collective violence, has also been shown to be responsible for a considerable burden of physical and mental health morbidity among youth and adults.11-14 According to the World Health Organization, "collective violence" includes the instrumental use of violence by people that identify themselves as members of a group, which could be transitory or with a more permanent identity, against another group of individuals in order to achieve political, economic, or social gain.15 Most studies regarding children's exposure to collective violence include the psychosocial effects as a result of violence within the community,16-19 war, or guerrilla or military conflicts.20-25 The effects of direct and indirect victimization related to environmental disasters, acts of terror, genocide, or extreme violence have also been studied.26-32
Lately, collective violence attributed to organized crime has received a high degree of public attention in Mexico with intense media coverage. News about mass murders of men, women, and children, including activists and bystanders, mutilations, and numerous acts of terror, including bombings, kidnappings, torture, and decapitations were broadcast and rebroadcast for days or months by media outlets during the most active years of the drug war (2008-2012).33,34 This extraordinary occurrence of stressful events can have a profound effect on children's sense of security, inducing strong feelings of vulnerability and resulting in emotional and psychological trauma, even if these events are only experienced through the media.35-37 The threatening, intrusive images of extreme acts of violence presented by the media include frightening images that are usually very intense, portray actual events with acute suffering, and are often presented unedited.38,39
Second-hand victimization via exposure to these events via the media represents a form of indirect trauma and has been shown to affect children's psychosocial, behavioral, and emotional responses even months to years after the exposure took place.40 Moreover, viewing media footage of geographically remote events led to posttraumatic symptoms in those children who interpreted the footage as threatening to themselves.38
Likewise, poverty has a devastating effect on mental health and is perpetuated through a cycle in which poverty cultivates mental illness, while mental illness reinforces pov-erty.41 Inequalities due to poverty and low socioeconomic status affect different areas of a child's social life, including their access to education and health care, as well as health sta-tus.42 As a result, early detection of emotional and behavioral problems may be impeded due to a reduced opportunity to access early intervention efforts. Mental health services, including detection, referral, and treatment are often described as inadequate in those confronted by poverty. Several communication barriers such as culture, linguistic elements, and literacy levels contribute to these disparities.43-46
Exposure to poverty alone is a risk to the mental health of children,47-49 and poverty with exposure to community violence also has an effect on the mental health of children and adolescents.50,51 However, the possible effect of indirect victimization due to collective violence attributed to organized crime has not been extensively studied due to the difficulty of locating an area where one group has been exposed while the other has not. Most studies describe the generalized effects on all children living in an area without a comparison group. In addition, data obtained by standardized measurements are not available.
In this study, a sample of children living in Ciudad Juarez, Chihuahua, Mexico, exposed to both indirect victimization (collective violence attributed to organized crime) and poverty, were compared with children living in El Paso, Texas, United States, exposed to poverty alone. A standardized instrument, the Pictorial Child Behavioral Checklist (P+CBCL), was used to measure emotional and behavioral problems to compare these two groups. When the study was conducted, Ciudad Juarez was considered one of the most violent cities in the world,33 whereas El Paso had the lowest crime rate in a city with a population of >500 000 residents in the United States.52 The number of drug-related killings in the two cities in 2010 was as follows: Ciudad Juarez, 2101 organized crime homicides,53 and El Paso, 0 per 100 000 people.
METHOD
Type of study
This is a cross-sectional study with data collected in 2010 in two border cities in the United States and Mexico.
Participants
A total of 632 participants was randomly included in this study: 316 from El Paso, Texas, United States, and 316 from Ciudad Juarez, Chihuahua, Mexico. Participant information was extracted from electronic records databases maintained during the same period in six university-based clinics in El Paso and nine clinics of the Secretaria de Salud in Mexico.
Database information characteristics
United States electronic information: A large electronic database containing approximately 3000 pediatric patients 18 months to 5 years old whose parents responded to a psychosocial and behavioral assessment known as the Pictorial Child Behavior Checklist (P+CBCL) during non-emergency visits.
Mexican electronic information: Parents/caretakers of children 18 months to 5 years of age responded to the selfresponse P+CBCL during non-emergency visits, when the children were receiving regular care in these clinics.
Information available in the two databases included date of assessment, gender, age, and total scores of the P+CBCL.
Inclusion criteria
The clinics in El Paso and Ciudad Juarez served mainly low-income Hispanic children. Only children of parents who reported Hispanic ethnicity responded to the P+CBCL questionnaire in Spanish, and those who had a family income below the poverty level were sampled in the United States. The United States site excluded <5% of the patients, with approximately 79% of families enrolled in Medicaid, 16% in the State Children's Health Insurance Program, and 5% without insurance. At the Mexico site, all children were covered by ''Seguro Popular", an insurance program provided by the government to those with the lowest income.54 Electronic data from the Mexico clinics containing records without identifiers were provided for analysis with authorization from the Secretaria de Salud-Jurisdiccion Sanitaria II ethics committee. The study was also approved by the Institutional Review Board at Texas Tech University Health Sciences Center.
Measurements
The P+CBCL is an adaptation of the original 18 months to 5 years of age CBCL,55 which was developed56 to support parents with limited literacy. The P+CBCL for ages 1.5 to 5 years is a well-validated questionnaire including items to determine the frequency of behavioral and psychosocial problems in young children. Both externalizing (attention deficit and aggressive behavior) and internalizing (withdrawn, somatic complaints, anxious and depressed, and emotionally reactive) syndromes are obtained as a result of the responses of the parents to the questionnaire. The P+CBCL has been validated with Mexican children.57-59 Additionally, it has demonstrated remarkable consistency in its psychometric properties across more than 30 countries.60 For this study, we used society Group 1 for children in the United States and Group 3 for children in Mexico.61
Different norms are established for children when raw scores from the P+CBCL are converted to T scores. A T score <60 is "normal", and a T score ≥64 is 'abnormal". This suggested cut-off point dichotomized ' normal" and ' clinical" groups and is able to discriminate between nonreferred and referred children for mental health services.
Additionally, the emotional and behavioral scales obtained for each group were compared with available evidence for children exposed to traumatic conditions or social and health risks.
The data from the El Paso site represent the poverty exposure group while data from the Ciudad Juarez site represent the poverty and violence exposure group. We refer to this exposure variable as a group (United States and Mexico) variable in the study.
Statistical methods
Continuous variables were described using mean and standard deviation (SD), while categorical variables were described using frequency and proportion. The prevalence of behavioral and psychosocial problems obtained using the P+CBCL was also determined and reported. Continuous variables were compared using an unpaired t-test according to the group, while categorical variables were compared using Fisher's exact test. The various scores obtained from the P+CBCL for different components of behavioral and psychosocial problems were compared between groups using an unpaired t-test. The overall group effect was examined using multivariate linear regression analysis after adjusting for gender and age followed by multiple linear regression analyses for each of the outcome scores, separately after adjusting for multiple outcome comparisons. The group effect on each score was presented using adjusted regression coefficient (ARC) with their 95% confidence interval (CI). The scores were non-normally distributed; thus the above analyses were carried out on log transformed scores. Results were consistent; therefore, we only reported results for untransformed scores. All the statistical analyses were performed using SAS 9.3.
RESULTS
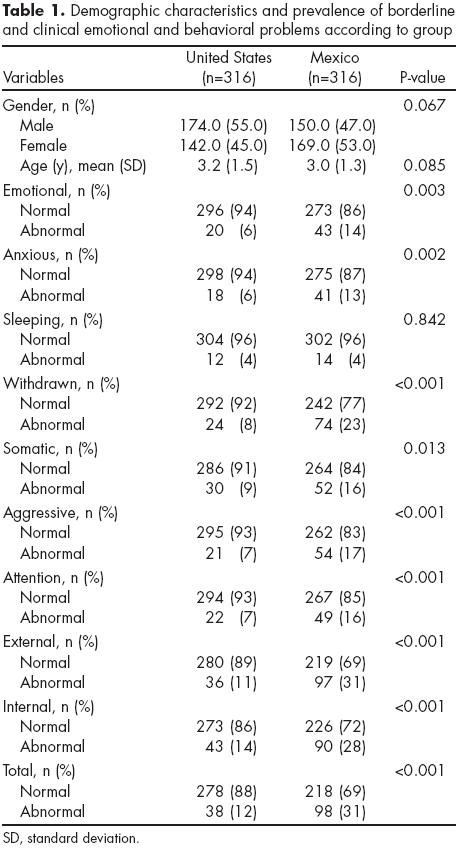
The demographic profile and prevalence of psychosocial and behavioral problems according to groups is presented in table 1. There were no apparent differences regarding age and gender between the two groups. The prevalence of borderline and clinical external and internal problems was higher in the Mexico group, but there were statistical differences for all emotional/behavioral problems reported, with the exception of sleeping problems.
Raw P+CBCL scores among the two groups indicate that the Mexico group had higher scores in all problem scales (table 2). When comparing the unadjusted mean raw scores between the United States and Mexico, there were significant differences in all scales, with higher scores reported in Mexico.

Multivariate regression analysis revealed that the overall Mexico group had higher scores as compared with the United States group after adjusting for gender and age (table 3). Individual scores analyses also demonstrated significant effects of group of the problem scales (emotionally reactive, anxious and depressed, somatic complaints, withdrawn, sleep problems, attention problems, and aggressive behavior).

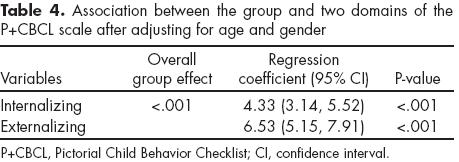
In addition, significant effects of the group were found in the total scales (internalizing and externalizing problems scales), with higher scores in the Mexico group (table 4). There were significant effects in all the Diagnostic and Statistical Manual of Mental Disorders (DSM) scales, including DSM affective, DSM anxiety, DSM pervasive, DSM attention-deficit/hyperactivity disorder (ADHD), and DSM oppositional defiant, with higher scores in the Mexico group (table 5). Age was significantly associated with sleep problems, attention problems, and aggressive behavior, while gender was associated with attention and aggressive behavior problems. These scores significantly decreased per unit increase in age. Females had significantly lower scores of aggressive behavior and external problems compared to males. Increase in age significantly reduced the external scores in multiple linear regression analysis, and in the DSM scale, age was only associated with ADHD problems, whereas gender was significantly associated with both pervasive problems and ADHD.

The compiled T scores of children confronting health risks measured using the CBCL scale from several available studies are presented in table 6. Comparison of these available results with the United States and Mexico groups indicates that the Mexico group had equal or higher T scores for most of the scales, with few exceptions (e.g., sleep problems). When compared to children with mild/severe brain injury,62 single-suture craniosynostosis,63 parental history of cocaine, alcohol, tobacco, and marijuana exposure,64 prenatal cocaine exposure,65 maternal current and past depression,66 and hearing impairment,67 children in the Mexico group had significantly higher scores for most scales. A smaller number of scales were similar and non-significant when compared with the Mexico group, with a reduced number of higher scales and significant differences in the same group. There were also significantly higher scores in the United States group for some scales, including emotional reactive, anxious depressed, and somatic problems.
DISCUSSION AND CONCLUSION
Crime victimization has been shown to be a major and public problem that increases the risks to victims of suffering from trauma-related disorders, including PTSD, suicide, substance abuse, future criminal behavior, health and social problems, and future poly-victimization.68 It has been found that trauma history, including direct victimization, is often not evaluated or treated appropriately. This implies that victims of indirect victimization have even less opportunity for rehabilitation or support services. In addition, studies of the effects of crime victimization, which is considered direct exposure to violence, generally focus on adults, leaving an important gap in the effects of indirect victimization on children.69 Some studies have found that indirect victimization does not predict aggressive behaviors,70 and others indicate systematically that aggression is present at short or long term.71-73
There are also key gaps in mental health research related to children from birth to age 5 years, particularly low-income children.74 Here, we presented the emotional and behavioral problems confronted by children living in poverty in two different geographic areas at the Mexico-United States border. Children at the Mexican site, in addition to poverty, were subject to collective violence attributed to organized crime and reported higher emotional and behavioral scores than those at the United States site. When compared with other children of the same ages exposed to social and health risks, most of the Mexico group scores surpassed the internalizing or/and externalizing scales. In a previous study examining the same exposure and groups, except with individuals 6-16 years of age, we found that the Mexico site externalizing scale scores were higher than the United States site scores.75 However, in the present study, emotional and behavioral scales scores were higher in the Mexico group than those in the United States site and also than those in the historical data groups. While poverty was shown to be a risk factor for emotional and behavioral problems for both groups, collective violence exposure may be the cause for the higher risk among the Mexico group.
The amount of published research about the effects of exposure to collective violence is minimal and lacking in longitudinal studies that would allow drawing firm conclusions. This study has limitations, including its retrospective, rather than prospective, character. In addition, due to the nature, frequency, and dissemination of news about the generalized violence in the city, for this study it was assumed that families were indirectly victimized, and specific questions regarding possible individual victimization were not posed.
These questions were not included due to the inability of the researchers to provide specific health care services to the families. This was considered ethical practice despite the possibility of confounding the results. Another limitation includes the possibility that poverty exposure could differ between Mexico and the United States, resulting in different adversity. Many families victimized in Ciudad Juarez had moved to El Paso seeking safety, and there is a remote possibility that these individuals were included in the United States group. Despite these limitations, this study allowed us to compare data using a well-recognized screening assessment with demonstrated consistency in more than 30 countries.60 In addition, in an attempt to compare similar populations, data collection included the same time periods in the United States and Mexico with equivalent poverty levels and the largest possible sample size.
Responses of children to indirect exposure to collective violence are determined by individual level risks factors that include socioeconomic status, family context (including parental distress), appropriate child care, personal characteristics, and the severity and amount of exposure.76 This article provides information indicating that behavioral problems are displayed with higher frequency among children exposed to poverty and collective violence when compared to children exposed only to poverty. Supportive parenting practices have been found to moderate the risks of exposure to collective violence caused by military conflicts and aggression.77 In addition, detection and treatment can have an important impact on the outcome.78 Effective systematic detection and treatment of children as young as 18 months exposed to trauma are necessary to diminish the mental health problems caused by the collective violence attributed to organized crime.
Funding
None.
Conflict of Interest
No author of this paper has a conflict of interest, including specific financial interests, relationships, and/or affiliations relevant to the subject matter included in this manuscript.
Acknowledgements
Special thanks to doctor Laura Carrillo for her contribution in finding available articles related to emotional and social risks.
References
1. Gilbert R et al. Burden and consequences of child maltreatment in high-income countries. Lancet 2009;373(9657):68-81. [ Links ]
2. Turner HA et al. Family context, victimization, and child trauma symptoms: variations in safe, stable, and nurturing relationships during early and middle childhood. Am J Orthopsychiatry 2012; 82(2):209-219. [ Links ]
3. Turner HA et al. Disability and victimization in a national sample of children and youth. Child Maltreat 2011;16(4):275-286. [ Links ]
4. Finkelhor D, Ormrod RK, Turner HA. Lifetime assessment of polyvictimization in a national sample of children and youth. Child Abuse Negl 2009;33(7):403-411. [ Links ]
5. Cuevas CA et al. Psychological distress as a risk factor for re-victimization in children. Child Abuse Negl 2010;34(4):235-243. [ Links ]
6. Turner HA, Finkelhor D, Ormrod R. The effects of adolescent victimization on self-concept and depressive symptoms. Child Maltreat 2010;15(1):76-90. [ Links ]
7. Turner HA, Finkelhor D, Ormrod R. Child mental health problems as risk factors for victimization. Child Maltreat 2010; 15(2):132-143. [ Links ]
8. Cuevas CA et al. Psychiatric diagnosis as a risk marker for victimization in a national sample of children. J Interpers Violence 2009;24(4):636-652. [ Links ]
9. Turner HA, Finkelhor D, Ormrod R. The effect of lifetime victimization on the mental health of children and adolescents. Soc Sci Med 2006;62(1):13-27. [ Links ]
10. Haynie DL et al. Exposure to violence in adolescence and precocious role exits. J Youth Adolesc 2009;38(3):269-286. [ Links ]
11. Turner HA et al. Recent victimization exposure and suicidal ideation in adolescents. Arch Pediatr Adolesc Med 2012. Published Online: p. 1-6. [ Links ]
12. Turner HA, Finkelhor D. Ormrod R. Family structure variations in patterns and predictors of child victimization. Am J Orthopsychiatry 2007;77(2):282-295. [ Links ]
13. Elbedour S et al. The scope of sexual, physical, and psychological abuse in a Bedouin-Arab community of female adolescents: The interplay of racism, urbanization, polygamy, family honor, and the social marginalization of women. Child Abuse Negl 2006;30(3):215-229. [ Links ]
14. Boney-McCoy S, Finkelhor D. Prior victimization: a risk factor for child sexual abuse and for PTSD-related symptomatology among sexually abused youth. Child Abuse Negl 1995;19(12):1401-421. [ Links ]
15. Global consultation on violence and health violence: a public health priority 1996, WHO Geneva. [ Links ]
16. Kelly SE, Anderson DG. Adolescents, gangs, and perceptions of safety, parental engagement, and peer pressure. J Psychosoc Nurs Ment Health Serv 2012;50(10):20-28. [ Links ]
17. Sareen J et al. Adverse childhood experiences in relation to mood and anxiety disorders in a population-based sample of active military personnel. Psychol Med 2013;43(1):73-84. [ Links ]
18. Fuller-Thomson E, Baker TM, Brennenstuhl S. Evidence supporting an independent association between childhood physical abuse and lifetime suicidal ideation. Suicide Life Threat Behav 2012;42(3):279-291. [ Links ]
19. Liu J, Chen X, Lewis G. Childhood internalizing behaviour: analysis and implications. J Psychiatr Ment Health Nurs 2011;18(10):884-894. [ Links ]
20. Harder VS et al. Multiple traumas, postelection violence, and posttraumatic stress among impoverished Kenyan youth. J Trauma Stress 2012;25(1):64-70. [ Links ]
21. Friedman-Peleg K, Goodman YC. From posttrauma intervention to immunization of the social body: pragmatics and politics of a resilience program in Israel's periphery. Cult Med Psychiatry 2010;34(3):421-442. [ Links ]
22. Betancourt TS et al. Sierra Leone's former child soldiers: a longitudinal study of risk, protective factors, and mental health. J Am Acad Child Adolesc Psychiatry 2010;49(6):606-615. [ Links ]
23. Panter-Brick C et al. Violence, suffering, and mental health in Afghanistan: a school-based survey. Lancet 2009;374(9692):807-816. [ Links ]
24. De Haene, Grietens LH, Verschueren K. Adult attachment in the context of refugee traumatisation: the impact of organized violence and forced separation on parental states of mind regarding attachment. Attach Hum Dev 2010;12(3):249-264. [ Links ]
25. Warf C, Eisenstein E, Stahl C. Children, adolescents, and war: the systematic engagement of youth in collective violence. Adolesc Med State Art Rev 2009;20(3):961-80, xi. [ Links ]
26. Garrett AL et al. Children and megadisasters: lessons learned in the new millennium. Adv Pediatr 2007;54:189-214. [ Links ]
27. Saraiya A, Garakani A. Billick S.B. Mental health approaches to child victims of acts of terrorism. Psychiatr Q 2013;84(1):115-124. [ Links ]
28. Perlman SE et al. Short-term and medium-term health effects of 9/11. Lancet 2011;378(9794):925-934. [ Links ]
29. Jordan HT et al. Mortality among survivors of the Sept 11, 2001, World Trade Center disaster: results from the World Trade Center Health Registry cohort. Lancet 2011;378(9794):879-887. [ Links ]
30. Gershoff ET et al. Exposure to 9/11 among youth and their mothers in New York City: enduring associations with mental health and sociopolitical attitudes. Child Dev 2010;81(4):1142-1160. [ Links ]
31. Pandya A et al. Services provided by volunteer psychiatrists after 9/11 at the New York City family assistance center: September 12-Novem-ber 20, 2001. J Psychiatr Pract 2010;16(3):193-199. [ Links ]
32. Mijanovich T, Weitzman BC. Disaster in context: the effects of 9/11 on youth distant from the attacks. Community Ment Health J 2010;46(6):601-611. [ Links ]
33. Hernandez AA, Grineski SE. Disrupted by violence: children's wellbeing and families' economic, social, and cultural capital in Ciudad Juarez, Mexico. Rev Panam Salud Publica 2012;31(5): 373-379. [ Links ]
34. Gutierrez LA et al. Using evidence on violence and injury prevention for policy development and decision making in Ciudad Juarez, Mexico. Rev Panam Salud Publica 2012;31(5):365-372. [ Links ]
35. Ahern J et al. Television images and psychological symptoms after the September 11 terrorist attacks. Psychiatry 2002;65(4):289-300. [ Links ]
36. Fairbrother G et al. Posttraumatic stress reactions in New York City children after the September 11, 2001, terrorist attacks. Ambul Pediatr 2003;3(6):304-411. [ Links ]
37. Otto MW et al. Posttraumatic stress disorder symptoms following media exposure to tragic events: impact of 9/11 on children at risk for anxiety disorders. J Anxiety Disord 2007;21(7):888-902. [ Links ]
38. Pfefferbaum B et al. Television exposure in children after a terrorist incident. Psychiatry 2001;64(3):202-211. [ Links ]
39. Pfefferbaum B. The impact of the Oklahoma City bombing on children in the community. Mil Med 2001;166(12 Suppl):49-50. [ Links ]
40. Holmes EA, Creswell C, O'Connor TG. Posttraumatic stress symptoms in London school children following September 11, 2001: an exploratory investigation of peri-traumatic reactions and intrusive imagery. J Behav Ther Exp Psychiatry 2007;38(4):474-490. [ Links ]
41. Anakwenze U, Zuberi D. Mental health and poverty in the inner city. Health Soc Work 2013;38(3):147-157. [ Links ]
42. Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med 2013;90:24-31. [ Links ]
43. Baker DW et al. Health literacy and performance on the Mini-Mental State Examination. Aging Ment Health 2002;6(1):22-29. [ Links ]
44. Baker DW et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health 2002;92(8):1278-1283. [ Links ]
45. Leiner M et al. The Pictorial Child Behavior Checklist: An assessment tool for parents with low literacy levels. Baltimore, MD: Pediatric Academy Societies; 2009. [ Links ]
46. Leyva M, Sharif I, Ozuah PO. Health literacy among Spanish-speaking Latino parents with limited English proficiency. Ambul Pediatr 2005;5(1):56-59. [ Links ]
47. Hurd NM, Stoddard SA, Zimmerman MA. Neighborhoods, social support, and african american adolescents' mental health outcomes: a multilevel path analysis. Child Dev 2013;84(3):858-874. [ Links ]
48. Marie-Mitchell A, O'Connor TG. Adverse childhood experiences: translating knowledge into identification of children at risk for poor outcomes. Acad Pediatr 2013;13(1):14-19. [ Links ]
49. Pearce A, Lewis H, Law C. The role of poverty in explaining health variations in 7-year-old children from different family structures: findings from the UK Millennium Cohort Study. J Epidemiol Community Health 2013;67(2):181-189. [ Links ]
50. Finkelhor D, Ormrod RK, Turner HA. Re-victimization patterns in a national longitudinal sample of children and youth. Child Abuse Negl 2007;31(5):479-502. [ Links ]
51. Finkelhor D, Ormrod RK, Turner HA. Poly-victimization: a neglected component in child victimization. Child Abuse Negl 2007;31(1):7-26. [ Links ]
52. Morgan KOL, Morgan S, Boba R. City Crime Rankings 2011-2012. Florida: Florida Atlantic University; 2011; p. 408. [ Links ]
53. Molzahn C, Ríos V, Shirk DA. Drug violence in Mexico: Data and analysis through 2011, in trans-border Institute-Joan B. Kroc School of Peace Studies. San Diego, Ca: University of San Diego; 2012. [ Links ]
54. King G et al. Politically Robust' Experimental Design for Public Policy Evaluation, with Application to the Mexican Universal Health Insurance Program. J Policy Analysis Management 2007;26(3):479-506. [ Links ]
55. Achenbach TM, Rescorla LA. Manual for the ASEBA preschool and school-age forms and profiles. Burlington, VT: University of Vermont, Department of Psychiatry; 2001. [ Links ]
56. Leiner M et al. Psychometric comparisons of the Pictorial Child Behavior Checklist with the standard version of the instrument. Psychol Assess 2010;22(3):618-627. [ Links ]
57. Albores-Gallo L et al. Validity and reability of the CBCL/6-18. Includes DSM scales. Actas Esp Psiquiatr 2007;35(6):393-399. [ Links ]
58. Albores-Gallo L et al. Bullying and its association with psychiatric disorders in a Mexican students sample. Salud Publica Mex 2010;53(3):220-227. [ Links ]
59. Leiner MA et al. Screening Mexicans for psychosocial and behavioral problems during pediatric consultation. Rev Invest Clin 2007;59(2): 116-123. [ Links ]
60. Ivanova MY et al. Testing the 8-syndrome structure of the child behavior checklist in 30 societies. J Clin Child Adolesc Psychol 2007;36(3): 405-417. [ Links ]
61. Rescorla LA et al. International comparisons of behavioral and emotional problems in preschool children: parents' reports from 24 societies. J Clin Child Adolesc Psychol 2011;40(3):456-467. [ Links ]
62. Wetherington CE et al. Parent ratings of behavioral functioning after traumatic brain injury in very young children. J Pediatr Psychol 2010;35(6):662-671. [ Links ]
63. Kapp-Simon KA et al. Behavioral adjustment of toddler and preschool-aged children with single-suture craniosynostosis. Plast Reconstr Surg 2012;130(3):635-647. [ Links ]
64. Accornero VH et al. Behavioral outcome of preschoolers exposed prenatally to cocaine: role of maternal behavioral health. J Pediatr Psychol 2002;27(3):259-269. [ Links ]
65. Lindhiem O, Dozier M. Caregiver commitment to foster children: the role of child behavior. Child Abuse Negl 2007;31(4):361-374. [ Links ]
66. Dietz LJ et al. Maternal depression, paternal psychopathology, and toddlers' behavior problems. J Clin Child Adolesc Psychol 2009;38(1):48-61. [ Links ]
67. Barker DH et al. Predicting behavior problems in deaf and hearing children: the influences of language, attention, and parent-child communication. Dev Psychopathol 2009;21(2):373-392. [ Links ]
68. O'Brien KM. Advancing mental health services and research for victims of crime. J Trauma Stress 2010;23(2):179-181. [ Links ]
69. McCart MR, Smith DW, Sawyer GK. Help seeking among victims of crime: a review of the empirical literature. J Trauma Stress 2010;23(2):198-206. [ Links ]
70. Orue I, Calvete E. [Justification of violence as a mediator between exposure to violence and aggressive behavior in children]. Psicothema 2012;24(1):42-47. [ Links ]
71. Siyahhan S, Aricak OT, Cayirdag-Acar N. The relation between bullying, victimization, and adolescents' level of hopelessness. J Adolesc 2012;35(4):1053-1059. [ Links ]
72. Arnocky S, Vaillancourt T. A multi-informant longitudinal study on the relationship between aggression, peer victimization, and dating status in adolescence. Evol Psychol 2012;10(2):253-270. [ Links ]
73. Poteat VP et al. The effects of general and homophobic victimization on adolescents' psychosocial and educational concerns: the importance of intersecting identities and parent support. J Couns Psychol 2011;58(4):597-609. [ Links ]
74. Fantuzzo J, McWayne C, Bulotsky R. Forging strategic partnerships to advance mental health science and practice for vulnerable children. School Psychology Review 2003;32(1):31-37. [ Links ]
75. Leiner M et al. Children's mental health and collective violence: a binational study on the United States-Mexico border. Rev Panam Salud Publica 2012;31(5):411-416. [ Links ]
76. Friedman MJ et al. Fighting the psychological war on terrorism. Psychiatry 2004;67(2):123-136. [ Links ]
77. Qouta S et al. Does war beget child aggression? Military violence, gender, age and aggressive behavior in two Palestinian samples. Aggress Behav 2008;34(3):231-244. [ Links ]
78. Weingarten K. Witnessing the effects of political violence in families: mechanisms of intergenerational transmission and clinical interventions. J Marital Fam Ther 2004;30(1):45-59. [ Links ]














