Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Salud mental
Print version ISSN 0185-3325
Salud Ment vol.37 n.2 México Mar./Apr. 2014
Artículo original
Thyroid status in lithium-treated bipolar disorder patients: An one-year follow-up study
Estudio de un año de seguimiento del estado de la tiroides en pacientes con trastorno bipolar tratados con litio
Gülsüm Cantürk,1 Nurhan Fistikci,1 Omer Saatcioglu,1 Evrim Erten,1 Seda Öner,1 Nurten Turan2
1 Bakirkoy Research and Training Hospital for Psychiatry, Neurology and Neurosurgery. Istambul, Turkey.
2 Bakirkoy Dr. Sadi Konuk Research and Training Hospital. Istambul, Turkey.
Correspondence:
Nurhan Fistikci.
Bakirköy Prof. Dr. Mazhar Osman Ruh Sağliği ve Sinir Hastaliklari
E.A. Hastanesi 34147 Bakirköy/Istanbul
Gsm: + 90 533 526 13 66.
Fax: +90 212 409 15 95.
E-mail: nurhanfistikci@gmail.com
Recibido: 4 de agosto de 2013.
Aceptado: 10 de enero de 2014.
ABSTRACT
Objective
In this follow-up study, the hormonal changes were determined in bipolar euthyroid patients who were treated with lithium for the duration of one year.
Method
For the study, 23 bipolar I disorder patients without any axis I co-morbidity were consecutively selected and followed up for one year. All patients were compared with 25 age- and sex-matched healthy controls in terms of thyroid hormone levels and thyroid volumes. The Sociodemographic and Clinical Characteristics Data Form, Hamilton Depression Rating Scale (HAM-D), Young Mania Rating Scale (YMRS), Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I and SCID-I/NP) were administered. Initial thyroid hormone levels and thyroid volumes were measured in the patients and controls. Patient and control groups were compared at baseline for thyroid volumes. Patients' lithium levels were measured at baseline, they were re-examined at six months for thyroid hormones, and at the first year for thyroid hormones and lithium levels.
Results
Thyroid hormone levels changed in no patients during the follow-up period. Thyroid hormone levels were measured within the normal range. No correlation was found between the final TSH levels and duration of illness, duration of lithium treatment, initial thyroid volumes, and the initial TSH levels.
Conclusions
Lithium can safely be used in bipolar patients who were already receiving this treatment before and not developed any thyroid problem for a substantial period.
Key words: Lithium, thyroid gland, bipolar disorder.
RESUMEN
Objetivo
En este estudio de seguimiento se determinarán los cambios hormonales que se producen en pacientes eutiroideos con trastorno bipolar en tratamiento con litio durante un periodo de un año.
Método
Para el estudio se seleccionaron de forma consecutiva 23 pacientes con trastorno bipolar tipo I sin prevalencia concomitante de otros trastornos del eje I, y fueron seguidos durante un año. En todos los pacientes se compararon los niveles de las hormonas tiroideas y el volumen de la glándula tiroides con las del grupo control sano pareado por sexo y compuesto de sujetos de 25 años de edad. La evaluación se hizo por medio de: una hoja de datos de las características sociodemográficas y clínicas, la Escala de Valoración de Hamilton para la Evaluación de la Depresión (HDRS), la Escala de Young para la Evaluación de la Manía (YMRS), Entrevistas clínicas estructuradas para los trastornos del eje I del DSM-IV (SCID-I y SCID-I/NP). A los pacientes y al grupo control se les midieron los niveles iniciales de las hormonas tiroideas y el volumen de la glándula tiroides, a la vez que se les comparó la línea base del volumen de la glándula tiroides. Al inicio del estudio se determinó la línea base de los niveles de litio en los pacientes. Al sexto mes, se reexaminaron las hormonas tiroideas y, al cabo del primer año, los niveles hormonales tiroideos y de litio.
Resultados
Los niveles de las hormonas tiroideas no sufrieron cambios en ningún paciente durante todo el seguimiento. Dichos niveles se midieron dentro de los intervalos normales. No se detectó ninguna correlación entre los niveles de TSH y la duración de la enfermedad, ni con la duración del tratamiento con litio, ni entre los volúmenes iniciales de las glándulas tiroideas con los niveles iniciales de TSH.
Conclusión
El litio puede administrarse con seguridad en pacientes bipolares que se hayan sometido antes a este tratamiento, y a los cuales no les produzca problemas tiroideos durante un periodo significativo de tiempo.
Palabras clave: Litio, glándula tiroides, trastorno bipolar.
INTRODUCTION
Lithium was shown to affect thyroid functions in cell cultures, experimental animals and studies conducted with volunteers and patients.1 Benign, diffuse, non-toxic goiter is reported in ratios varying between 3.8-51%.2-8 While goiter may develop after a couple of weeks of lithium use, it may also develop after long years.9,10 Thyroid functions are within normal ranges in most of the patients receiving lithium therapy. Its effect on thyroid functions is within a large spectrum varying between asymptomatic conditions which can only be detected with laboratory tests and hypothyroidism.11-14 Although lithium is reported to lead to subclinical or clinical hypothyroidism, rare cases with hyperthyroidism and even thyrotoxicosis have also been reported in literature.15,16
In the study of Özsoy et al.,17 comparing lithium-naive and lithium-treated bipolar patients and healthy controls, they reported that volume increase and thyroid hormone changes were more common in lithium-treated group and recommended thyroid ultrasonography before starting lithium therapy and on follow-up of patients. It is recommended to measure free T3, T4,TSH and thyroid volumes at the beginning of therapy and re-examine them at every six months.18-21 Similarly, Bauer et al. reported that palpation is not sufficient for detection of goiter and thyroid ultrasonography must be obtained before therapy and on follow-up.22 It is also recommended to monitor thyroid volume changes with thyroid ultrasonography when goiter is detected during lithium therapy.23
In this study, lithium-treated euthyroid patients with bipolar disorder were followed up for one year and lithium and hormone levels were recorded. It was detected whether patients developed thyroid disorders or hormonal changes in one year of follow-up period.
METHOD
Participants
Twenty-three patients who were being followed up with diagnosis of type I bipolar disorder according to DSM-IV diagnostic criteria were consecutively enrolled in the study. Control group consisted of 25 subjects who met the criteria of the study. Bipolar patients who were euthymic for at least eight weeks (YMRS<5, HAM-D<7), whose two lithium levels measured within the recent six months were normal (0.6-1.2 meq/l) were included in the study. Five out of 30 patients and six out of 31 controls were excluded from the study as they were detected to have a thyroid nodule on thyroid ultrasonography.
Patients were included if they had baseline free thyroxine (fT4), free triiodothyronine (fT3), and Thyroid-stimulating hormone (TSH) values at normal limits (TSH: 0.35 - 4.94 uIU/ml; fT3: 1.71 - 3.71 pgr/mL; fT4: 0.70 - 1.48 ng/dL). Patients who had educational or lingual problems interfering with diagnostic psychiatric interview, who had any neurodegenerative diseases, dementia, mental retardation, seizures, cerebral tumor or cerebrovascular diseases, head trauma leading to unconsciousness, endocrino-logic diseases, any concurrent axis I diagnosis, diagnosis of alcohol and/or substance addiction, who had contraindications for ultrasonography (a significant wound scar or tissue defect interfering with or limiting mild extension of the neck and acoustic permeability), pregnancy, abnormal fT3, fT4, TSH values, thyroid nodule, mass or abnormal vascularization on ultrasonography were excluded from the study.
Control group consisted of individuals aged between 18-65 years, who had normal fT3, fT4, TSH values, who had the similar criteria with patient group.
Thyroid function tests (fT3, fT4, TSH) of patient and control groups were examined in the same laboratory and subjects who had normal values were included in the study. Presence of axis I disorders or whether there was an additional diagnosis or was not determined using SCID-I prepared for patients and healthy controls. fT3, fT4, TSH, thyroid volumes and lithium levels were measured at the beginning of the study. Thyroid hormone levels and thyroid volumes of patient and control groups were compared at the beginning of the study. fT3, fT4, TSH, lithium levels were re-examined at six months and one year. Ethics committee approval was obtained and written informed consent was obtained from the participants.
Measurements
Scales
Sociodemographic and Clinical Characteristics Data Form: This semi-structured form prepared by the researchers considering study characteristics and inquiring sociodemo-graphic and clinical characteristics included gender, age, marital status, educational status, occupational status, level of income, age of bipolar disorder onset, drug use, family history of psychiatric diseases.
Hamilton Depression Rating Scale (HAM-D) is a scale developed by Hamilton in order to evaluate depression severity in patients diagnosed with depression and filled out by the reviewer. Its Turkish reliability and validity study was done by Akdemir et al.24
Young Mania Rating Scale (YMRS) is a scale developed by Young et al. in 1978 in order to measure severity and alteration of manic condition and is filled out by the reviewer. It consists of a total of 11 items. Its validity and reliability study was done by Karadağ et al. in our country.25
• Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I and SCID-I/NP):
- SCID-I: A structured interview developed to facilitate DSM-IV axis I diagnoses.26 The Turkish reliability and validity study was conducted by Çorapçioğlu et al.27
- SCID-I/NP: A semi-structured clinical interview tool developed to exclude DSM-III-R diagnoses.28 The Turkish adaptation was conducted by Sorias et al.29
• Thyroid ultrasonography: Thyroid ultrasonography of the subjects was done by the same radiologist using VFX 9-4 multi-D matrix probe of Siemens Acuson Antares (Siemens, USA) device. Central frequency was adjusted as 7 mHz in the probe of which frequency interval is 4-9 mHz and transverse and antero-posterior length on axial plane and cranio-caudal length on sagittal plane were measured with an electronic ruler.
Statistical analysis
Statistical analysis of the study was done using SPSS 14.0 package program. Descriptive methods (frequency, median, standard deviation) were used for statistical evaluation of data and cui-square test was used for assessment of associations between categorical variables. Mann Whitney U test was used for comparison of non-parametric measurements, Friedman test was used for significance level of change of repeated measurements and Spearman's correlation analysis was used for analysis of factors which could affect TSH value at the end of one year of follow up.
RESULTS
Patients with bipolar disorder who had been euthymic for at least eight weeks and whose at least two plasma lithium levels were found within normal ranges (0.6-1.2 mEq/L) during recent six months were included in the study. Five out of 28 patients were excluded from the study as thyroid nodule was detected on thyroid ultrasonography.
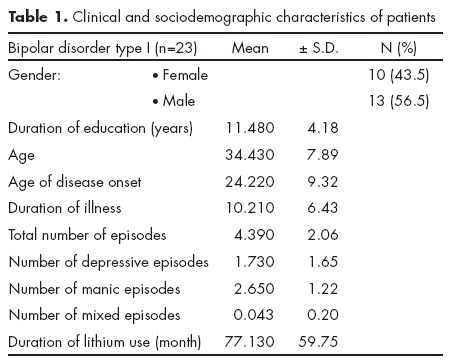
Of the patients, 10 (43.5%) were female and 13 (56.5%) were male and mean age was 34.43 ± 7.89 years. Mean duration of education was 11.48 ± 4.18 years. Of control group, 11 (44%) were female and 14 (56%) were male. A significant difference was not detected between groups in terms of gender distribution (χ2=0.01; p=0.60). Mean age of control group was 33.6 ± 6.69 years. A statistically significant difference was not detected between groups in terms of mean age (z=-0.50; p=0.61). Patients had been using lithium for average 77.13 ± 59.75 months. Clinical and sociodemographic characteristics of patients are shown in table 1.
Of the patients, 30.4% (n=7) were using only lithium, 56.5% (n=13) were using antipsychotics in addition to lithium, 13% (n=3) were using the combination of lithium, anti-psychotics and antidepressants.
Mean TSH level of bipolar patients was 2.10 ± 0.98 and mean TSH level of control group was 1.83 ± 0.97. A statistically significant difference was not found when TSH levels of bipolar patients were compared with control group (z=-1.17; p=0.24). Mean fT4 values of patient and control groups were 1.00 ± 0.10 and 1.11 ± 0.09, respectively. Mean fT3 of patient groups were compared.
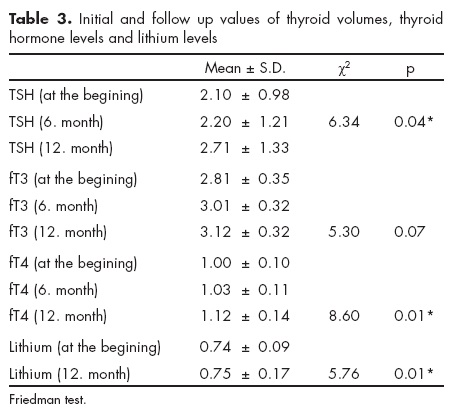
All volumes except right sagittal diameter (z=-1.28; p=0.19) and left sagittal diameter (z=-0.56; p=0.55) were detected to be greater in bipolar patients (p<0.05). Comparison of initial thyroid volumes of patient and control groups is summarized in table 2. Euthyroid status change occurred in no patients; ft3, ft4 and TSH were within normal ranges. No patients discontinued lithium therapy and they came for controls regularly. Change in TSH levels at the beginning of the study (2.10 ± 0.98), at six months (2.20 ± 1.21) and at the first year (2.71 ± 1.33) was found statistically significant (χ2=6.34; p=0.04). A significant difference was detected between lithium levels measured at the beginning of the study (0.74+0.09) and after one year (0.75 ± 0.17). Lithium levels measured after one year were found higher (χ2=5.76; p=0.01). Thyroid hormone levels at the beginning, initial and follow-up levels of lithium are given in table 3.
A significant correlation was not detected between the final TSH value and duration of disease, duration of lithium use, thyroid volumes on ultrasonography, initial TSH value and lithium level (p>0.05) (table 4).

DISCUSSION
In this study, thyroid hormones did not change in the course of lithium therapy in euthyroid patients with bipolar I disorder who were using lithium and who were in remission. Euthyroid status did not change in one year follow-up although the patients were using lithium regularly. Thyroid volume of patients was significantly greater than healthy controls at the beginning of the study. There was not a significant difference between initial TSH values of both groups, but fT3 and fT4 values of bipolar patients were significantly lower than those of controls. Plasma lithium level and TSH values were significantly elevated at the end of one year follow-up although they stayed within normal values. Lithium use is known to reduce synthesis and release of thyroid hormone.30 Initial low fT3 and fT4 levels may be associated with lithium use in bipolar patients. fT4 level was found to be lower in lithium-treated bipolar patients compared to healthy controls in a study.31 In a 15-year follow-up study of Bocchetta et al., yearly hypothyroidism ratio was found at 1.5% in lithium-treated bipolar patients.32 No patients developed hypothyroidism in our study. Ezzaher et al. found TSH values of bipolar I patients higher than healthy controls. Hy-pothyroidism was found in the ratio of 28.5% in that study.33 Under the light of our findings, it may be suggested that lithium treatment is safe in patients who stayed euthyroid when using lithium and treatment may be continued by doing required tests.
Increased thyroid volume on ultrasonography is an expected finding in patients who have been using lithium for a long time.17,30,34-36 Bauer et al. reported that thyroid enlargement that cannot be detected by palpation may be detected with ultrasonography and they recommended regular ultra-sonography examinations.22 An association was not found between thyroid volumes and hypothyroidism in lithium-treated bipolar patients in a study.31 In our study, the final TSH value and initial thyroid diameters, duration of lithium therapy and total duration of disease were not associated. Significance of thyroid diameter increases may be understood with follow-up studies with longer duration.
Bauer et al. found that TSH values were higher in bipolar patients who did not receive thyroid hormone replacement compared to healthy controls.22 Zhang et al. found that TSH levels increased with time in lithium-treated patients.37 In our study, TSH levels tended to elevate in one-year follow-up and this elevation was not found to be correlated with lithium level. Increase in TSH levels indicates the significance of follow-up of this parameter although it stayed within normal ranges.
Five out of 28 subjects in patient group were excluded from the study as thyroid nodule was detected on thyroid ultrasonography. It is not possible to detect the relationship between lithium therapy and thyroid nodules due to the small number of patients. However, we may suggest that thyroid nodule may be detected in lithium-treated patients and care must be taken.
The small number of patients and the relatively short duration of the follow-up are the major limitations of our study. Nutrition-related confounding factors like iodine consumption were not studied in the study. It would not be proper to generalize this to all lithium-treated patients as lithium-treated euthyroid patients were analyzed in our study. Psychotropic drugs beside lithium may be a confounding factor.
In conclusion, lithium use may lead to an increase in thyroid volumes although the patients are euthyroid. Thyroid volumes were not found to be related with TSH levels one year later in our study. According to these results, it may be considered that lithium may be used safely in euthyroid patients if required tests are performed.
REFERENCES
1. Boccheta A, Loviselli A. Lithium treatment and thyroid abnormalities. Clinical Practice Epidemiology Mental Health 2006;2:23. [ Links ]
2. Sadock BJ, Sadock VA. Comprehensive textbook of psychiatry. Vol. 2, 7th edition Philadelphia: Lippincott Williams Wilkins; 2000. [ Links ]
3. Deodhar SD, Sing B, Pathak MC, Sharan P et al. Thyroid functions in lithium-treated psychiatric patients. Biol Trace Element Res 1998;67:151. [ Links ]
4. Perrild H, Hegedus L, Baastrup PC, Kayser L et al. Thyroid function and ultrasonically determined thyroid size in patients receiving longterm lithium treatment. Am J Psychiatry 1990;147:1518. [ Links ]
5. Bocchetta A, Bernardi F, Pedditzi M, Loviselli A et al. Thyroid abnormalities during lithium treatment. Acta Psychiatr Scand 1991;83(3):193-8. [ Links ]
6. Lee S, Chow CC, Wing YK, Shek CC. Thyroid abnormalities during chronic lithium treatment in Hong Kong Chinese: a controlled study. J Affect Disord 1992;26:173-178. [ Links ]
7. Bochetta A, Cherchi A, Loviselli A, Mossa P et al. Six-yearfollow- up of thyroid function during lithium treatment. Acta Psychiatr Scand 1996;94:45-48. [ Links ]
8. Loviselli A, Bocchetta A, Mossa P, Velluzzi F et al. Value of thyroid echography in the long-term follow-up of lithium-treated patients. Neuropsychobiology 1997;36(1):37-41. [ Links ]
9. Livingstone C, Rampes H. Lithium: A review of its metabolic adverse effects. J Psychopharmacol 2006;20:347-355. [ Links ]
10. Ahmadi-Abhari SA, Ghaeli P, Fahimi F, Esfahanian F et al. Risk factors of thyroid abnormalities in bipolar patients receiving lithium: a case control study. BMC Psychiatry 2003;3:4. [ Links ]
11. Schoenberg M, Ts'O TOT, Meisel AN. Graves' Disease manifesting after maintenance lithium. The J Nerv Ment Disease 1979;167(9):575-77. [ Links ]
12. Reisberg B, Gershon S. Side effects associated with lithium therapy. Arch Gen Psychiatry 1979;36:879-87. [ Links ]
13. Pohl R, Berchou R, Gupta BK. Case report: Lithium induced hypothyroidism and thyroiditis. Biol Psychiat 1979;14(5):835-37. [ Links ]
14. Transbol I, Christiansen C, Baastrup PC. Endocrine effects of lithium. Primay Hypothyroidism, its prevalence in long term treated patients. Acta Endocrinologica 1978;87:579-67. [ Links ]
15. Kirov G. Thyroid disorders in lithum-treated patients. J Affect Disord 1998;50:33. [ Links ]
16. Chow CC, Lee S, Shek CC, Wing YK et al. Lithium-associated transient thyrotoxicosis in 4 chinese woman with autoimmune thyroiditis. Aust N Z J Psychiatry 1993;27:246. [ Links ]
17. Ozsoy S, Mavili E, Aydin M, Turan T et al. Ultrasonically determined thyroid volume and thyroid functions in lithium-naïve and lithium-treated patients with bipolar disorder: a cross-sectional and longitudinal study. Human Psychopharmacology Clinical Experimental 2010;25(2):174-178. [ Links ]
18. Bernstein JG. Drug therapy in psychiatry. 3rd ed., Massachusetts: Aimes Mirror Company; 1995. [ Links ]
19. Tuğlular I. Psikiyatride İlaç Kullanimi. 1. Baski, Drug use in psychiatry, 1. edition, İn İzmir. Turkish: Ege Üniversitesi Basimevi; 1991; pp. 257-298. [ Links ]
20. Yüksel NY, Köroğlu E. Klinik Uygulamali Psikofarmakoloji. 1. Baski, Clinical Psychopharmacology. 1. Edition. Ankara, Turkish: Hekimler Yayin Birligi; 1991; pp. 160-190. [ Links ]
21. Vahip S. Mood stabilizers: Lithium, carbamazepine, valproate Güleç C., Köroğlu E., Psikiyatri Temel Kitabi. Cilt 2, 1. Baski, Ankara, Turkish: Hekimler Yayin Birligi; 1998; p. 995. [ Links ]
22. Bauer M, Blumentritt H, Finke R, Schlattmann P et al. Using ultrasonography to determine thyroid size and prevalence of goiter in lithium-treated patients with affective disorders. J affect Disord 2007;04(1-3):45-51. [ Links ]
23. Schiemann U, Hengst K. Thyroid echogenicity in manic-depressive patients receiving lithium therapy. J Affect Disord 2002;70:85-90. [ Links ]
24. Akdemir A, Örsel S, Dağ İ, Turkcapar H et al. Validity, reliability and clinical use of Hamilton depression rating scale. Psikiyatri Psikoloji Psikofarmakoloji Dergisi (İn Turkish) 1996;4:251-9. [ Links ]
25. Karadağ F, Oral ET, Aran Yalçin F, Erten E. Validity and reliability of Young Mania Rating Scale in Turkey. Türk Psikiyatri Dergisi (ín Turkish) 2002;13:107-114. [ Links ]
26. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders -clinical version (SCID-CV). Washington, DC: American Psychiatric Press; 1997. [ Links ]
27 Çorapçioğlu A, Aydemir Ö, Yildiz M, Esen A et al. Structured clinical interview for DSM-IV axis I disorders -clinical version (SCID-CV) in Turkish version: Study of reliability. İlaç ve Tedavi Dergisi (in Turkish) 1999;12:233-236). [ Links ]
28. Spitzer RL, Williams JBW, Gibbon M, First M. Structured clinical interview for DSM-III-R, non-patient edition (SCID-NP, Version 1.0). Washington DC: American Psychiatric Press; 1990. [ Links ]
29. Sorias S, Saygili R, Elbi H. Turkish version of structured clinical interview for DSM-III-R, non-patient edition (SCID-NP, Version 1.0), (in Turkish). Bornova: Ege Üniversitesi Basimevi; 1990; [ Links ]
30. Kibirige D, Luzinda K, Ssekitoleko R. Spectrum of lithium induced thyroid abnormalities: a current perspective. Thyroid Res 2013;6(1):3. [ Links ]
31. Ozpoyraz N, Tamam L, Kulan E. Thyroid abnormalities in lithiumtreated patients. Adv Ther 2002;19(4):176-84. [ Links ]
32. Bocchetta A, Cocco F, Velluzzi F, Del Zompo M et al. Fifteen-year follow-up of thyroid function in lithium patients. J Endocrinol Invest 2007;30(5):363-366. [ Links ]
33. Ezzaher A, Haj Mouhamed D, Mechri A, Neffati F et al. Thyroid function and lipid profile in bipolar I patients. Asian J Psychiatr 2011;4(2):139-43. [ Links ]
34. Bou Khalil R, Richa S. Thyroid adverse effects of psychotropic drugs: a review. Clin Neuropharmacol 2011; 34(6):248-255. [ Links ]
35. Gau CS, Chang CJ, Tsai FJ, Chao PF et al. Association between mood stabilizers and hypothyroidism in patients with bipolar disorders: a nested, matched case-control study. Bipolar Disord 2010;12(3):253-263. [ Links ]
36. Lazarus JH. Lithium and thyroid. Best Pract Res Clin Endocrinol Metab 2009;23(6):723-733. [ Links ]
37. Zhang ZJ, Qiang L, Kang WH, Tan QR et al. Differences in hypo-thyroidism between lithium-free and -treated patients with bipolar disorders. Life Sci 2006;78(7):771-6. [ Links ]
Declaration of conflict interest: None














