Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Salud mental
versão impressa ISSN 0185-3325
Salud Ment vol.36 no.1 México Jan./Fev. 2013
Artículo original
Factors related to health outcomes and health risk behaviors of adolescents with lead exposure. A pilot study
Factores relacionados con el estado de salud y conductas de riesgo para la salud de adolescentes con exposición a plomo. Un estudio piloto
Patricia Cossío-Torres,1 Jaqueline Calderón,2 Martha Tellez-Rojo,3 Fernando Díaz-Barriga2
1 Environmental Toxicology Department, Medicine School, Autonomous University of San Luis Potosí. Mexico.
2 Applied Research Center for Environment and Health, Autonomous University of San Luis Potosí. Mexico.
3 Center for Population Health Research, National Institute of Public Health. Cuernavaca, Mexico.
Correspondence:
Patricia Cossío-Torres.
PhD in Environmental Sciences.
Environmental Toxicology Department, Medicine School,
Autonomous University of San Luis Potosí.
Av. Venustiano Carranza 2405, 78210, San Luis Potosí,
SLP, Mexico.
Telephone and fax: (52-444) 826-2354.
E-mail: patricia.cossio@sip.uaslp.mx.
Recibido primera versión: 14 de septiembre de 2011.
Segunda versión: 14 de mayo de 2012.
Aceptado: 31 de agosto de 2012.
ABSTRACT
This pilot study was an approach to determine the health outcomes (nutritional status, cognitive status, mental health and educational status), and the presence of health risk behaviors (aggressive behavior/ delinquency, hazardous/harmful drinking, substance use/abuse and tobacco use) of adolescents who have been exposed all their lives to lead. Besides, we could identify individual, familial and social factors, such as lead exposure, that were related to them. The sample included 40 adolescents (25 females and 15 males), aged 12-19 years, who participated as children in the Childhood Lead Exposure Surveillance Program (CLESP), conducted in a metallurgical area of Mexico. The 100% of the participants were reported neurologically healthy by medical clinical examination. The 15% were below 70 points of the Full Scale Intelligence Quotient, higher than the expected percentage in the general Mexican population. Moreover, we detected the presence of health risk behaviors. The protective factors identified were mean cell volume, adolescent education, father education and living in an apartment. Risk factors identified were: sleep hours, mono-parental family, positive family history of substance use/abuse, residents by household, having social security, tibia bone lead, and childhood blood lead (p<0.05). The gender and exercise variables were accounted for both risk and protection. The health problems that we found were mostly related to individual factors, followed by familial and social factors. The lead exposure explained, in minor proportions, the multivariate models; however, for every 1 pg lead/g bone mineral increased in the tibia and 1 pg/dL increase in blood lead during childhood; the Perceptual Organization/Perceptual Reasoning Index and Processing Speed Index are decreased by 1.21 and 1.11~points, respectively. The detection of protective and risk factors enable the design of an intervention program as an extension of CLESP. The health of these adolescents can be improved by avoiding some risk factors and fostering protective factors at individual, family and community levels.
Key words: Adolescents, health outcomes, health risk behaviors, protective and risk factors, lead exposure.
RESUMEN
Este estudio piloto fue una aproximación para determinar el estado de salud (nutricional, cognitivo, salud mental y educacional) y las conductas de riesgo para la salud (agresión/delincuencia, consumo riesgoso/ dañino de alcohol, uso/ abuso de sustancias y consumo de tabaco) de adolescentes que han estado expuestos toda su vida al plomo. Se identificaron factores individuales, familiares y sociales; así como la exposición al plomo, que estuvieran relacionados con ellos. Se incluyeron 40 adolescentes (25 mujeres y 15 hombres) de 12 a 19 años de edad, quienes participaron siendo niños en el Programa de Vigilancia Infantil de Exposición a Plomo (PVIEP), conducido en un área metalúrgica de México. El 100% estaba neurológicamente sano por examen médico. El 15% obtuvo menos de 70 puntos en la Escala Total del Coeficiente Intelectual, porcentaje mayor al esperado en la población general mexicana. Además se detectó la presencia de conductas de riesgo. Los factores protectores identificados fueron volumen corpuscular medio, educación del adolescente, educación del padre y vivir en departamento. Los factores de riesgo fueron horas de sueño, familia monoparental, familia con antecedentes de uso/abuso de sustancias, número de residentes en la vivienda, tener seguridad social, plomo en tibia y plomo en sangre durante la infancia (p<0.05). El género y el ejercicio fueron variables tanto de riesgo como de protección. Los problemas de salud encontrados estuvieron mayormente asociados a factores individuales, seguidos por factores familiares y sociales. La exposición a plomo explicó en menor proporción los modelos multivariados, sin embargo, por cada 1 ug plomo/g de hueso mineral incrementado en tibia y 1 ug/dL de plomo incrementado en sangre durante la infancia, el Indice de Organización Perceptual/Razonamiento Perceptual e Indice de Velocidad de Procesamiento, disminuyeron 1.21 y 1.11 ~puntos, respectivamente. La detección de factores de riesgo y protección permitirá el diseño de un programa de intervención como parte del PVIEP. La salud de estos adolescentes puede ser mejorada aminorando algunos factores de riesgo y fomentando factores de protección, desde el nivel individual, familiar y/o comunitario.
Palabras clave: Adolescentes, estado de salud, conductas de riesgo para la salud, factores de riesgo y protección, exposición a plomo.
INTRODUCTION
One of every five people in the world, and in Mexico as well, is an adolescent; a healthy development in this group is a key point to progress of nations. Specifically in Mexico, the programs for adolescent attention have been functioning for almost four decades. However, investment has not been enough. Whereas the Mexican government targets 30 dollars per adolescent per year in health programs, 1,500 dollars are invested for every child under the age of nine.1 Therefore, services are limited for adolescent health services in terms of prevention, opportune detection, treatment and continuous rehabilitation.
In addition, more than 75 percent of all adolescent mortality is related mainly to social and behavioral factors.2 Moreover, some diseases occur during adolescence; and diseases that were latent during childhood might appear during this stage.3 Adolescents face new situations, and in order to prevent health risks, they frequently do not have enough elements in terms of knowledge, attitude and behavior. Adolescents' scant attendance to medical checkups, their inadequate diet, and use or abuse of tobacco, alcohol and illegal drugs; their early sexual debut, aggressive/delinquent behavior, and a context of poverty and marginalization, blended with exposure to environmental pollutants, such as lead and endocrine disruptors, trigger a synergy of effects that shape their health outcome and current well-being. This scenario hinders their transition to the adult stage, leaving sequels for the rest of their lives.
In relation to environmental pollutants, it is well known that lead is a neurotoxic, which can trigger dysfunction at mitochondria, excitotoxicity, influences on neurotransmitter, second messengers, astroglia and oligodendroglia.4 Cognitive functions and neurobehavior are affected by exposure to this metal, even at blood lead concentrations below 5.0 μg/ dl.4-6 The effects of lead exposure during childhood are present until adolescence and the young adult stage, or even 50 years after lead poisoning.6-13 In Mexico, lead exposure is still a problem, and the major sources of lead are the smelting and refining activities, and lead-glazed pottery.14-17
The studies in adolescents are focused mainly on sexual, psychosocial, and mental health aspects. In addition, the reach of the research that evaluates the effects of environmental pollutants, such as lead, in adolescent population is limited, and none of them have done integral assessments, they only have taken some social factors as covariates without demonstrating the contribution that each of them has (individual, familial, social and lead exposure) in the development of the adolescents.6,9-13 Therefore, it is essential to conduct research where lead exposure should be seen with other factors of individual, familial and social contexts affecting normal development.18 Besides, the research should recognize which factors are protective or risky in specific contexts; because they may be specific for certain adolescent health endpoints, as some of them may be relevant only during specific risk processes, and/or only at some windows of vulnerability (developmental stages). Moreover, the level of protection for some factors may depend on the individual's attributes. As for risk factors, they also operate in different ways at different age periods.19 In conclusion, adolescents are placed in a dynamic vulnerable-protective state; so for intervention, it is important to foster protective processes by developing protective factors, and/ or decreasing the influence of risk factors through their elimination or by intercepting their mechanisms of action.20,21 Furthermore, adolescent behavior could become a risk or protection factor by itself and influence their future development.2,22
Therefore, the first purpose of this work was to determine the health outcomes (nutritional status, cognitive status, mental health and educational status), and health risk behaviors (aggressive behavior/delinquency, hazardous/harmful drinking, substance use/ abuse and tobacco use) of adolescents who have been exposed all their lives to lead. The second purpose was to identify individual, familial and social factors, such as lead exposure, that were related to them.
METHODS AND MATERIAL
Study area
Morales is an urban area in San Luis Potosi, Mexico, where a smelter complex has been working since 1890. The historical accumulation of lead, cadmium and arsenic, mainly in soil and dust, represents a risk to children who live in this area.23,24 This evidence was detected through the Childhood Lead Exposure Surveillance Program (CLESP) that our research group has been operating in this site since 1993. Currently, nearly 30 500 inhabitants live in this site, 50.3% of whom are 24 years of age or younger. Considering these antecedents, we decided to extend the surveillance program to the adolescent population. This group is not only exposed to lead, they also live in a context of poverty and violence.
Study population
The adolescent sample was obtained from our CLESP databases (1993 to 2004). During 2007, there were only 85 individuals between 12 and 20 years of age, and only 40 met the inclusion criteria: adolescents, history of living in the study area since birth and having a written informed consent. Adolescents that were pregnant at the time of the study or occupationally exposed to lead were excluded. The study was approved by the Bioethics Committee of the School of Medicine, Autonomous University of San Luis Potosí.
Measurements
1. Nutritional assessment. Blood samples were taken for hemoglobin (Hb) and mean cell volume (MCV) as indicators of iron status. The cutoff points for iron deficiency were from the National Health and Nutrition Examination Survey (NHANES II), and from Dallman.25 Their weight and height were obtained to calculate body mass index (BMI) and height-for-age Z-scores (HAZ), which were calculated with Epi Info, version 3.4.3. One person took all the weight and height measurements, for which the adolescents removed their shoes and wore casual clothing.
2. Questionnaire application. Four questionnaires were applied to each individual. 1. One was to obtain information about individual, familial and social factors such as: exercise (any type of cardiovascular exercise at least three times per week), sleep hours (average sleep hours at night), age, gender, occupation (student, worker and unemployed), social security (with social security, or without social security), type of family (monoparental or biparental family), adolescent's education (number of school years), parents' education (number of school years), type of housing (detached home or apartment), number of residents by household and family history of substance use/abuse. 2. The Alcohol Use Disorders Identification Test (AUDIT) to identify hazardous and harmful drinking,26 validated in Mexican population. 3. The Fargestrom Test for Nicotine Dependence, validated in Mexican population.27 4. The Problem Oriented Screening Instrument for Teenagers (POSIT) that provided information about substance use/abuse, mental health status, family relationships, peer relations, educational status, employment status and aggressive behavior/delinquency.28 The POSIT was standardized and validated in adolescent Mexican population.29,30
3. Clinical neurological examination. In order to determine the current health status of the participants and identify symptoms of neurological impairment, a complete clinical history and neurological examination were performed by pediatric neurologists, including cranial nerve, motor reflexes, coordination and gait, and a sensory exam. The physicians were "blinded" regarding any information on the adolescents' status.
4. Cognitive assessment. The cognitive status included the Full Scale Intelligence Quotient (FSIQ) and the four composed scores known as indexes: Verbal Comprehension (VCI), Perceptual Organizational Index (POI) or Perceptual Reasoning Index (PRI), Working Memory Index (WMI) and Processing Speed Index (PSI). The Wechsler Intelligence Scale for Children (WISC-IV) and the Wechsler Adult Intelligence Scale (WAIS-III),31,32 both standardized and validated in Mexican population, were administered to subjects under 17 and over 17 years of age, respectively. In order to be able to analyze all the data from both tests, the compatible indexes were taken into account: the FSIQ and the four composite scores: VCI, POI in the case of WISC-IV and PRI in the case of WAIS-III; WMI and PSI. Besides, there were not any statistical differences between these two tests. The psychologists were "blinded" regarding any information on the adolescents' status.
5. Lead exposure
5.1. Lead in Blood. Lead in blood was measured once during childhood (CBL), and once during adolescence (ABL). CBL and ABL were measured in the same laboratory with the same methodology. Blood samples were obtained by venipuncture using lead-free "Vacutainer" tubes containing EDTA as an anticoagulant. Lead in blood was analyzed with a matrix modifier of diammonium hydrogenphosphate-Triton X-100 in the presence of 0.2% nitric acid.33 The samples were analyzed with a Perkin-Elmer 3110 atomic absorption spectrophotom-eter, using a graphite furnace. ClinChek whole blood controls were used for internal quality assurance.
5.2. Lead in Bone. Tibia Bone Lead levels (TBL) and Patella Bone Lead concentrations (PBL) were measured at the mid-shaft of the tibia and patella with in vivo X-ray fluorescence. Concentrations were expressed as μg Pb/ g bone mineral. Both legs were measured by one hour. Each leg measurement took 30 minutes and tibia and patella were evaluated simultaneously. A set of bone lead phantoms (lead-doped plaster of Paris) furnished by the National Institute of Standards and Technology (NIST) was used to recalibrate and validate the spectrum analysis. The technique is non-invasive and requires radiation to the subject during measurement.34 When the X-ray signal is low, the masking effect of the Poisson-distributed background frequently produces negative bone lead concentrations. These were expected and observed. To deal with this in our analysis, we dichotomized our bone lead concentrations above and below the median. Measurements were performed in the Centro de Investigación y Capacitación BRIMEX-III, American British Cowdray Medical Center, located in Mexico City (280 miles from the studio area) by trained personnel from the National Institute of Public Health. Therefore, the adolescent and one parent were taken to Mexico City, only for bone lead measure.
Statistical analysis
A descriptive analysis was conducted, followed by bivariate analysis to compare individual, familial, social factors and lead exposure, with health outcomes and health risk behaviors. Because of the results of the bivariate analysis, the nutritional status and substance use/abuse were not considered in the multiple analysis. In the case of nutritional status some indicators were considered like independent variables for cognitive status, because it is well known that nutrition is related with cognitive status.35,36 The Chi-Square test in categorical variables and Pearson's correlation in continuous variables were used. From the variables that had significant association in the bivariate analysis (p<0.05) or approached significance (p>0.05 and p<0.1) and with statistical normality, the construction of multiple logistic and linear regression models were realized according to the type of variable, to find which variables explained the health risk behavior and health outcome in adolescents. In the cognitive status, we included the adolescent education variable, because we had heterogeneous participants from junior high school to college. The Statistical Package for the Social Science version 10.0 (SPSS) was used for statistical analysis. Variables included in the final models are shown in figure 1.
RESULTS
1. Factors
1.1 Individual factors
The sample included 25 females (62.5%) and 15 males (37.5%), aged 12 to 19 years, and all were unmarried. The 75% were students (70% of this group was in high school or more); 15% were workers, and 10% were unemployed. The 62.5% did not exercise regularly (3 times per week), and the 67.5% had a suitable sleep pattern (7 to 9 hours per day).
1.2 Familial factors
Seventy-five percent of the adolescents had a bi-parental family. The percentage of mothers and fathers with high school or more (>12 years of education) was 30% and 40%, respectively. More than 50% of the participants had a family relationship risk and positive family history of substance use/abuse.
1.3 Social factors
In relation to social factors, 57.5% had social security, 62.5% were living in a detached home and the rest in an apartment. All the participants had the same socioeconomic status. More than 50% of the adolescents had a risk peer relation and risk employment status. The mean value of the number of residents by household was 5.1 (SD=1.8).
1.4 Lead exposure
Regarding historical exposure to lead (Childhood Blood Lead), 66.7% of them had blood lead levels (M=13.1, SD=5.8 µg/dL) above the Centers for Disease Control (CDC) reference value of 10 µg/ dL; whereas after analyzing current exposure (M=5.3, SD=1.9 µg/ dL), only 5.0% were above this reference value. However, it is important to note that 55% of the adolescents had blood lead levels above 5µg/dL. Considering Tibia Bone Lead, the 2.5% of the adolescents had levels above the reference value of 10ug lead/g bone mineral, according to the Centro de Investigación y Capacitación BRI-MEX-III, American British Cowdray Medical Center; while measuring Patella Bone Lead, again 2.5% had concentrations above the reference value (15µg lead/g bone mineral).
2. Health Outcomes
All adolescents in the study were reported neurologically healthy by medical clinical examination. Table 1 shows that 7.5% of the adolescents had an iron deficiency by MCV (M=85.58, SD=3.80 fL), but not by Hb (M=15.18, SD=1.50 g/dL). Besides, the 62.5% had an appropriate body mass index. In addition, the 27.5% ate less than three times per day.
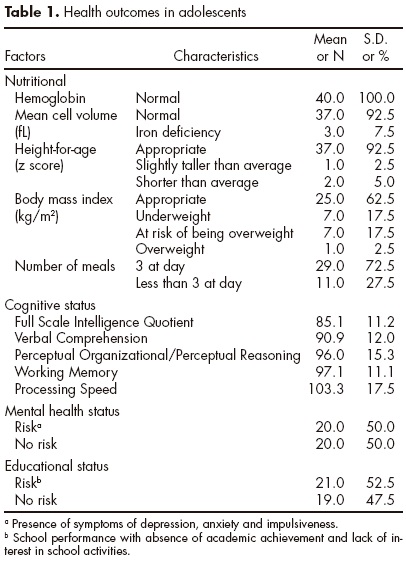
According to POSIT cut-off points, more than 50% of the sample showed risk educational status and risk mental health status (table 1). In the cognitive status, we found that 15.8% of the adolescents were below 70 FSIQ, higher than the expected percentage of 6.7% in the general Mexican population, according to test results.
3. Health risk behaviors
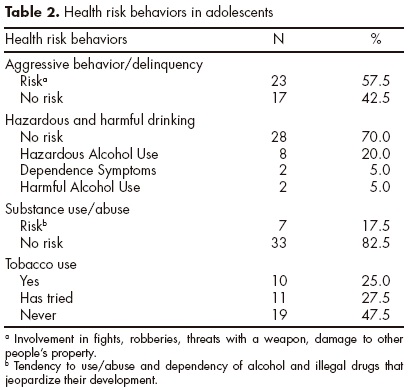
We found that 57.5% of the participants (table 2) showed aggressive behavior/delinquency. One of four participants had positive tobacco use, and the 30% had hazardous and harmful drinking. According to the self-report, none of the participants had used illegal drugs; however, according to the POSIT the 17.5% had risk of substance use/abuse.
4. Factors related to health outcomes and health risk behaviors
Even though the different indexes composed by the FSIQ are highly associated amongst themselves, we found different factors that explain these areas (table 3). For every 1 fL increase in MCV concentration, a 0.97~point increase in FSIQ was found; and for every 1 year increase in the parents' education, an increase of 1.08~points and 1.40~points in FSIQ and POI/PRI was obtained, respectively. The VCI and POI/PRI were associated to a 2.76 and 3.46~point increase, respectively, for every 1-year increase in adolescent education. Whereas, every resident increased in the household and an increase of one hour of sleep were associated to a 2.38 and 5.46 ~point decrease in VCI and PSI, respectively. Adolescents with bi-parental families had a 17.8% higher score in PSI than adolescents with mono-parental families. As for lead exposure, for every 1 ug lead/g bone mineral increased in the tibia and 1 ug/dL increase in blood lead during childhood, the POI/PRI and PSI score decreased by 1.21 and 1.11~points, respectively.
The lack of exercise increases the risk of education status by a factor of 10.78. Risk of mental health status decreases by a factor of 0.08 by being male, and increases by a factor of 8.90 for having a mono-parental family (table 4). The odds of having aggressive behavior/delinquency are decreased by a factor of 0.18 by living in an apartment. For hazardous and harmful drinking, the odds decreased by a factor of 0.08 by not doing exercise; and increased by a factor of 7.17 by having positive family history of substance use/abuse. Finally, the odds of tobacco use is increased by a factor of 12.79 by being male, and decreased by a factor of 0.06 by not having social security.
DISCUSSION
Through this pilot study, we could determine the health status of adolescents that are living in a lead-polluted site. Besides, we could identify a cluster of protective and risk factors that were related to the health status. Five individual variables (exercise, gender, mean cell volume, adolescent's education, and sleep); three familial variables (family history of substance use/abuse, type of family, and father's education); and three social variables (type of housing, number of residents by home and social security) were associated with health outcomes and health risk behaviors. In addition, the childhood blood lead and tibia bone lead (chronic exposure) were risk factors to cognitive status.
Although the clinical neurological examination did not show any problem, the adolescents had issues in other health outcomes, like nutritional status. It was found that 20% of the adolescents had problems with overweight and obesity. This percentage is less than the national prevalence found by the National Survey of Health and Nutrition (ENSANut 2006),37 in the 12 to 19 years of age group, where they reported 32.5% and 31.2 %, in women and men respectively. Also in our sample, we found that 7.5% of the participants had iron deficiencies; this percentage is less than reported (11.5%) by ENSANut in 2006.
We could detect adolescents who were red flags in the cognitive status, since they probably did not have sufficient or efficient cognitive processes for decision-making, which may involve risk behaviors. Even though cognitive status is related to how behavior is produced, and not why it happens (affective and connotative aspects), it has been shown that resilient teenagers have a higher IQ.38 Sleep deprival has been negatively associated to cognitive functions, such as attention span, working memory and executive func-tion,39 and in our results, sleep hours were associated to a 5.46 ~point decrease in PSI.
Several studies have reported an association between blood lead and cognitive issues.5-10,18,40 A previous study in the community of Morales41 found a significant association between blood lead and the sequential factor (p<0.05), an indicator of attention in 41 children (M=7.6, SD=0.8 years); and we found that the chronic lead exposure (TBL) and lead exposure during childhood (CBL) were inversely associated to POI/PRI and PSI, respectively. Therefore, the lead exposure is having influence until adolescence, specifically in this context.
In relation to educational status, physical activity has been positively related to scholastic contentment and academic achievement;42 these findings are consistent with our results. However, other study in Mexico43 found a relation between lead exposure and school failure; in our results, we did not found this association, probably because we studied adolescents (differences between ages) and our blood lead concentrations were lower. Being a student is seen to be a protective factor because school is an important context, which provides experiences for the construction of positive attitudes.44 Furthermore, adolescent education is a predictor of economic status as an adult. Nevertheless, the reality in Mexico is that 15.5% of the adolescents between 10 and 17 years old do not attend school; and 52% of this group stated not having an aptitude for school and had no interest in it.45
Although in our study being male was a protective factor (OR=0.08) for mental health, in other studies being male is a risk factor for risk behaviors like delinquency and exposure to violent acts.19,46
Concerning health risk behaviors, our results show a major prevalence of disorders for consumption of alcohol (30%), compared to the findings of another study, where they used the same instrument (AUDIT). They reported a prevalence of 16.8% in university students between 17 to 19 years of age. On the other hand, also in our sample we found more prevalence for consumption of tobacco (25%) and to have once tried tobacco (27.5%), compared to the findings of the National Survey of Addictions in 2008, which were 8.8% and 14.9% respectively.47,48
Living in an apartment was a protective factor (OR=0.18) for the presence of aggressive behavior/delinquency; probably in this context, due to the existing violence in this zone, living in an apartment generates more safety and reduces the exposure to delinquent criminal acts.
The odds of having hazardous and harmful drinking (OR= 7.17) is increased by having a positive family history of substance use/abuse; these results coincide with other studies.49,50 In addition, the hazardous and harmful drinking is decreased by not exercising (OR=0.08). However, in the educational status, the lack of exercise was a risk factor (OR=10.78); this is a clear example that one protective factor may function for one risk process but not for another.
Being a male was a risk factor (OR=12.79) for the consumption of tobacco in the adolescents of this study. These results coincide with the findings of the National Survey of Addictions in 2008, where 48.8% of those polled (27 million Mexicans) were men who had once tried cigarettes, compared with 23.4% of women.48 Finally, not having social security was a protective factor for the consumption of tobacco (OR=0.06), from what we can deduce that there does not exist a difference between those adolescents who have access to a free health care and those that do not have it, in relation to the prevention of addictions, as this one is the case.
As for the factors of pollution exposure, a decrease of the proportion of individuals with concentrations of lead in their blood greater than 10µg/ dL; from 66.7% in infancy to 5% in adolescence was observed; and only 5% of the population sample had concentrations of lead in tibia and patella over the value of reference. As mentioned earlier, probably the first instance was due to the changes of recreational habits that a child has, in comparison to an adolescent. Besides, interventions started in this site in 1990 (streets were paved, contaminated soil in some areas was removed and the smelter introduced control devices to decrease emissions). Furthermore, a Risk Communication Program in the area was implemented by our group. However, with these concentrations, TBL are having an influence on the cognitive status.
If we compare our concentrations of tibia bone lead with the findings of a study done in adolescents of Mexico City in 1998,51 they found a M=4.8µg Pb/g mineral bone (<1-44.82µg Pb/g); and we found minor concentrations, a M=1.05 µg Pb/g mineral bone (<1-15.47 µg Pb/g). Nevertheless, these numbers should be taken carefully, since there exists a period of 10 years between each study; also in the other study the principal source of contamination was the exposure to vehicular traffic and the consumption of food prepared in lead-glazed pottery.
Even though other studies found an association between lead exposure and aggressive behavior, mental health status and school performance,18,20,22,43 in our results did not find these relations. It is probably due to the fact that the lead concentrations in our sample correspond to the concentrations of the control groups of the other studies. Besides, these associations have been seen in the social contexts of developed countries. Finally, there are differences in participants' ages, instruments used, and sample size.
The next challenge since this follow up pilot study was done is to focus research on a specific protective process that operates in this polluted marginal community, and then, to foster this mechanism, as well as a resilience process through an Integral Program that includes: i) improvement of family cohesion, parents' education, connection to school and educational attainment in the adolescent; ii) promotion of healthy behavior through diet, exercise and sleep patterns; iii) to create a protective mechanism for 60% of the adolescents with a positive family history of substance use/ abuse, to transform it into a resilience factor and iv) continue with Preventive and Risk Communication Programs to control lead exposure, especially in children because they will soon be adolescents.
In this way, we could create opportunities to support the adolescent environment, mainly through the family, peers and social institutions. If we do not resolve the current negative outcomes in this population, these adversities in adult life would represent a continuation of their physical and psychosocial problems; and these problems could create a range of risk experiences that generate other negative outcomes.52,53 In addition, there are many places around the world, and Mexico is not an exception, where lead exposure is still a public health problem.14-17
Research to evaluate the protective and risk mechanisms and total burden of adolescent vulnerability is complex, but necessary, including exposure to environmental pollutants. Research is often focused on a single problem behavior or risk factor, encouraging sweeping generalizations and simplistic solutions. In addition, there are differences between adolescents' concerns regarding adult perceptions on adolescent health. Thus, it is necessary to know of another process, such as adolescent competence in identifying risks.2
It is essential that multidisciplinary experts in adolescent and environmental (pollutants) fields work together to ensure that information generated from research is translated into programs, and for these programs to be implemented and evaluated, and disseminate the findings widely as a result of the aforementioned.
These results should be interpreted cautiously due to various study limitations. Firstly, the sample size was small; however, the complexity and diversity of the interventions make it necessary to study small groups in order to ensure successful results. Secondly, the study design did not allow us to obtain retrospective information on individual, familial and social factors. Thirdly, all written instruments can be used as screening information only.
In conclusion, this follow-up pilot study was an approach to attend adolescents at risk in pollution sites. The results provide information to know where the parents, professors and service providers should focus their efforts in this specific population, through multidisciplinary and integral health programs, which involve the community, family and adolescent. To accept the challenge means working with small samples and simultaneous consideration of all possible multiple factors due to the diversity of the contexts and their complexity. However, there are factors, such as lead exposure, which concern not only adolescents or their families, but political and government policy as well. Finally, it is important to mention that these results are valid only for this specific site, not in other populations. Therefore, it is necessary to validate these results in other contexts.
ACKNOWLEDGEMENTS
This work was supported by a fellowship and grants from Consejo Nacional de Ciencia y Tecnología CONACYT-SALUD-2007-C01-69320. We appreciate the contribution of Raúl Morales-Villegas for his quality control on cognitive assessment, Leticia Carrizales for her technical support and Leticia Yañez for the information regarding lead levels in children.
REFERENCES
1. World Health Organization. Growing in confidence: Programming for adolescent health and development. Ginebra: 2002. [ Links ]
2. Fischhoff B, Nightingale EO, Iannotta J. Adolescent risk and vulnerability: Concepts and measurement. Board on children, youth, and families. Washington, DC: National Academy Press; 2001. [ Links ]
3. Golub MS. Adolescent health and the environment. Environ Health Perspect 2000;108:355-362. [ Links ]
4. Lidsky T, Schneider J. Lead neurotoxicity in children: basic mechanisms and clinical correlates. Brain 2003;126:5-19. [ Links ]
5. Min JY, Min KB, Cho SI, Kim R et al. Neurobehavioral function in children with low blood lead concentrations. Neurotoxicology 2007;28:421-425. [ Links ]
6. Lanphear BP, Dietrich K, Auinger P, Cox C. Cognitive deficits associated with blood lead concentrations <10µg/dL in US Children and Adolescents. Public Health Reports 2000;115:521-529. [ Links ]
7. Stokes L, Letz R, Gerr F, Kolczak M et al. Neurotoxicity in young adults 20 years after childhood exposure to lead: the Bunker Hill experience. Occup Environ Med 1998;55:507-516. [ Links ]
8. White RF, Diamond R, Proctor S, Morey C et al. Residual cognitive deficits 50 years after lead poisoning during childhood. Br J Ind Med 1993;50:613-622. [ Links ]
9. Needleman HL, Schell A, Bellinger D, Leviton A et al. The long-term effects of exposure to low doses of lead in childhood: An 11-year follow-up report. N Engl J Med 1990;322:83-88. [ Links ]
10. Needleman HL, Riess JA, Tobin MJ, Biesecker GE. Bone lead levels and delinquent behavior. JAMA 1996;275:363-369. [ Links ]
11. Dietrich KN, Ris MD, Succop PA, Berger OG et al. Early exposure to lead and juvenile delinquency. Neurotoxicol Teratol 2001;23:511-518. [ Links ]
12. Needleman HL, McFarland C, Ness RB, Fienberg SE et al. Bone lead levels in adjudicated delinquents; a case control study. Neurotoxicol Teratol 2002;24:711-717. [ Links ]
13. Wright JP, Dietrich KN, Ris MD, Hornung RW et al. Association of prenatal and childhood blood lead concentrations with criminal arrests in early adulthood. Plos Medicine 2008;5:732-740. [ Links ]
14. Ornelas M, Sanin LH, Díaz-Barriga F, Reza SA et al. Evaluación de riesgo de intoxicación por plomo en la zona urbana aledaña a una fundidora en Chihuahua, México. Tecnociencia Chihuahua 2007;1:26-33. [ Links ]
15. Ordoñez BR, Ruiz L, Mora R. Investigación epidemiológica sobre niveles de plomo en la población infantil y en el medio ambiente domiciliario de Ciudad Juárez, Chihuahua, en relación con una fundidora de El Paso, Texas. Salud Pública Mex 2003;45:S281-S295. [ Links ]
16. López-Carillo L, Torres-Sánchez L, Garrido F, Papaqui-Hernández J et al. Prevalence and determinants of lead intoxication in Mexican children of low socioeconomic status. Environ Health Perspect 1996;104:1208-1211. [ Links ]
17. Meneses-González F, Richardson V, Lino-González M, Vidal MT. Niveles de plomo en sangre y factores de exposición en niños del estado de Morelos, México. Salud Pública Mex 2003;45:S203-S208. [ Links ]
18. Koller K, Brown T, Spurgeon A, Levy L. Recent developments in low-level lead exposure and intellectual impairment in children. Environ Health Perspect 2004;112:987-994. [ Links ]
19. Lipsey MW, Derzon JH. Predictors of violent or serious delinquency in adolescence and early adulthood. In: Loeber R, Farrington DP (eds). Serious and violent juvenile effenders: risk factors and successful interventions. Thousand Oaks, CA: Sage Publications; 1998. [ Links ]
20. Rutter M. Resilience: Some conceptual considerations. J Adolesc Health 1993;14:626-631. [ Links ]
21. Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychology Review 1979;84:191-215. [ Links ]
22. Kotliarenco MA, Cáceres I, Fontecilla M. Estado de arte en resiliencia. Organización Panamericana de la Salud; 1997. [ Links ]
23. Díaz-Barriga F, Santos MA, Mejía JJ, Batres L et al. Arsenic and cadmium absorption in children living near a smelter complex in San Luis Potosí, Mexico. Environ Res 1993;62:242-250. [ Links ]
24. Carrizales L, Razo I, Téllez-Hernández JI, Torres-Nerio R et al. Exposure to arsenic and lead of children living near a copper-smelter in San Luis Potosi, Mexico: Importance of soil contamination for exposure of children. Environ Res 2006;101:1-10. [ Links ]
25. Gibson RS. Principles of nutritional assessment. New York: Oxford University Press; 1990. [ Links ]
26. Medina-Mora E, Carreno S, De la Fuente JR. Experience with the Alcohol Use Disorders Identification Test (AUDIT) in Mexico. In: Galanter (ed). The consequences of alcoholism. New York: Plenum Press; 1998. [ Links ]
27. Norma Oficial Mexicana NOM-028SSSA2-1999, para la prevención, tratamiento y control de las adicciones. México: 1999. [ Links ]
28. Latimer W, Winters K, Stinchfield R. Screening for drug abuse among adolescents in clinical and correctional settings using the problem-oriented screening instrument for teenagers. Am J Drug Alcohol Abuse 1997;23:79-98. [ Links ]
29. Mariño M, González-Forteza C, Andrade P, Medina-Mora ME. Validación de un cuestionario para detectar adolescentes con problemas por el uso de drogas. Salud Mental 1998;21:27-36. [ Links ]
30. Mariño M, González-Forteza C, Medina-Mora ME. Detección de adolescentes mexicanos con problemas en siete diferentes áreas de vida. Psicopatología 1999;19:125-128. [ Links ]
31. Wechsler D. Escala Wechsler de Inteligencia para niños-IV: Manual de aplicación/Wechsler D. México: Manual Moderno; 2007. [ Links ]
32. Wechsler D. Escala Wechsler de Inteligencia III. México: Manual Moderno; 2001. [ Links ]
33. Subramaninan KS. Determination of lead in blood: Comparison of two GFAAS methods. At Spectrosc 1987;8:7-14. [ Links ]
34. Hoppin JA, Aro A, Hu H, Ryan PB. In vivo bone lead measurement in suburban teenagers. Pediatrics 1997;100:365-370. [ Links ]
35. Pollitt E, Hathirat P, Ktchabhakdi NJ, Missel L et al. Iron deficiency and educational achievement in Thailand. Am J Clin Nutr 1989;50:687S-696S. [ Links ]
36. Soewondo S, Husaini M, Pollit E. Effects of iron deficiency on attention and learning processes in preschool children: Bandung, Indonesia. Am J Clin Nutr 1989;50:667S-673S. [ Links ]
37. Secretaría de Salud, Instituto Nacional de Salud Pública. Encuesta Nacional de Salud y Nutrición 2006. México: 2006. [ Links ]
38. Fergusson DM, Lynskey MT. Adolescent resiliency to family adversity. J Child Psychol Psychiat 1996;37:281-292. [ Links ]
39. Valdez P, Reilly T, Waterhouse J. Rhythms of mental performance. Mind Brain Education 2008;2:7-16. [ Links ]
40. Lanphear BP, Homung R, Khoury J, Yolton K et al. Low-level environmental lead exposure and children's intellectual function: An international pooled analysis. Environ Health Perspect 2005;113:894-899. [ Links ]
41. Calderón J, Navarro ME, Jimenez-Capdeville ME, Santos-Díaz MA et al. Exposure to arsenic and lead and neuropsychological development in Mexican children. Environ Res 2001;85:69-76. [ Links ]
42. Kristjánsson AL, Sigfúsdóttir ID, Allegrante JP, Helgason AR. Adolescent health behavior, contentment in school, and academic achievement. Am J Health Behav 2009;33:69-79. [ Links ]
43. Leal-Escalante CR, Baltazar-Reyes MC, Lino-González M, Palazuelos-Rendón E et al. Concentraciones de plomo en sangre y reprobación de escolares en la ciudad de México. Gac Méd Méx 2007;143:377-381. [ Links ]
44. Robles F, Rodríguez E, Medina-Mora ME, Villatoro J et al. Resultados definitivos: Informe ejecutivo. México: DIF, UNICEF, PNUFID; 1999. [ Links ]
45. Instituto Nacional de Estadística y Geografía (INEGI). Resultados del módulo de trabajo infantil 2007. Encuesta Nacional de Ocupación y Empleo 2007. México: INEGI; 2008. [ Links ]
46. Zavaschi ML, Benetti S, Polanczyk G, Solés N et al. Adolescents exposed to physical violence in the community: a survey in Brazilian public schools. Rev Panam Salud Publica 2002;12:327-332. [ Links ]
47. Díaz A, Díaz R, Hernández-Avila C, Narro J et al. Prevalencia del consumo riesgoso y dañino de alcohol y factores de riesgo en estudiantes universitarios de primer ingreso. Rev Salud Mental 2008;31:271-282. [ Links ]
48. Secretaría de Salud, Secretariado Técnico del Consejo Nacional Contra las Adicciones, Instituto Nacional de Salud Pública, Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz. Encuesta Nacional de Adicciones 2008. México: 2008. [ Links ]
49. Florenzano U. Adicciones, consumo de sustancias y factores de riesgo. In: Martínez G, Menenghello (eds). Psiquiatría y psicología de la infancia y adolescencia. Argentina: Médica Panamericana; 2000. [ Links ]
50. Medina-Mora ME, Natera G, Borges G, Cravioto P et al. Del siglo XX al tercer milenio. Las adicciones y la salud pública: drogas, alcohol y sociedad. Salud Mental 2001;24:3-19. [ Links ]
51. Farias P, Hu H, Rubenstein E, Meneses-González F et al. Determinants of boné and blood lead levels among teenagers living in urban areas with high lead exposure. Environ Health Perspect 1998;106:733-737. [ Links ]
52. Bellinger D. Lead. Pediatrics 2004;113:1016-1022. [ Links ]
53. Chen A, Cai B, Dietrich KN, Radcliffe J et al. Lead exposure, IQ, and behavior in urban 5 to 7 year old: does lead affect behavior only by lowering IQ? Pediatrics 2007;119:650-658. [ Links ]














