Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Salud mental
versão impressa ISSN 0185-3325
Salud Ment vol.34 no.5 México Set./Out. 2011
Artículo original
Autistic spectrum disorders: Diagnostic and therapeutic challenges in Mexico
Trastornos del espectro autista: retos diagnósticos y terapéuticos en el contexto de México
María Elena Márquez–Caraveo,1 Lilia Albores–Gallo1
1 Hospital Psiquiátrico Infantil Dr. Juan N. Navarro.
Correspondence:
Dra. María Elena Márquez–Caraveo.
Av. San Buenaventura 86, col. Belisario Domínguez, Tlalpan, 14080, México, D F. Tel. 5485–4370,
E mail: marquezmalena@yahoo.com.mx
ABSTRACT
Autistic Spectrum Disorders (ASD) are developmental disorders with impairments in three broad domains: social interaction, communication and stereotypic movements and repetitive behavior. Their symptoms are complex, bizarre and most of them persistent, causing maladaptive and poor psychosocial adjustment.
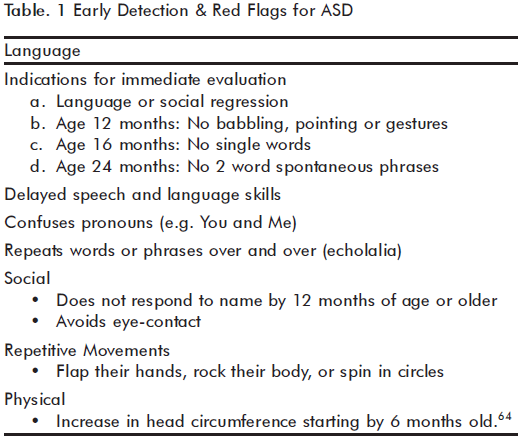
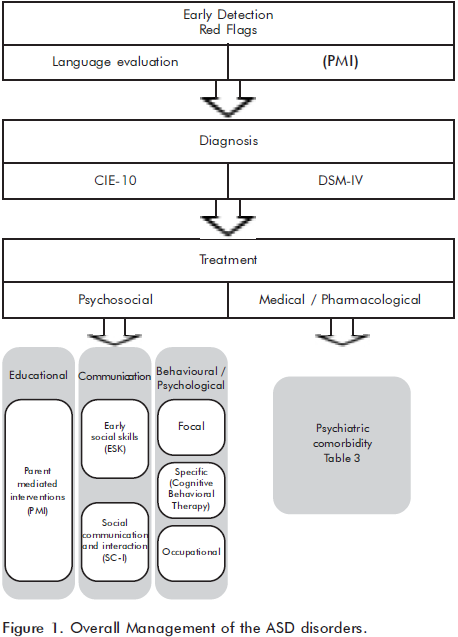
Early detection and diagnosis is a priority in ASD, parents are the first to notice early autism symptoms: 50% observe signs in the first 12 months of age. Despite initial observations of atypical development, there are significant delays in seeking proper medical attention and correct diagnosis; less than 38% of families receive their diagnosis through health services. Educational and health primary care providers need training in developmental milestones with focus on language and socio–communicative domains. Health policy planners should facilitate rationale referral when key symptoms such as language alterations are detected. The use of valid instruments and surveillance approaches versus awareness through red flag symptoms is discussed.
Psychosocial interventions are the most important treatment, with ABA and TEACHH techniques recommended; pharmacological treatment (atypical antipsychotics, antidepressants, drugs for hyperactivity, sleep problems and anxiety) must be directed to treat comorbid conditions and combined with behavioral interventions.
Key words: Autistic disorders, treatment, psychosocial interventions, pharmacological therapy, Mexico.
RESUMEN
Los trastornos del espectro autista (TEA) son trastornos del desarrollo con alteración en tres dominios: interacción social, comunicación y conductas repetitivas o movimientos estereotipados. Los síntomas son complejos, bizarros y la mayoría persistentes y causan un pobre ajuste psicosocial. La detección y diagnóstico tempranos son prioridad en los TEA; los padres son los primeros en advertir los síntomas tempranos del autismo: 50% observan manifestaciones en los primeros doce meses de edad. A pesar de las observaciones tempranas del desarrollo atípico, existen atrasos en la búsqueda de atención médica apropiada. Los proveedores de servicios educativos y cuidados primarios en salud necesitan adiestramiento en los hitos del desarrollo enfocados en el lenguaje y dominios sociocomunicativos.
Se discute el uso de instrumentos y protocolos de abordaje frente a programas sobre advertencia de los síntomas de alarma. Las intervenciones médicas y psicosociales se describen de acuerdo con un abordaje de manejo integral. Las intervenciones psicosociales son las más importantes, en particular el empleo de los programas conocidos como ABA y TEACHH. El tratamiento farmacológico debe combinarse con intervenciones conductuales y utilizarse para el manejo de la comorbilidad.
Palabras clave: Trastornos autistas, tratamiento, intervenciones psicosociales, tratamiento farmacológico, México.
INTRODUCTION
Autism is classified in the Pervasive Developmental Disorders category according to ICD–101 and DSM–IV.2 The term ASD (autism spectrum disorders) was proposed by Lorna Wing3 to cover a spectrum ranging from severe autism with profound mental retardation to high functioning autism. Therefore, ASD definition in this article will include: autism (infantile and atypical), Asperger's syndrome/disorder and pervasive developmental disorders not otherwise specified (PDD–NOS).
These complex developmental disorders are defined by a triad of impairments in reciprocal social interaction, communication and the presence of repetitive or overly restricted behaviors.
ASD have a high level of comorbidity with intellectual and learning disabilities. The underlying deficit of ASD has been related to social cognition processes such as joint attention. This term defines the individual's early ability to coordinate attention between a social partner and an object or event.4–7
This impairment has been assumed as an explanation for the triad of ASD symptoms.8 Communication failures include difficulties in expressive and pragmatic abilities. Children with ASD have problems understanding rules of communicative exchange and the meaning of nonverbal language. These deficits increase social withdrawal and atypical social and playing skills behavior. Stereotypical behaviors are observed in repetitive motor acts, ritualistic behavior and exaggerated interest in parts of objects. Children with ASD have key symptoms that may be unrecognized by primary care providers, and even specialized professionals may lack the skills and expertise to properly diagnose and help these children. Service delivery is needed in both directions, it is urgent to provide evidence–based and cost–effective interventions. The overall management implies a combined approach of medical, psychological, educational and social interventions.9 Whilst doctors may be prone to emphasize pharmacological treatments, psychologists and educators often prefer psychosocial interventions. This paper focuses on an update of evidence based recommendations for the diagnosis and treatment of ASD conditions.
EARLY DETECTION AND DIAGNOSIS
Parents are the first to notice early autism manifestations: 50% observe signs in the first 12 months,10 while 83.3% have concerns before age 2.11 Despite these initial observations of atypical development, there are still significant delays in seeking proper medical attention (mean delay: 22–32 months) and correct diagnosis (mean age: 53 months).12–14 Health and educational services play a crucial role in recognition and diagnosis of ASD.
In Spain, less than 38% of families receive their diagnosis through health services.12 In Bogota, up to 39% of referrals for autism is done by non–health or educational professionals mostly parents, friends or others.15 In the same line, many children (40%) are identified in school settings.16
Although the development of measures to assess the ASD in the last two decades has augmented, the cost of using these tools has increased significantly.17 Many of these instruments are very complex and are targeted to highly specialized professionals with experience in autism, so their use in the primary care setting is not feasible.18 Furthermore, some of them require training and take enormous time to administrate and rate.19,20 There are some screening and diagnostic measures available in Mexico with reported psychometric properties,21,22 but their systematic use in an autism surveillance program is still controversial, because no studies about their cost–effectiveness have been conducted.19,23
Some researchers propose that screening should be oriented to children at risk like probands' siblings, children with low gestational age and/or weight, or children whose parents have developmental concerns.19 The use of key symptoms (red flags)24 for referral to child psychiatrist or clinical psychologist could be a more cost–effective strategy than screening instruments.25–27
Autism has a wide range of symptom presentations that can sometimes overlap with other developmental disabilities and communication disorders. Stigma associated with mental disorder bias the referral process and milder diagnosis such as expressive language delays or late language emergence are considered before autism. Therefore, it is important to raise awareness of abnormal language and social deviant development as key symptoms of autism among parents, family doctors and pediatricians. Head circumference should also be measured28,29 (table 1). There is enough evidence that early intensive intervention provides family support and improves outcome.30,31 Early detection should be followed by a rigorous assessment to confirm the diagnosis and evaluate the general functioning level of referred children and adolescents. Mexican researchers need to develop valid and reliable gold standard measures which can be used in busy settings with minimal training requirements.
Overall management includes early detection, diagnostic evaluation, psychosocial intervention and medical pharmacological treatment. This perspective is proposed in figure 1.
TREATMENT
According to recent guidelines,32 most of the interventions should be supported by systematic reviews or RCTs (Randomized Control Trials) when evidence is available, because many alternative medicine treatments commonly used are not evidence based.33,34
Psychosocial treatment
Psychosocial treatment begins with the appropriate education, which has had the greatest positive impact for ASD children in the last 50 years by reducing long stay treatments.
Current approaches include home and school based programs requiring parents and teachers as mediators to promote structured activities. Enrollment in these programs is recommended at an early age (2–3 years).35
The interventions and treatment methods for children with ASD include two approaches:36,37 Applied Behavioral Analysis (ABA) and the Treatment and Education of Autistic and related Communication–handicapped Children (TEACCH).
1. Applied Behavioral Analysis (ABA)
It is based on conditional operant theory to teach communication, play, social, academic, self–care, work, and community living skills, and to reduce disruptive behaviors in children with autism. This behavioral model proposed by Lovaas38,39 requires an average of 30 to 40 hours sessions per week of one–to–one instruction. The program is administered by trained certified therapists and parents at home and school settings.
The Early Start Denver Model (ESDM),40 based on ABA approach, was designed to address the needs of toddlers with ASD as young as 12 months. It is a comprehensive early behavioral intervention for infants to preschool–aged children with ASD that integrates ABA with developmental and relationship–based approaches.
A recent randomized, controlled trial study with ESDM41 intervention showed a shift in diagnosis from autism to PDD–NOS. The outcomes of this study involved an increase in IQ scores of 17 points (>1 SD) and significant gains in language and adaptive behavior.
ABA methods use discrete trial training (DTT) and incidental teaching (IT).
DTT consists of a basic four step process to teach:
a. A short verbal command or request or physical stimulus. For example: «Match colors» or «Show me blue».
b. Prompt stimulus. A prompt cue from the therapist to help the child respond correctly.
c. Response: resulting behavior, which can be a response or lack of response.
d. A consequence, which depends on the behavioral response; may include positive reinforcement of the desired behavior, or no reaction for the incorrect response.
IT focuses on teaching whenever the child shows interest in the teaching materials or activities in the natural environment. It is less structured than the DTT and allows the child to lead his/her interests and the teaching processes.42
2. The Treatment and Education of Autistic and related Communication–handicapped Children (TEACCH)43 program
It was developed by Eric Schopler and colleagues at the University of North Carolina.42 This approach is focused on modifying the environment to meet the individualized needs of children with autism. The four general components of TEACCH program are: physical organization and structure, daily schedules, work systems and task structure.
The purpose is to build a repertoire of social behaviors and communication methods through visual, verbal and tactile clues. The program aims to motivate direct learning and involvement in emotional experiences that take place in every day settings to observe the active learning and social participation of children.
Currently, a combination of ABA and TEACCH approaches is recommended;43 their use has showed significant IQ gains,44 leading children incorporation to regular classrooms.
Other interventions are:
a. Communication interventions include strategies designed by speech and language therapists.32,43 Their aim is to develop and enhance early communication skills, social communication and interaction. Modification of the communicative, social and physical environment through the use of visual prompts, routine and timetabling is recommended to minimize sensory sensitivity and complex social interactions.
b. Behavioral/psychological interventions include what was previously called behavioral management and is now identified as Positive Behavior Support Systems.45 The method requires identification of environmental contingencies to focus on the positive aspects of the environment and the child behavior. The focal interventions are designed to reduce symptom frequency and severity of specific problematic behaviors such as aggression or self injury. This approach helps the development of adaptive skills. At present, the specific psychological intervention includes Cognitive Behavior Therapy (CBT), feasible in children with ASD who have a verbal IQ of at least 69. Children with social difficulties or with co–occurring depression and/or anxiety can benefit from this approach.46
c. Interventions such as occupational47 and vocational support may aid children with ASD to prepare and adapt to future employment environments. Good workplace practices and proper work conduct such as timelines and understanding the concept of others privacy can be developed in adolescents with ASD.
The focus of psychosocial interventions is summarized in table 2.
Individualized treatment is indicated given the heterogeneous presentation of ASD.
Pharmacological treatment
Family feedback regarding the etiology, diagnosis and prognosis is combined with the transient use of drugs indicated to deal with psychiatric comorbidity48 and/or epilepsy. Medical/pharmacological management should be used as a component of a multidisciplinary care approach.49
There are some general principles regarding medication treatment assessment of the child's home and school environment; routines in meals, daily activities, and sleep are crucial as changes in these domains are worth attempting before using medication.
In fact, there are few drugs specifically approved for use in children and adolescents with ASD. Pharmacological treatment for ASD should only be undertaken by physicians with appropriate training. It is important to define the target symptoms before medication and to measure any side effect.
Currently, there is no drug with a specific ameliorative effect on autism. Medication is a short– to medium–term intervention for symptoms such as self–aggression, irritability, hyperactivity, insomnia and anxiety; details are presented in table 3.
At present, risperidone is indicated for symptoms such as irritability, aggression and repetitive behavior,50 but weight gain and metabolic syndrome must be identified as an adverse effect.51,52 Methylphenidate may be considered for attention difficulties and hyperactivity in children or young people with ASD;53 side effects as insomnia and weight loss should be carefully monitored.
Melatonin54,55 and clonidine56,57 had been suggested for the treatment of persistent sleep problems, resistant to behavioral interventions. Anxiety can be ameliorated with fluvoxamine58,59 or buspirone.60 We recommend to review the guidelines for epilepsy treatment.61,62
CONCLUSIONS
There are still many challenges that Mexico should meet to provide comprehensive management for children with ASD and their families, which are described as follows:
1. The exact number of people with these disabilities is unknown; epidemiological research would allow better planning of health, educational and social services for this population.
2. There is an urgent need to raise awareness of ASD disorders in the community. Previous studies have shown that at least two key symptoms (stares at nothing and abnormal language) are easily recognized by the parents as reasons for seeking medical help.63
3. It is also important to train health and educative services providers in developmental milestones with focus on language, social and communication domains in order to increase the early detection of ASD.
4. Medical assessment could be combined with the evaluation of functioning, as well as context barriers and facilitators.
5. Training in ABA and TEACCH techniques for professionals (psychologists, therapists, special education teachers, etc.) working in health and educational public institutions is highly recomended.
REFERENCES
1. World Health Organization. ICD–10: International Statistical Classification of Diseases and Related Health Problems: 10th revision. Geneva; 2007. [ Links ]
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth edition, text revision. Washington; 2000. [ Links ]
3. Wing L. The autistic spectrum. The Lancet 1997; 350:1761–1776. Available at: http://www.thelancet.com/search/results?fieldName=Authors&searchTerm=Lorna+Wing. Access date: June 29; 2011. [ Links ]
4. Scaife M, Bruner J. The capacity for joint visual attention in the infant. Nature 1975;253:265–266. [ Links ]
5. Bakeman R, Adamson LB. Coordinating attention to people and objects in mother–infant and peer–infant interaction. Child Dev 1984;55:1278–1289. [ Links ]
6. Mundy P, Sigman M, Kasari C. Joint attention, developmental level, and symptom presentation in young children with autism. Dev Psychopathol 1994;6:389–401. [ Links ]
7. Mundy P, Thorp D. Atención conjunta y autismo: Teoría, evaluación y neurodesarrollo. En: Asociación de padres de personas con autismo (APNA). Nuevos desarrollos en autismo: el futuro es hoy. Madrid: Gráficas Áreas Montano, S.A; 2005; pp. 123–169. [ Links ]
8. Mundy P, Sigmanm M, Ungerer J, Sherman T. Deûning the social deûcits of autism: The contribution of nonverbal communication measures. J Child Psychol Psychiatry 1986;27:657–669. [ Links ]
9. Reiss AL. Childhood developmental disorders: an academic and clinical convergence point for psychiatry, neurology, psychology and pediatrics. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19220592 Access date: April 01; 2011. [ Links ]
10. Kishore MT, Basu A. Early concerns of mothers of children later diagnosed with autism: Implications for early identiûcation. Res Autism Spectr Disord 2011;5:157–163. [ Links ]
11. Jónnsdóttir S, Saemundsen E, Antonsdóttir IS, Sigurdardóttir S et al. Children diagnosed with autism spectrum disorder before or after the age of 6 years. Res Autism Spectr Disord 2001;5:175–184. [ Links ]
12. Confederación de Autismo España e Instituto de Investigación de Enfermedades Raras (IIER). Informe sobre demora en el diagnostico en los TEA. Available at: www.isciii.es/htdocs/centros/enfermedadesraras/pdf/aut_isdd2.pdf Access date: April 01; 2011. [ Links ]
13. Chakrabarti S. Early identiûcation of autism. Indian Pediatr 2009;4:412–414. [ Links ]
14. Rice C, Nicholas J, Baio J, Pettygrove S et al. Changes in autism spectrum disorder prevalence in 4 areas of the United States. Disabil Health J 2010;3:186–201. [ Links ]
15. Talero–Gutiérrez C, Rodríguez M, De la Rosa D, Morales G et al. Caracterización de niños y adolescente con trastornos del espectro autista en una institución de Bogotá, Colombia. Neurología 2011. Available at: https://docs.google.com/viewer?url=http://www.elsevier.es/sites/default/files/elsevier/eop/S0213–4853%2811%2900139–3.pdf&embedded=true&chrome=true. Access date: June 28; 2011. [ Links ]
16. Yeargin–Allsopp M, Rice C, Karapurkar T, Doernberg N et al. Prevalence of autism in a US metropolitan area. JAMA 2003; 289:49–55. [ Links ]
17. Bishop D. University of Oxford. How to choose between diagnostic tools? Discussion: a plea for efficiency. Available at: http://psyweb.psy.ox.ac.uk/oscci/ Access date: June 01; 2011. [ Links ]
18. Albores–Gallo L, Hernández–Guzmán L, Díaz–Pichardo JA, Cortés–Hernández B. Dificultades en la evaluación y diagnóstico del autismo. Una discusión. Salud Mental 2008;31:37–44. [ Links ]
19. Matson JL, Rieske RD, Tureck K. Additional considerations for the early detection and diagnosis in autism: Review of available instruments. Res Autism Spectr Disord 2011;5:1319–1326. [ Links ]
20. Akshoomoff N, Corsello C, Schmidt H. The role of the autism diagnostic observation schedule in the assessment of autism spectrum disorders in school and community settings. Calif School Psychol 2006;11:7–19. [ Links ]
21. Hedley D, Young R, Angelica M, Gallegos J et al. Cross–cultural evaluation of the Autism Detection in Early Childhood (ADEC) in Mexico. Autism 2010;14:93–112. [ Links ]
22. Albores–Gallo L, Roldan Ceballos O, Hernández–Guzmán L, Villarreal–Valdés G et al. Validity of M–CHAT in a large ASD sample. International Society for Autism Research: 11th International Meeting for Autism Research (IMFAR). San Diego California May 11–13: New research poster #128; p.122. [ Links ]
23. Al–Qabandi M, Gorter JW, Rosenbaum P. Early autism detection: Are we ready for routine screening? Pediatrics 2011;10:1–7. [ Links ]
24. Wong V, Hui L, Lee W, Leung L et al. A modified screening tool for autism (Checklist for Autism in Toddlers [CHAT–23]) for Chinese Children. Pediatrics 2004;114:166–176. [ Links ]
25. Aylward GP. Conceptual issues in developmental screening and assessment. J Dev Behav Pediatr 1997;18:240–249. [ Links ]
26. Baron–Cohen S, Cox A, Baird G, Swettenham J et al. Psychological markers in the detection of autism in infancy in a large population. Br J Psychiatry 1996;168:158–163. [ Links ]
27. Perera H, Wijewardena K, Aluthwelagem R. Screening of 18–24–month–old children for autism in a semi–urban community in Sri Lanka. J Trop Pediatr 2009;55:402–405. [ Links ]
28. Sacco R, Militerni R, Frolli A, Bravaccio C et al. Clinical, morphological, and biochemical correlates of head circumference in autism. Biol Psychiatry 2007;62:1038–1047. [ Links ]
29. Bertoglio K, Hendren R. Research: New developments in autism. Psychiatr Clin N Am 2009;32:1–14. [ Links ]
30. Dawson G, Rogers S, Munson J, Smith M et al. Randomized, controlled trial of an intervention for toddlers with autism: the early start denver model. Pediatrics 2010;125:17–23. [ Links ]
31. Howlin P, Magiati I, Charman T. Systematic review of early intensive behavioral interventions for children with autism. Am J Intellect Dev Disabil 2009;114:23–41. [ Links ]
32. Scottish Intercollegiate Guidelines Network (SIGN). [Online] 2007. Available at: http://www.sign.ac.uk/new.html Access date: April 01; 2011. [ Links ]
33. Levy SE, Mandell DS, Schultz RT. Autism. Lancet 2009;374:1627–1638. [ Links ]
34. Seida JK, Ospina MB, Karkhaneh M, Hartling L et al. Systematic reviews of psychosocial interventions for autism: An umbrella review. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19191842 Access date: April 01; 2011. [ Links ]
35. Rogers SJ, Vismara LA. Evidence–based comprehensive treatments for early autism. J Clin Child Adolesc Psychol 2008;37:8–38. [ Links ]
36. Jordan R, Jones G, Murray D. Educational interventions for children with autism: A literature review of recent and current research. Available at: https://www.education.gov.uk/publications/eOrderingDownload/RB77.pdf Access date: April 01; 2011. [ Links ]
37. Diggle T, McConachie HR. Parent–mediated early intervention for young children with autism spectrum disorder. UK: John Wiley & Sons; 2009; pp. 1–30. [ Links ]
38. Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. J Consult Clin Psychol 1987;55:3–9. [ Links ]
39. Basset K, Green CJ, Dazanjian A. Autism and Lovaas treatment: A systematic review of effectiveness evidence available at: http://www.chspr.ubc.ca/node/351. Access date: April 01; 2009. [ Links ]
40. Dawson G. Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Dev Psychopathol 2008;20:775–803. [ Links ]
41. Smith M, Rogers S, Dawson G. The Early Start Denver Model: a comprehensive early intervention approach for toddlers with autism. En: Handleman JS, Harris SL (eds). Pre–school education programs for children with autism. Austin: Pro–Ed Corporation, Inc. 2008:65–101. [ Links ]
42. Ringdahl J, Kopelman T, Falcomata TS. Chapter 2. Applied behavior analysis and its application to autism and autism related disorders. In: Matson JL. Applied behavior analysis for children with autism spectrum disorders. New York: Springer; 2009; pp. 15–32. [ Links ]
43. Ospina MB, Seida JK, Clark B, Karkhaneh M et al. Behavioural and developmental interventions for autism spectrum disorder: A clinical systematic review. PLoS ONE 2008;3:3755. [ Links ]
44. Myers SM, Johnson CP. Management of children with autism spectrum disorders. Pediatrics 2007;120:1162–1182. [ Links ]
45. Carr EG, Dunlao G, Horner RH, Koegel RL et al. Positive behavior support: Evolution of a applied science. J Positive Behavior Interventions 2002;4:4–16. [ Links ]
46. White AH. Cognitive behavioural therapy in children with autistic spectrum disorder. En: Bazian LTD (ed). STEER: Succinct and timely evaluated evidence reviews. London: Bazian Ltd and Wessex Institue for Health Research and Development; 2004. [ Links ]
47. Case–Smith J, Arbesman M. Evidence–based review of interventions for autism used in or of relevance to occupational therapy. Am J Occup Ther 2008;62:416–429. [ Links ]
48. Simonoff E, Pickles A, Charman T, Chandler S et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity and associated factors in a population–derived sample. J Am Acad Child Adolesc Psychiatry 2008;47:921–929. [ Links ]
49. West L, Waldrop J, Brunssen, S. Pharmacologic treatment for the core deficits and associated symptoms of autism in children. J Pediatr Health Care 2009;23:75–89. [ Links ]
50. Posey DJ, Erickson CA, McDougle CJ. Antipsychotics in the treatment of autism. UK. J Clinic Invest 2008;118:6–14. [ Links ]
51. Jesner OS, Aref–Adid M, Coren E. Risperidona para el trastorno del espectro autista. Oxford: John Wiley & Sons; 2008. [ Links ]
52. Malone R, Waheed A. The role of antipsychotics in the management of behavioral symptoms in children and adolescents with autism. Drugs 2009;6:535–548. [ Links ]
53. Reiersen AM, Todd RD. Co–occurrence of ADHD and autism spectrum disorders: phenomenology and treatment. Expert Rev Neurother 2008;8: 657–669. [ Links ]
54. Wirojanan J, Jacquemont S, Diaz R, Bacalman S et al. The efficacy of melatonin for sleep problems in children with autism, fragile X syndrome, or autism and fragile X syndrome. J Clin Sleep Med 2009;5:145–150. [ Links ]
55. Wasdell MB, Jan JE, Bomben MM, Freeman RD et al. A randomized, placebo–controlled trial of controlled release melatonin treatment of delayed sleep phase syndrome and impaired sleep maintenance in children with neurodevelomental disabilities. J Pineal Res 2008;44:57–64. [ Links ]
56. Jaselskis CA, Cook EH, Fletcher KE, Leventhal BL. Clonidine treatment of hyperactive and impulsive children with autistic disorder. J Clin Psychopharmacol 1992;12:322–327. [ Links ]
57. Fankhauser MP, Karumanchi VC, German ML et al. Double–blind, placebo–controlled study of the efficacy of transdermal clonidine in autism. J Clin Psychiatry 1992;53:77–82. [ Links ]
58. Walkup JT, Labellarte MJ, Riddle MA, Pine DS et al. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl Med 2001;344:1279–1285. [ Links ]
59. Kolevzon A, Mathewson KA, Hollander E. Selective Serotonin reuptake inhibitors in autism: a review of efficacy and tolerability. J Clin Psychiatry 2006;67:14–407. [ Links ]
60. Buitelaar JK, van der Gaag RJ, van der Hoeven J. Buspirone in the management of anxiety and irritability in children with pervasive developmental disorders: results of an open–label study. J Clin Psychiatry 1998;59:56–59. [ Links ]
61. Alonso M, Estañol B, Garza S, Gavito J et al. Epilepsia. Primera edición. México: Programa Prioritario de Epilepsia; 2007. [ Links ]
62. Scottish Intercollegiate Guidelines Network SIGN 81. Diagnosis and management of epilepsies in children and young people. Available at: http://www.sign.ac.uk/new.html Access date: April 01; 2011. [ Links ]
63. Caraveo–Anduaga JJ, Colmenares–Bermudez E, Martínez–Vélez NA. Síntomas, percepción y demanda de atención en salud mental en niños y adolescentes de la Ciudad de México. Salud Publica de México 2004;44: 492–498. [ Links ]
Nota
Editores invitados: Rosa Elena Ulloa Flores, Francisco de la Peña Olvera, Lino Palacios Cruz.














