Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Salud mental
versión impresa ISSN 0185-3325
Salud Ment vol.37 no.1 México ene./feb. 2014
Artículo original
Cognitive conflicts and symptom severity in dysthymia: "I'd rather be good than happy"
Conflictos cognitivos y gravedad de los síntomas en la distimia: "Prefiero ser bueno que feliz"
Adrián Montesano,1 Guillem Feixas,2 Luis A. Saúl,3 María I. Erazo Caicedo,4 Gloria Dada,2 David Winter5
1 Universitat de Barcelona, Facultat de Psicología, Departament de Personalitat, Avaluaciò i Tractament Psicològics.
2 Department of Personality, Assessment and Psychological Treatments, Universitat de Barcelona, Spain.
3 Universidad Antonio Nariño, Cali, Colombia.
4 Department of Personality, Assessment and Psychological Treatments, Universidad Nacional de Educación a Distancia, Madrid, Spain.
5 Department of Psychology, College Lane, University of Hertfordshire, Hatfield, Hertfordshire, UK.
Correspondence:
Adrián Montesano,
Department of Personality, Assessment and Psychological Treatments,
Faculty of Psychology, Universitat de Barcelona. Passeig Vall d'Hebron,
171, 08035 Barcelona, Spain. E-mail: adrianmontesano@ub.edu
Received first version: July 23, 2012.
Second version: August 29, 2013.
Third version: November 11, 2013.
Accepted: December 4, 2013.
ABSTRACT
A method for studying cognitive conflicts using the repertory grid technique is presented. By means of this technique, implicative dilemmas can be identified, cognitive structures in which a personal construct for which change is wished for implies undesirable change on another construct. We assessed the presence of dilemmas and the severity of symptoms in 46 participants who met criteria for dysthymia and compared then to a non-clinical group composed of 496 participants. Finally, an analysis of the specific content of the personal constructs forming such dilemmas was also performed. Implicative dilemmas were found in almost 70% of the dysthymic participants in contrast to 39% of controls and in greater quantity. In addition, participants in both groups with this type of conflict showed more depressive symptoms and general distress than those without dilemmas. Furthermore, a greater number of implicative dilemmas was associated with higher levels of symptom severity. Finally, content analysis results showed that implicative dilemmas are frequently composed of a constellation of moral values and emotion, indicating that symptoms are often related to moral aspects of the self and so change processes may be hindered. Clinical implications of targeting implicative dilemmas in the therapy context are discussed.
Key words: Dysthymia, Repertory Grid Technique, cognitive conflicts, implicative dilemmas, content analysis, personal constructs.
RESUMEN
En este estudio se presenta un método para el estudio de los conflictos cognitivos utilizando la técnica de rejilla. Por medio de ella, se identificaron los dilemas implicativos, una estructura cognitiva en la que un constructo personal en el que se desea un cambio se asocia con otro constructo en el que el cambio no es deseable. Se evaluó la presencia de dilemas y la gravedad sintomatológica en una muestra de 46 participantes que cumplían criterios diagnósticos para la distimia y se comparó con un grupo control compuesto por 496 participantes. Por último, se llevó a cabo un análisis del contenido de los constructos personales que forman los dilemas. Se encontraron dilemas en casi 70% de la muestra clínica frente a 39% de la muestra control y en mayor cantidad. Por otro lado, los participantes de ambos grupos con este tipo de conflicto mostraron un nivel mayor de sintomatología depresiva y malestar general que aquellos sin dilemas. Además, se encontró una alta correlación entre el número de dilemas implicativos y la gravedad de los síntomas. Los resultados del análisis de contenido mostraron que los dilemas estaban frecuentemente formados por una constelación de valores morales y constructos emocionales indicando que a menudo los síntomas están asociados a aspectos positivos del sí mismo, por lo que el proceso de cambio puede verse bloqueado. Se discuten las implicaciones clínicas de abordar los dilemas en el contexto terapéutico.
Palabras clave: Distimia, técnica de rejilla, conflictos cognitivos, dilemas implicativos, constructos personales, análisis de contenido.
INTRODUCTION
According to the World Health Organization, there are approximately 121 million persons with depressive disorders and these are among the leading causes of disability around the world. It is estimated that by the end of this decade depression will be the second leading cause of morbidity.1 As yet, the etiology of depressive disorders is not fully understood, but the biopsychosocial model has gained increasing support over the past decades and is assumed to best explain the disorder.
In the psychological arena, the literature addressing cognitive aspects of depressive disorders has so far grown rapidly, with increasing precision and elaboration. Most studies have focused on Beck's and colleagues' original descriptions of depressive cognitions.2,3 However, the systematic study of the subjective experience of depression (for instance, how patients particularly construe their selves and significant others) has received less attention. Contributions from Personal Construct Theory4 (PCT) may be helpful in complementing current models of depression by investigating subjective processes and structures of self-construing. In addition, research on cognitive features of depression has mainly focused on patients with major depression, whereas the milder condition of dysthymia has received little attention.5 Thus, the goal of this study is to explore, from a constructivist framework, the personal constructs of patients with a diagnosis of dysthymia. Concretely, we study the role and the content of identity-related cognitive conflicts and their relationship with symptom severity.
Similar to subsequent cognitive therapies, PCT propounds that the process of attributing meaning to experience is the most important activity of human psychological functioning.4 In Kelly's view, we strive to give meaning to our universe, ourselves and the ongoing experience of everyday life. To this end, humans create an evolving theoretical framework. Just as scientific theories are made of theoretical constructs, personal theories are composed of what Kelly termed "personal constructs". They represent bipolar dimensions of meaning which are organized in a hierarchical and (more or less) complex network system. In short, the personal construct system comprises the specific subjective way in which each person construes experience.6
Inspired by PCT, researchers have developed tools for the systematic study of subjective experience. The most widely used instrument is the Repertory Grid Technique (RGT), aimed at the elicitation, through a semi-structured interview, and exploration of a person's personal constructs.7 One of the advantages of the RGT is that it allows one to perform and combine quantitative and qualitative analyses based on the grid data matrix resulting from the ratings of constructs across a set of elements (usually self, ideal self and significant others). Indeed, several measures of self-construing and system organization can be derived from the RGT analyses.
Various studies8-11 have pointed out the utility of exploring the construct system in the evaluation of depressive disorders. For example, Neimeyer and Feixas8 showed that measures derived from the RGT tapped some cognitive features (e.g., rigidity) that symptom and standard cognitive measures of cognitive distortions did not account for. Of great importance here is the study of cognitive structures involved in change processes as long as dysthymic patients, by definition, show a chronic course of the disorder.12 With regard to change, a PCT-based line of research explored the idea that symptoms (e.g., low self-esteem) can be associated, by construct implications, to positive aspects of the self (e.g., being sensitive) so that the process of change might be hindered. From this point of view, symptom persistence could be better understood by considering the implication lines among constructs and the conflict derived from these implications.
Preliminary data from the Multi-Centre Dilemma Project research group13 (see at www.usal.es/tcp) indicated that Implicative Dilemmas (IDs) were the most explanatory type of cognitive conflict detected in the personal construct systems of a large clinical sample. Furthermore, the number of IDs was associated with higher levels of symptoms13 and the resolution of IDs, after a psychotherapeutic process, was related to symptom improvement.14
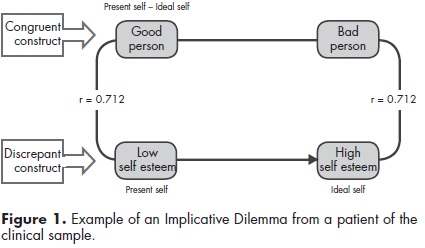
Two types of constructs are involved in an ID. On the one hand, discrepant constructs indicate discrepancies in self-representations. These self-discrepant cognitions occur when people's beliefs about themselves do not match their own expectations (self versus ideal self). Thus, discrepant constructs reveal dissatisfaction areas, usually reflecting symptomatic aspects. On the other hand, congruent constructs are those in which people see their actual selves akin to how they would ideally like to be. Therefore, congruent constructs are often related to personal values and qualities which persons would not like to change at all. So, an ID arises whenever there exists a strong association between a construct in which the person wishes to change (discrepant) and another construct in which change is not desirable (congruent) such that change in a desirable direction on the former is associated with movement away from the ideal self on the latter. This association between constructs within the context of a personal construct system could constitute an explanation of the relative resistance to change of a depressed patient.
As said before, the personal construct system is hierarchically organized, and so some subordinate constructs could be directly related to others of greater significance for the individual. For example, the construct "sad-happy" could be related to higher order constructs such as "good person-bad person" which belong to the core of the system. Core constructs provide a sense of continuity of the self and, thus, define the person's identity. Consequently, whenever a person holds an ID, trying to move to the desired pole of the discrepant construct may also imply moving away from a core quality that the person estimates as part of his or her identity. Arguably, such a process challenges the person's identity and might generate greater distress, eventually impeding the achievement of the desired change and maintaining the symptoms.
For instance, the patient illustrated in figure 1 desired a change from having low self-esteem to being a person with high self-esteem (note that here "self-esteem" is a personal construct, not a theoretical one). However, the dilemma occurred because changing on this discrepant construct implied an undesired change on the congruent construct, that is, becoming a "bad person". In other terms, a movement of the self to the opposite pole of the discrepant construct generated a dilemmatic situation because the pole of this construct where the self was originally situated was associated by implication to the preferred pole of a congruent construct. Therefore, that movement would result in invalidation of core aspects of the self.
Cognitive conflicts are not regarded as a specific feature of depression. The extant research15-17 on this kind of cognitive structure suggests that cognitive conflicts, and specially IDs, are a common phenomenon cutting across a variety of diagnostic categories. However, it seems reasonable to hypothesize that IDs, which provide an explanation for resistance to change, might play a noticeable role in depression and dysthymia taking into account their high rates of relapse and recurrence and the tendency towards a chronic course of the disease.
Currently, relapse and recurrence are the most pressing challenges to address in research on and treatment of depression. Research on cognitive conflicts could shed light on the processes underlying such unfortunate phenomena not only by providing a theoretical explanation but also by offering a procedure of clinical intervention insofar as IDs are amenable to therapeutic work. In fact, a specific brief intervention has been devised18-22 to target IDs in clinical settings. Focusing the intervention on this cognitive structure helps therapists in case formulation and treatment planning and might help improve the efficacy of existing treatments for depression.
The general objective of this study is to explore the cognitive conflicts of a group of persons with a diagnosis of dysthymia as compared to a non-clinical sample. The target of the assessment consisted of identifying the presence of IDs using the RGT and examining their relationship with severity of symptoms. In addition, we analysed, in the clinical sample, the specific content of congruent and discrepant constructs forming such IDs. In a previous study23 we examined the content of personal constructs in depression but not specifically in dysthymia, and the content of IDs was not analysed. Although we found particular patterns of content for depressed participants, we conclude that more research should be carried out to better understand the role of moral values, for which differences were not found, and emotion, insofar as these are crucial areas of content for this kind of patient.
MATERIALS AND METHODS
Participants
The sample of the study consisted of 542 participants distributed in two groups. On the one hand, the clinical group (n=46) was composed of persons seeking psychological treatment in private clinics of the city of Barcelona, Spain. The inclusion criteria for the study were: a) 18 to 65 years of age, and b) meeting diagnostic criteria for dysthymia according to DSM-IV-R.12 Exclusion criteria were: a) presenting other Axis I diagnoses, b) presence of psychotic symptoms, and c) organic mental disorder or pervasive developmental delay. The mean age of this clinical sample was 42.30 (SD=15.76); 76.1% were women. The non-clinical group was formed by a convenience sample of 496 participants with a mean age of 28.51 (SD=9.63); 61.3% were women.
Instruments and measures
Repertory Grid Technique
The RGT is a constructivist assessment procedure originally proposed by Kelly.4 It has evolved in a variety of formats depending on the needs of the researcher.7,24 It has been applied to the study of a variety of research topics within psychology and other disciplines.25 In the present study, we used an interpersonal version of the grid. To complete the administration process, three stages were needed. First, participants identified a set of significant others from their interpersonal world that, alongside the "present self" and the "ideal self", constituted the elements of the grid (columns). Secondly, the constructs (rows) were elicited by describing similarities and differences between pairs of elements. Finally, the participant rated each element on the grid on each construct using a 7-point Likert scale ranging from very much like the right pole to very much like the left pole of the construct. For our purpose, two measures related to IDs were used:
a) The presence (or absence) of IDs in the grids. According to Feixas and Saúl,13 a construct is classified as discrepant when the ratings assigned to the element "present self" and the element "ideal self" differ by four or more points within the 7-point scale used. On the other hand, those constructs in which the score given to the "present self" and the "ideal self" coincide (or there is no more than one point of difference) are identified as congruent constructs. Whenever either of the two elements is rated as four (the middle point), then it is excluded from this classification. IDs are detected whenever the correlation between the scores given to a discrepant con- struct and those given to a congruent construct is .35 or higher, indicating an association between the desired pole of the discrepant construct and the undesired pole of the congruent one. This is a dichotomous variable scoring <<1>> for those participants for whom at least one ID is found, and <<0>> for those for whom none is found.
b) The percentage of implicative dilemma (PID). The PID reveals the number of IDs in a grid taking into account its size. The number of constructs elicited during administration varies from one grid to other, influencing the possible number of IDs within a grid. This measure is calculated by dividing the number of dilemmas of a grid by the total number of possible combinations of constructs in such a grid taking two at a time. The resulting proportion is multiplied by 100 to obtain the percentage. The mathematical analysis of the RGT was performed using the GRIDCOR v. 4.0 software created by Feixas and Cornejo.24
Classification System for Personal Constructs (CSPC)
The CSPC is a system developed by Feixas, Geldschläger and Neimeyer26 designed to analyse and classify the content of personal constructs derived from constructivist assessment procedures, and particularly from the RGT. The CSPC is composed of 45 comprehensive and mutually exclusive categories arranged into six thematic areas (moral, emotional, relational, personal, intellectual, specific values and interests). Those areas are hierarchically ordered as listed above to increase the reliability of the system by eliminating potential overlap among them: whenever a construct fits within two or more areas, it is coded in the area of higher level. Categories belonging to the same area are considered at the same hierarchical level. It is considered an instrument with high methodological quality, versatility and with a promising applicability.27 It has already been applied to personal constructs of depressed23 and other patients,17 but not of dysthymics and the content of the constructs forming IDs has not been analysed. Feixas et al.26 reported a high reliability index for the CSPC (Cohen's Kappα=0.93).
Symptom Checklist -90- Revised
The SCL-90-R28,29 is a self-administered questionnaire composed of 90 items that assess psychological distress across nine dimensions. For the present study we used two measures: a) Global Severity Index (GSI), which indicates the overall level of discomfort suffered by the subject taking into account all the variety of symptoms and their intensity, and b) the depression subscale (DS).
Procedure
Participants of the clinical group were recruited during a five-year period in various private clinical centres of the province of Barcelona. Diagnoses were made by their psychotherapists, who had a minimum of six years of experience. Those who agreed to participate were interviewed on at least two occasions before therapy started. At the initial interview, participants were asked to provide informed consent and all doubts about the research were discussed. Sociodemographic data was also gathered. Then, the RGT was administered, the elicitation and rating phases being carried out conjointly by the participant and the interviewer. Before initiating the therapy, participants also completed the SCL-90-R.
Participants in the control group were volunteers recruited and assessed by psychology undergraduate or master students (trained in the application of RGT) in face-to-face interviews. All participants provided informed consent on forms approved by local research ethics committees.
Finally, pairs of independent graduate and undergraduate students well-trained in the CSPC performed the content analysis of the personal constructs. The training consisted in rating a set of 150 constructs from a sample used in another study. To avoid biased ratings, the coders were blind to the hypothesis of the study and did not know whether the grids belonged to the clinical or the control sample. Inter-rater analysis yielded high levels of agreement (K=.91; p<.001).
Statistical analyses
Data collected from RGT was analyzed with the software GRIDCOR v. 4.024 and dumped into the Statistical Package for Social Sciences version 20.0(IBM Corporation, Armonk, New York, USA) datasheet for further analyses. First, the clinical and control groups were compared in order to identify differences in the presence and number of IDs. We used the Student-T test for continuous variables and the Chi-square test for categorical variables. Second, Student-T test and non-parametric Spearman's rank order Correlation were used to describe the relationship between IDs and symptom severity. Finally, Chi-square test and confidence intervals were used to compare the content of congruent and discrepant constructs within the clinical sample.
RESULTS
Presence of implicative dilemmas
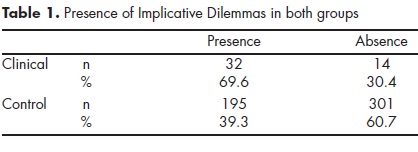
In order to determine whether the proportion of participants having IDs was different across samples, a Chi-square test was performed. Yates correction for continuity was used to compensate for the overestimate of Chi-square value for a 2x2 contingency table. The clinical sample contained significantly (x2 [1]=14.6; p<.001; phi=.17) more participants with one or more IDs than the control group (table 1). Then, an independent samples t-test was conducted to compare the PID of clinical (M=2.58; SD=3.52) and non-clinical (M=.87;SD=1.7) samples. The significant difference found between the two groups (t [47.03]=-3.25; p=.002; d=.62) indicated a greater number of IDs in the former, with a medium effect size.
Implicative dilemmas and symptomatology
Data of the SCL-90-R were available for 234 participants, 199 from the non-clinical sample and 35 from the clinical one. First, two independent samples t-tests were conducted to compare GSI (t [32.99]=4.47, p<.001, d=1.41) and DS (t [32.94]=6.29, p<.001, d=1.99) scores within the clinical sample. Participants with IDs (n=25) yielded an average score on the GSI of 1.19 (SD=.44) and on the DS of 1.86 (SD=.67), whereas for those without IDs (n=10) it was .72 (SD=.17) and .85 (SD=.27), respectively. Second, the same analyses were conducted for the non-clinical group. Participants with IDs (n=84) showed an average on the GSI of .66 (SD=.39) and on the DS of .89 (SD=.63), whereas for the remainder (n=115) it was .49 (SD=.34) for the GSI and .64 (SD=.50) for the DS. Independent samples t-tests showed significant differences for both the GSI (t [197]=3.33, p=.001, d=0.48) and the DS (t [153.86]=3.13, p=.002, d=.44).
Finally, the relationship between PDI and SCL-90-R scores was inspected using Spearman's coefficient due to the skewed distribution of the former. In the clinical sample there were strong correlations between PDI and GSI (rho=.48, n=35, p<.001) and between PDI and DS (rho=.57, n=35, p<.001). Likewise, significant correlations were found in the control group (rho=.22, n=199, p=.002, for the GSI and rho=.21, n=199, p=.004 for the DS).
Content analysis of implicative dilemmas
Table 2 illustrates the coding of congruent and discrepant constructs forming IDs in the clinical sample. A chi-squared test showed that these types of constructs differed in their content (x2 [5]=71.16; p<.001, Cramer's V=.49). In order to know in which particular areas they were differentiated, adjusted standardized residuals where compared to the critical value of ± 1.96 (α=0.05). Differences were found in the moral, emotional, and interest areas.
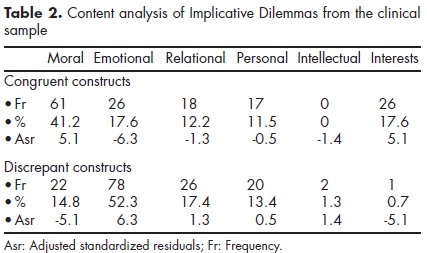
Once the difference in content between the types of constructs was established, we estimated, separately, the confidence intervals of proportion for congruent and discrepant constructs in each area of the CSPC. While the proportion of congruent constructs that belonged to the moral area differed significantly from the proportion in the rest of the areas, most of the discrepant constructs were significantly associated with the emotional area (table 3).
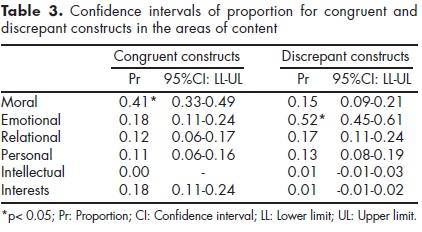
In order to analyse in more detail the content of the IDs, we observed the frequency of congruent and discrepant constructs in each category of the relevant areas described above. In regard to congruent constructs, the categories "altruist-egoist" and "responsible-irresponsible" were the most frequently rated. For discrepant constructs, the category "balanced-unbalanced" significantly stood out from the rest of the categories. The categories "optimist-pessimist", "warm-cold" and "specific emotions" were also frequent (table 4).
DISCUSSION
Results obtained in this study were in line with previous findings,13,15-18 which consistently pointed towards a higher rate of IDs in clinical samples. We found IDs in over two thirds of dysthymic patients in contrast to only 39% of controls. Moreover, differences between groups were underlined by the fact that dysthymic participants significantly presented a higher quantity of IDs.
Although conflictual configurations of constructs have proved their relevance for patients with other diagnoses,30-32 results from this and other preliminary* studies suggest that cognitive conflicts are particularly pertinent for depressive disorders due to the prototypical pattern of self-construing among these patients. Self-construing in depression often entails not just elevated self-ideal discrepancies but a mixed pattern of positive and negative perceptions.33
Although IDs are a natural constellation of constructs, their relation to symptom behaviour became more evident when exploring correlations with symptom severity. Among dysthymic participants, those who presented one or more IDs displayed significantly (and with large effect sizes) higher levels of depressive and global symptom severity. Furthermore, a greater number of IDs was strongly associated with higher levels of distress. In fact, correlations from this study were much higher than in previous research.18 Future research should clarify whether the relationship between the number of dilemmas and the severity of symptoms is linear or not. Nevertheless, findings from our study suggested that the higher level of severity is related to a higher number of dilemmatic implications within the construct network of dysthymic patients. To a certain extent, the persistence of symptoms and the tendency towards chronicity in dysthymia could be explained by a high level of conflicts and, in turn, this might be the reason of the greater correlations found in this study.
The results from the content analysis of the IDs offered a much more detailed picture of not only the nature of these conflicts, but also of the role of moral and emotional constructs in the clinical participants' construction of their experience. Another study,16 in which the general content of personal constructs was analysed, did not demonstrate the relevance of moral constructs in the grids of depressed patients. However, the strategy of analysing the content of the specific constructs forming IDs has yielded more precise findings. The content analysis results have also provided evidence for the construct validity of congruent and discrepant constructs.
Congruent constructs, which provide people with a crucial source of coherence and continuity, mostly were of a moral nature. Conversely, discrepant constructs usually presented content related to the degree of emotional balance but also to the "optimism-pessimism" and "warm-cold" dimensions, and other specific emotions such as melancholy, apathy and sadness. Ostensibly, these areas of content are particularly relevant dimensions of meaning for understanding the psychological distress of dysthymic patients if we consider central features of the disorder such as emotional dysregulation, low self-esteem and feelings of hopelessness.12
It seems that the manner of conflictual self-construing in most dysthymic patients in the present study conforms to the observations made by Rowe34,35 and Winter36 about the dilemmatic implications for change of depressive patients. They pointed out that they typically embrace self-constructions whereby they should choose either being depressed but human or being happy but unpleasant: "I'd rather be good than happy". In view of such a dilemma, it is not surprising that they might decide to maintain their positive features even though when not changing implies suffering, inasmuch as from this position they avoid the invalidation of core constructs and preserve their sense of personal identity.
We do not consider this thematic composition of IDs as specific for dysthymic patients. As we said above, IDs are common across different disorders. Thus, we look upon this thematic composition as a general constellation of content in which congruent constructs are mostly of a moral nature and discrepant ones refer to symptomatic areas, which thereby, may subtly vary across different diagnoses. However, the conflictual construct configuration found in this study and its content seems really pertinent to understand the kind of dilemmas depressive patients might face. For instance, according to the hypothesis of Linares and Campo,37 the identity of people with depression is built on the ineluctable need of doing "what is right", "what must be done" and "being what the others are expecting". The effort to maintain these requirements can undoubtedly lead to personal dilemmas in circumstances in which these conflictual structures are activated. Thus, emotional well-being could be jeopardized due to the need for preserving coherence of self-identity and personal values. From this point of view, is not only the emotional symptomatic aspect that disheartens depressed patients but the insurmountable weight of moral values and duty.
We do not say that depressive distress is a consequence of an unbearable hyper-morality. Undoubtedly, the moral aspects related to the congruent constructs assessed with the RGT represent healthy attributes of the identity. Precisely, the conflict arises when a patient assimilates a construction in which to stop being depressed involves seeing oneself as a despicable person, devoid of virtue.
From a clinical point of view, these findings suggest that therapists could benefit from screening for the presence of cognitive conflicts in patients experiencing difficulties to overcome their symptoms. In turn, using the RGT helps therapists to better understand the personal factors that maintain or worsen the disorder and allows treatment to be individualized to fit patient subjective experience. Several techniques can be applied to address cognitive conflicts in the therapeutic context such as laddering, Tschudis' ABC model,38 or the two-chair technique.* The interested reader can consult published case studies for major depression and other comorbidities,19 depressive and obsessive symptoms,39 or dysthymia.40 In addition, the efficacy of a dilemma-focused intervention in combination with cognitive behavioural therapy is being tested out for unipolar depression.41
While the results of this study have clarified the role of implicative dilemmas and their content for dysthymic patients, there are some limitations that need to be considered. First of all, the lack of a matched control group restricted the generalizability of the results; likewise, the current comparison group was formed of a convenience sample with no control for undiagnosed disorders. Indeed, these participants showed higher levels of symptoms than the Spanish normative data for the SCL-90-R.29 Nonetheless, given that the current findings were consistent with previous studies of cognitive conflicts with balanced samples of other clinical disorders, this limitation on generalizability may be negligible. On the other hand, the potential of IDs to explain relapse and recurrence would be better tested out by analysing longitudinal data of the course of the disorder, but the cross-sectional design of the study precluded such analyses. Future prospective research would also benefit from including assessment of changes in both the structure and the content of personal constructs systems and so enhancing the effectiveness in dealing with the chronic nature of dysthymic symptoms.
ACKNOWLEDGEMENT
This study was partially founded by the Spanish Ministry of Science and Innovation (ref. PSI2008-00406).
REFERENCES
1. World Health Organization. The global burden of disease: 2004 update. Geneva, Switzerland: 2008. [ Links ]
2. Beck AT. Depression: Clinical, experimental, and theoretical aspects. New York: Harper & Row; 1967. [ Links ]
3. Beck AT, Rush JA, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford; 1979. [ Links ]
4. Kelly GA. The psychology of personal constructs. New York: NortoiV London, Routledge; 1955/1991. [ Links ]
5. Hollon SD, Ponniah K. A review of empirically supported psychological therapies for mood disorders in adults. Depress Anxiety 2010;27:891-932. [ Links ]
6. Walker BM, Winter D. The elaboration of personal construct psychology. Annu Rev Psychol 2007;58:453-477. [ Links ]
7. Fransella F, Bell R, Bannister D. A manual for repertory grid technique. London: John Wiley & Sons; 2004. [ Links ]
8. Neimeyer RA, Feixas G. Cognitive assessment in depression: A comparison of some existing measures. European J Psychological Assessment 1992;8:47-56. [ Links ]
9. Feixas G, Bach L, Laso E. Factors affecting interpersonal construct differentiation when measured using the Repertory Grid. J Constructivist Psychology 2004;17:297-311. [ Links ]
10. Feixas G, Erazo MI, Harter S, Bach L. Construction of self and others in unipolar depressive disorders: A study using repertory grid technique. Cognitive Therapy Research 2008;32:386-400. [ Links ]
11. Sanz J. Constructos personales y sintomatologia depresiva: un estudio longitudinal. Revista Psicologia General Aplicada 1992;45:403-411. [ Links ]
12. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. (4th ed., Text Review). Washington, DC; 2000. [ Links ]
13. Feixas G, Saúl LA. The multi-center dilemma project: An investigation on the role of cognitive conflicts in health. Spanish J Psychology 2004;7:69-78. [ Links ]
14. Feixas G, Saúl LA, Winter D, Watson S. Un estudio naturalista sobre el cambio de los conflictos cognitivos durante la psicoterapia. Apuntes Psicologia 2008;26:243-255. [ Links ]
15. Dada G, Feixas G, Compañ V, Montesano A. Self construction, cognitive conflicts and disordered eating attitudes in young women. J Constructivist Psychology 2012;25:70-89. [ Links ]
16. Melis F, Feixas G, Varlotta N, González LM et al. Conflictos cognitivos (dilemas) en pacientes diagnosticados con trastornos de ansiedad. Revista Argentina Clínica Psicológica 2011;XX:41-48. [ Links ]
17. Compañ V, Feixas G, Varlotta N, Torres M et al. Cognitive factors in fibromyalgia: The role of self-concept and identity related conflicts. J Constructivist Psychology 2011;24:1-22. [ Links ]
18. Feixas G, Saúl LA, Ávila A. Viewing cognitive conflicts as dilemmas: implications for mental health. J Constructivist Psychology 2009;22:141-169. [ Links ]
19. Feixas G, Hermosilla S, Compañ V, Dada G. Camino hacia el coraje: terapia de constructos personales en un caso de depresión mayor, fibromialgia y otras comorbilidades. Revista Argentina Clinica Psicológica 2009;18:241-251. [ Links ]
20. Feixas G, Saúl LA. Resolution of dilemmas by personal construct psychotherapy. In: Winter D, Viney L (eds). Personal construct psychotherapy: Advances in theory, practice and research. London: Whurr; 2005; pp.136-147. [ Links ]
21. Fernandes E, Senra J, Feixas G. Psicoterapia construtivista: um modelo centrado em dilemas. Braga, Portugal: Psiquilibrios Edicöes; 2009. [ Links ]
22. Senra J, Feixas G, Fernandes E. Manual de intervención en dilemas implicativos. Revista Psicoterapia 2006;63-64:179-201. [ Links ]
23. Montesano A, Feixas G, Varlotta N. Análisis de contenido de constructos personales en la depresión. Salud Mental 2009;32:371-379. [ Links ]
24. Feixas G, Cornejo JM. RECORD v. 4.0: Análisis de correspondencias de constructos personales. Barcelona: Psimedia; 2002. [ Links ]
25. Saúl LA, López-González MA, Moreno-Pulido A, Corbella S et al. Bibliometric review of the Repertory Grid Technique: 1998-2007. J Constructivist Psychology 2012;25:112-131. [ Links ]
26. Feixas G, Geldschläger H, Neimeyer RA. Content analysis of personal constructs. J Constructivist Psychology 2002;15:1-19. [ Links ]
27. Green B. Personal construct psychology and content analysis. Personal Construct Theory Practice 2004;1:82-91. [ Links ]
28. Derogatis LR. SCL-90-R Symptom Checklist 90 Revised. Minnesota: NCS Pearson; 1994. [ Links ]
29. González de Rivera JL, de las Cuevas C, Rodriguez M, Rodriguez F. SCL-90-R Cuestionario de Síntomas [SCL-90-R Symptoms Inventory]. Madrid: TEA Ediciones; 2002. [ Links ]
30. Benasayag R, Feixas G, Mearin F, Saúl LA et al. Conflictos cognitivos en el sindrome del intestino irritable (SII): un estudio exploratorio. International J Clinical Health Psychology 2004;4:105-119. [ Links ]
31. Feixas G, Cipriano D, Varlotta N. Somatización y conflictos cognitivos: estudio exploratorio con una muestra clinica. Revista Argentina Clinica Psicológica 2007;16:194-203. [ Links ]
32. Feixas G, Montebruno C, Dada G, Del Castillo M e al. Self construction, cognitive conflicts and polarization in bulimia nervosa. International J Clinical Health Psychology 2010;10:445-457. [ Links ]
33. Space LG, Cromwell RL. Personal constructs among depressed patients. J Ner Ment Dis 1980;168:150-158. [ Links ]
34. Rowe D. Poor prognosis in a case of depression as predicted by the repertory grid. Br J Psychiatry 1971;118:231-244. [ Links ]
35. Rowe D. Depression: The way out of the prision. London Paul: Routledge & Kegan; 1983. [ Links ]
36. Winter D. Personal construct theory in clinical practice: Theory, research and applications. London: Routledge; 1992. [ Links ]
37. Linares JL, Campo C. Tras la honorable fachada. Los trastornos depresivos desde una perspectiva relacional. Barcelona: Paidós; 2000. [ Links ]
38. Tschudi F, Winter D. The ABC model revisited, in personal construct methodology. In: Caputi P, Viney LL, Walker BM, Crittenden N (eds). UK Ltd, Chichester: John Wiley & Sons; 2011. [ Links ]
39. Fernandes EM. When what I wish makes me worse... to make coherence flexible. Psychology Psychotherapy: Theory, research and practice 2007;80:165-180. [ Links ]
40. Montesano A, Feixas G, Muñoz D, Compañ V. Systemic couple therapy for Dysthymia: a case study. Psychotherapy 2014:51. [ Links ]
41. Feixas G, Bados A, García-Grau E, Montesano A et al. Efficacy of a dilemma-focused intervention for unipolar depression: study protocol for a multicenter randomized controlled trial. Trials 2013:14(144). [ Links ]
* Feixas G, Montesano A, Compañ V, Salla M et al. Measuring cognitive conflicts and their relevance for unipolar depression. 6th Biennial Conference of the International Society Affective Disorders, London; 2012. Available at http://www.scribd.com/doc/95551301/Measuring-Cognitive-Conflicts-and-Their-Relevance-for-Unipolar-slides.
* Montesano A, Feixas G, Salla M, Compah V. Combining group CBT with an individual Dilemma-Focused Intervention: A case study. Paper presented at the XXIX congress of the Society for the Exploration of Psychotherapy Integration. Barcelona; 2013. Available at:http://prezi.com/dl2nt-kk-dvf/combining-group-cbt-with-an-individual-dilemma-focused-intervention-a-case-study.
Declaration of conflict interest: None














