Serviços Personalizados
Journal
Artigo
Indicadores
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Salud mental
versão impressa ISSN 0185-3325
Salud Ment vol.33 no.5 México Set./Out. 2010
Artículo original
Retention rates and potential predictors in a longitudinal randomized control trial to prevent postpartum depression
Tasas de retención y variables que la predicen en un estudio aleatorio controlado longitudinal para prevenir la depresión posparto
Ma. Asunción Lara,1 Claudia Navarro,1 Laura Navarrete,1 Huynh-Nhu Le2
1 Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz.
2 The George Washington University, Washington DC
Correspondencia:
Dra. Ma. Asunción Lara.
Instituto Nacional de Psiquiatría Ramón de la Fuente.
Calzada México-Xochi mi lco 101. San Lorenzo Huipulco,
Tlalpan. 1 4370, México, DF
Tel: (55) 4160 5170. Fax: (55) 5655 7999.
E-mail: laracan@imp.edu.mx
Recibido primera versión: 9 de noviembre de 2009.
Segunda versión: 23 de marzo de 2010.
Aceptado: 18 de mayo de 2010.
Abstract
Perinatal depression is increasingly recognized as a significant public mental health problem; consequently, there is a major interest in developing strategies to prevent postpartum depression that may help reduce its detrimental consequences. However, the unique experiences associated with the perinatal period make it more difficult to recruit participants at this stage and to retain them over time when assessing prevention interventions. The aim of the study is to examine retention rates and predictors of retention in a longitudinal, randomized controlled trial (RCT) to prevent postnatal depression.
Method
Participants: Pregnant women (N = 377) at risk of depression were randomized to intervention or usual care condition and assessed during pregnancy and at 6 weeks and 4-6 months postpartum.
Intervention: The intervention was designed by modifying a previously evaluated one and includes information on normal pregnancy and the postpartum period, from psychoanalytic and risk factors perspectives. It attempts to reduce depression levels by increasing positive thinking and pleasant activities, improving self-esteem, increasing self-care, learning skills to strengthen social support, and exploring unrealistic expectations about pregnancy and motherhood. It is delivered in eight two-hour weekly group sessions during pregnancy.
Measures: Depressive symptoms were measured using the second edition of the Beck Depression Inventory (BDI-II); anxiety symptoms with the corresponding subscale of the Hopkins Symptoms Checklist (SCL-90) and social support with the Social Support Apgar (SSA). A short form of 12 items representing potential stressors was used as a measurement of stressful life events and the Abbreviated Version of the Dyadic Adjustment Scale (A-DAS) measured partner relationship.
Results
Retention rates —defined in three ways— were: (1) Total retention (percentage of participants completing the 4-6 month postpartum interview) was 41.7% (31.2% intervention and 61.4% control); (2) Retention from randomization to (a) completion of initial evaluation and attendance of > 1 intervention sessions was 42.4%; and (b) completion of initial evaluation (control) was 82.2%; and (3) Follow-up retention: (a) intervention participants attending > 1 sessions that completed the intervention as well as the 4-6 months postpartum interview was 73.5%; and (b) control participants assesses in this period was 66.6%. For those who came to at least one intervention session 83% completed the intervention.
The predictors of total retention were: being single, more educated, and poor partner relationship quality. For the intervention condition, predictors of (a) retention from randomization to attendance to > 1 sessions were anxiety and stressful life events, and (b) for follow-up retention was being employed.
Conclusions
In the present study, retention of participants was even lower than what has been found in similar interventions. However, attendance rates of the course, once the participants had attended one session, were very good. In terms of predictors of retention, women at high risk of depression (single, with poor partner quality relationship, more stressful life events and high anxiety) were more committed to participating in the study. Consequently, in order to increase retention rates, future interventions should target women that present such risk factors. Nevertheless, those with low educational attainment and homemakers, who are a vulnerable group, were difficult to retain and thus remain a challenge in postpartum depression prevention studies. We conclude that rates and predictors of retention differed depending on points of measurement, suggesting different strategies to optimize participation.
Keywords: Postnatal depression, prevention, retention, psycho-educational interventions.
Resumen
La depresión perinatal cobra cada día mayor reconocimiento como un problema importante de salud mental pública; en consecuencia, ha crecido el interés por desarrollar estrategias para prevenir la depresión posparto, que lleven a evitar sus consecuencias adversas. Sin embargo, las peculiaridades del periodo perinatal dificultan tanto el reclutamiento como la retención de esta población a lo largo del tiempo, cuando se evalúan intervenciones preventivas. El objetivo del estudio es examinar las tasas de retención y las variables que predicen las mismas en un estudio longitudinal aleatorio controlado (EAC) para prevenir la depresión posparto.
Método
Participantes: Trescientas setenta y siete embarazadas que mostraron riesgo de depresión fueron aleatorizadas a grupos de intervención y control y evaluadas durante el embarazo y a las 6 semanas y a los 4-6 meses después del parto. La muestra se tomó de salas de espera de tres instituciones que proporcionan atención prenatal.
Intervención: La intervención se desarrolló a partir de modificar una anterior dirigida a mujeres con depresión para incluir información sobre el embarazo y puerperio normales desde una perspectiva psicoanalítica y de factores de riesgo de depresión posparto. Pretende reducir la depresión al reforzar los pensamientos positivos y las actividades agradables, mejorar la autoestima y el autocuidado, desarrollar habilidades que fortalezcan el apoyo social y explorar las expectativas poco realistas sobre el embarazo y la maternidad. Se imparte en ocho sesiones grupales durante el embarazo, dos horas por semana.
Instrumentos: Los síntomas de depresión se midieron con la segunda versión del Inventario de Depresión de Beck (IDB-II), los de ansiedad con la correspondiente subescala del Hopkins Symptom Check List 90 (SCL-90) y el apoyo social con la escala de Apoyo Social Apgar (SSA). Una selección de 12 reactivos sobre estresores potenciales y dificultades persistentes se usó para medir sucesos vitales y la Escala de Ajuste Diádico (A-DAS) para evaluar la satisfacción con la relación de pareja.
Resultados
Las tasas de retención definidas de tres maneras fueron: 1. La retención total (participantes aleatorizadas que concluyeron con todo el procedimiento hasta la entrevista a los 4-6 meses posparto) fue de 41.7% (31.2% intervención y 61.4% control). 2. La retención desde la aleatorización hasta (a) completar la entrevista inicial y asistir a > 1 sesión de intervención fue de 42.4% y (b) completar la evaluación inicial (control) fue de 82.2% (c). 3. La retención hasta el seguimiento: (a) proporción que inició y completó la intervención, esto es, que asistió a > 4 sesiones, así como a la entrevista a los 4-6 meses posparto fue de 73.5% y (b) participantes del grupo control que fueron entrevistadas en este periodo fue de 66.6%. Para quienes asistieron a por lo menos una sesión, la tasa de asistencia a la intervención fue de 83%.
Las variables que predijeron la retención totalfueron: ser soltera, tener mayor nivel de escolaridad y la mala relación de pareja. En el grupo de intervención, las variables que predijeron (a) la retención desde la aleatorización hasta asistir a > 1 sesión de intervención fueron la presencia de ansiedad y de sucesos estresantes, y (b) la retención hasta el seguimiento aumentó en mujeres que estaban o habían estado empleadas los últimos seis meses.
Conclusiones
Los resultados son consistentes con los de trabajos anteriores respecto a la dificultad para retener mujeres embarazadas y en el puerperio en ensayos a lo largo del tiempo. En el presente estudio la tasa de retención fue aún más baja de lo que han encontrado otros autores, sobre todo debido a la enorme pérdida de participantes que firmaron el consentimiento informado y fueron aleatorizadas y no asistieron a ninguna sesión de la intervención. Al mismo tiempo, es interesante notar que la tasa de asistencia a la intervención, una vez que las participantes se presentaron a una primera sesión, fue muy alta. Esto habla de la alta aceptación que ésta tuvo entre las participantes.
En cuanto a los factores que predijeron la retención, las mujeres con alto riesgo de depresión (sin pareja, con una relación mala con la pareja, con más sucesos estresantes y síntomas de ansiedad) fueron las más comprometidas en participar en el estudio. Por lo tanto, una manera de mejorar la tasa de retención es a través de dirigirla a mujeres que presenten estos factores de riesgo. Por otro lado, fue difícil retener a aquellas con bajo nivel de escolaridad y a las amas de casa, que también son una población vulnerable. Saber cómo mejorar la retención de este grupo sigue siendo un reto para estudios posteriores de prevención de la depresión posparto. Podemos concluir que las tasas y los factores que predicen la retención varían dependiendo de la manera en que se definan, lo que sugiere que las estrategias para optimizar la retención deben adecuarse a cada una de estas definiciones.
Palabras clave: Depresión posparto, prevención, retención, intervenciones psicoeducativas.
INTRODUCTION
Perinatal depression is increasingly recognized as a significant public mental health problem. Approximately 10 to 15% of women during childbearing years experience perinatal depression1 which negatively affects mothers' health, their infants' development, and the quality of mother-infant relationships.2,3 Parallel to these findings is a major interest in developing strategies to prevent postpartum depression to avoid its detrimental consequences.4 The perinatal period, however, is different from other periods in women's lives because of the accompanying physiological and psychological changes, the demands of new parenthood and the expected norms that pregnancy and giving birth are celebratory occasions. These differences may make it more difficult to recruit participants at this stage5 and to retain them over time. Although randomized intervention trials increase internal validity, lack of compliance and attrition are common research challenges that can reduce statistical power and confuse outcome results.6,7 Lack of retention in prevention interventions also reduces the likelihood of receiving effective treatments and may increase costly future care if participants become clinically depressed.
To our knowledge, there are eight prevention intervention studies of perinatal depression that reported retention rates.8-16 All of these studies were randomized controlled trials that took place in the United Kingdom, the United States and Australia, evaluated psycho-educational interventions with different theoretical perspectives, and were conducted during pregnancy in a period of four to twelve sessions, with some extending these interventions to the postpartum period. This research conceptualizes retention efforts differently. First, it is defined as the percentage of women who remained in the study from the beginning to the end, including follow-up interviews (from 3 to 12 months postpartum). In this respect, overall, retention rates range from 59.2%16 to 94.5%.12 The second way that intervention studies have defined retention is to examine course attendance for intervention participants (i.e., the number of sessions attended out of the total possible number of sessions). Course attendance rate was low for some interventions. For instance, Stamp et al.8 reported that 31% of their participants attended a sufficient number of sessions and Brugha et al.10 reported a rate of 45%. In contrast, in Zlotnick et al.'s12 pilot sample of 37 women, an impressive 88% attended three or more out of four sessions. The main reasons for attrition in these studies were miscarriages, stillbirths and neonatal deaths.8,11,15 Other reasons attributed were stigma, poverty, being young, lack of childcare and domestic ties,8,16 belonging to a minority population14 and moving out of town.13
In a previous article, we discussed the challenges of recruiting Latina and Mexican women in the prenatal period for depression prevention trials.5 This is the first study conducted not only in Mexico but in Latin America.17 One other study has been published in Mexico, which reported that 19.3% to 22.5% of women experience clinical depression after the second and fourth weeks of delivery18 suggesting that prevention programs are needed. The aim of this paper is to examine retention rates and predictors of retention in a longitudinal randomized controlled trial aimed at preventing postnatal depression.
MATERIAL AND METHODS
Design
The study used a randomized controlled design to evaluate the effectiveness of an eight-week antenatal psycho-educational group intervention to prevent postpartum depression. At each of the institutions involved, the staff and administrators shared the research team's commitment to providing the appropriate conditions for the development of the research study. The research protocol was approved by the respective institutional review boards.
Study population
Screening interviews were conducted at three institutions in Mexico City: 1. a hospital setting that provides intensive care for women with high-risk pregnancies; 2. a women's clinic that provides obstetrics and gynecological services for women and/or wives of men in the Armed Forces. Both clinics are open to women from all regions in Mexico, although the majority is from Mexico City, and 3. a community health care center providing prenatal care and other comprehensive medical care to local women.
Recruitment procedures and eligibility screening
Pregnant women receiving antenatal care were screened and recruited for eligibility in the waiting rooms of each institution by the research team composed of advanced undergraduate and graduate students in clinical psychology. Women were eligible if through a screening checklist, they: 1. were over the age of 18; 2. were > 26 weeks pregnant at the start of the course; 3. had a minimum reading ability (had completed primary school); and 4. did not have any substance abuse or bipolar conditions. In addition to these demographic variables, they also had to meet the criteria for being at a high risk of depression (>16) on the Center for Epidemiologic Studies - Depression Scale,19 and/or having a self-reported history of depression. With this procedure, 6 484 women were screened across the three settings. Of all the respondents, 91.7% failed to meet eligibility criteria. Of those eligible, 29.8% refused to participate in the study for various reasons, while the remaining 377 were randomized into intervention (N=250) and control (N=127) conditions. A higher number was considered in the former as attrition was expected to be higher in this group. The intervention started from 1 day to 4 weeks after recruitment (for more detailed information on recruitment procedures, see Lara et al.17 and Le et al.5
Intervention
The intervention was designed by modifying a previously evaluated prevention intervention for depression in non pregnant women.20-23 It includes information on normal pregnancy and the postpartum period, from psychoanalytic24-26 and risk factors perspectives.27-30 It attempts to reduce depression levels by increasing positive thinking and pleasant activities, improving self-esteem, increasing self-care, learning skills to increase social support, and exploring unrealistic expectations about pregnancy and motherhood (adapted from Lara et al;20 Muñoz et al.;31 Solchany32). The intervention consists of eight two-hour weekly group sessions, delivered during pregnancy by facilitators with extensive training and clinical experience, and two follow-up interviews -in the postpartum period- accompanied by a reinforcement to review the main concepts of the course. The intervention program is highly structured and described in two manuals,* one for the facilitator and one for the participant. The format of each session consists of: a brief explanation of the topic in question by the facilitator, comments from participants on the bases of their own experiences, clarification, additional information and support from facilitator, individual and group exercises within the session, home assignments and sharing experiences derived from home assignments. Some of the topics review are: postpartum depression definition and risk factors, psychological changes during pregnancy, the relation with their own mother, myths about motherhood, losses that the new mothers face, importance of social support, the role of the partner/father to be, and baby and mother self-care in the postpartum. The group sessions were organized in spaces appropriate for this purpose assigned by each institution. Fourteen groups were conducted with 5 to 10 participants in each group (March 2005 through December 2006).
Retention procedures and follow-up
The research team encouraged women's participation by explaining the potential positive outcomes of their taking part in the intervention/course and establishing a good rapport with each of them. They motivated participants by reminding them by phone of each session; calling them if/ when they missed a class, and updating them with what was covered in the missing session. They were offered childcare during the sessions and a small allowance for transportation to each class or interview. After baseline assessment, participants in both conditions were given copies of an easy to read book on depression.20 Intervention and control participants were interviewed 6 weeks and 4-6 months postnatally, in any place they preferred (e.g., the clinic, their home, a public place such as a coffee shop). After each follow-up interview, intervention participants had a booster session to review and reinforce the main contents of the course. Both, intervention and control women, completed a similar battery of measures on risk factors and outcomes of depression. As compensation for their interview time, all participants received printed materials on parenthood, and a pack of diapers.
Measures
1. Demographic and obstetric data (age, years of education, marital status, occupation [either currently or within the last six months], gestation trimester, order of pregnancy and planned pregnancy).
2. Depressive symptoms were measured using the second edition of the Beck Depression Inventory,33 a 21 item self-reporting instrument that explores depressive symptom levels during the last two weeks. The scale has proved to be valid in pregnant and postnatal women34 and in Spanish-speaking populations.35 A cut-off point of >14 is considered «moderate risk» for depression.33,35
3. Anxiety symptoms were assessed with the corresponding subscale of the Hopkins Symptoms Checklist (SCL-9036). The scale has been used with pregnant women,37 and validated in Mexico.38,39 A cutoff point of > 18 was based on Lara et al.'s39 data.
4. Social support was measured with the Social Support Apgar (SSA40) which evaluates the perception and
satisfaction with various types of social support during pregnancy, used in Spanish speaking populations.41 A modified version of the SSA was used, in which a source of social support, Partner, was changed to Baby's Father and My Parents was separated into My Mother and My Father, with the latter yielding five more questions for the SSA. Thus, thirty questions are responded according to the degree of satisfaction in a Likert scale, and a score of > 20 was used, meaning more satisfaction with support.40
5. Stressful life events. A short form of 12 items representing potential stressors (e.g., illness, accident, job loss) was used.42 It assesses the occurrence of the event within the last six months and the degree of stress produced (0=the event was not present; 1=it was present but produced no stress, 2=it produced little stress, 3=it produced moderate stress, 4=it produced great stress). Categories for the logistic regression analyses were established using a score of > 13 representing the 75th percentile.
6. The Abbreviated Version of the Dyadic Adjustment Scale (A-DAS43) consists of 7 items of the original 32 items developed by Spanier.44 The total summed score ranges from 0-30, with higher scores indicating higher levels of marital/partner adjustment. The A-DAS has been found to have good psychometric properties43 among ethnic minorities, including Hispanics.45 A cut-off point of > 15 was used after Sharpley and Cross.46
In this paper, the retention rate is defined in three different ways: 1. Total retention: number of participants in both conditions (intervention and control) who completed the 4-6 month postpartum interview; 2. Retention fromrandomization to: (a) completion of initial evaluation and attendance of > 1 intervention sessions (intervention), and (b) completion of initial evaluation (control); and 3. Follow-upretention: (a) the number of participants attending at least one session that completed the intervention (i.e., > 4 sessions) and the 4-6 month postpartum interview (intervention), and (b) participants interviewed 4-6 months postpartum (control). In addition, we assessed the predictive value of several variables on each of the three definitions of retention rate, although for definitions 2 & 3 analyses were only conducted for the intervention condition, as it was in this group where lower retention was observed. Since we found no published studies that have formally identified factors to predict retention in postpartum depression prevention trials, we included as predictors the risk factors for perinatal depression, such as young maternal age,47,48 low educational attainment,47,49 being single,48,50,51 being unemployed,47 second trimester,52 multiparous condition,52 unplanned pregnancy,48,50 stressful life events,53 lack of social support, 48,50,54,55 poor relationship quality with the partner,41,56 previous depression,51,57 and anxiety. 1,58
RESULTS
Sociodemographics
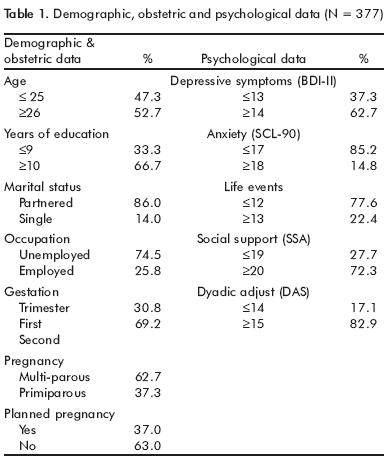
The majority of participants were over 26 years old (52.7%), had had over ten years of education (66.7%), were partnered (86%), were not employed -either currently or within the last six months- (74.5%), were in the second gestation trimester (69.2%), multiparous (62.7%), and had an unplanned pregnancy (63%).
Regarding their emotional symptoms, 62.7% scored as being at a high risk for depression, 14.8% had significant anxiety symptoms, 66.1% had experienced significant stressful life events, 63.3% were satisfied with their social support, and 82.9% reported a good level of adjustment with their partner (table 1).
Retention rates
Total retention was 41.7%, with 31.2% being retained in the intervention condition and 61.4% in the control condition (figure 1). Regardingretention from randomization to attendanceof > 1 sessions, of the 250 women randomized into the intervention condition, 42.4% attended at least one session, whereas 57.6% of those signing informed consent did not attend the intervention at all. In the control condition, retention was 82.2% during this same period. Follow-up retention, defined as (a) the proportion of participants attending one or more sessions that completed the intervention (> 4 sessions), and were assessed at 4-6 months postpartum was 73.5%, and (b) participants who completed all initial evaluations and were assessed at 4-6 months postpartum in the control group, was 66.6% (78/117).

Regarding course attendance, 82.1% (87/106) completed the intervention (> 4 sessions). In addition, for those who came to at least one session, the attendance rate was 83%, with a mean number of sessions completed of 6.7 out of eight possible sessions.
We have little or no information as to why intervention and control participants did not complete the study because we were unable to contact them again (58.7%) due to problems with phone numbers or phones having been disconnected or because they said they would come to the next session/interview and failed to show up. Of those we were able to contact, the reasons for dropping out included health problems, miscarriages, stillbirths and premature birth (19.5%), and having other commitments, such as work, study and child-care, living far away, moving out of town and various other problems (21.7%).
Predictors of retention
Three separate logistic regression analyses were performed to predict each definition of retention. The socio-demographic and psychosocial predictive variables were included in each analysis, as presented in table 1. The cut-off points for the psychosocial variables (e.g., depressive and anxiety symptoms, life events, social support, and dyadic adjustment) are also described in this table.
The significant predictors of total retention (p <0.05) were marital status (single) (OR=2.94), having had greater educational attainment (OR=1.63), and having lower adjustment with their partners (OR=1.69). The predictors of retention from randomization to attendance of>\ session were (p <0.05) having more stressful life events (OR=1.16) and high anxiety (OR=2.43). Being employed currently or in the last six months (OR=8.55) was a significant predictor (p <0.05) of follow-up retention.
DISCUSSION
This study examined retention rates and potential predictors of retention in a longitudinal, randomized controlled preventive trial of perinatal depression in Mexico.5,17 In general terms, we found that retention rates differed for each definition of retention, and the predictors were also specific for each classification, suggesting that the strategies to optimize completion of the study might also differ.
The total retention rate was very low overall (41.7%), in which only 31.2% were retained in the intervention condition and 61.4% in the control condition. These findings are lower than in previous trials, which also reported difficulties in retaining participants.9,14,16 We do not know why over half the women were unable to complete the entire study, as we lacked follow-up information. However, for those that we were able to contact again, health problems, miscarriages, premature birth, and time constraints are mentioned. Similar problems have been found in previous perinatal prevention trials,8,11,13-16 which reinforces the assertion that the perinatal period makes it more difficult to retain participants longitudinally. A particular difficulty in our study was that most of the women lived far away from where they received prenatal care; they had to travel over an hour to reach the site where the intervention was conducted. This also may explain why there was a higher retention of the control (i.e., those who completed interviews) than the intervention participants throughout the course of the study. An implication of this finding for future research with longitudinal trials in the perinatal period in Mexico would be to move the intervention closer to the participant's homes. This would be an expensive solution both in terms of research and dissemination. Nevertheless, cost-effectiveness studies could be conducted to evaluate its feasibility.
Total retention is predicted by not having a partner and being less satisfied when in a relationship. These findings are consistent with previous research demonstrating that single women48,50,51 and those who have difficult relationships with their partner are at a higher risk of depression,41,56 a fact that may have increased their need for help. Total retention was also predicted by having a higher education, similar to what has been reported for perinatal women that continue in longitudinal studies.59 In contrast, women with lower education, who are more at risk of depression during pregnancy,47,49 were poor attendees in the study, challenging investigators to figure out alternative ways to increase outreach and retention of this particular group. A possible way to address this problem is by spending more time introducing the study to the target population, organizing a group session, using visual aids, allowing for queries, and helping them find possible solutions to the barriers they encounter to participating in the study (i.e. transportation, domestic chores).
A unique characteristic of this study is that retentionfrom randomization to attendance of one or more sessions was very low (42.4%), suggesting that the greatest loss of participants occurred in the intervention group even before the course started. The fact that a high proportion of the Mexican sample failed to come to the sessions after signing informed consent can be interpreted culturally as a difficulty in saying «no» directly, and therefore expressing their refusal indirectly by not attending.5 The regression analysis for this definition of retention showed that this was predicted by experiencing stressful life events and having high anxiety symptoms. This finding indicates that the most vulnerable women did attend the intervention, consistent with the fact that people must feel great distress in order to consider taking part in a prevention activity60. This also suggests that there may be different risk levels within the «high risk» group. Specifically, those with low levels of stress and anxiety did not feel the need to attend the intervention or perhaps the commitment to an eight-week intervention is too long. One way of dealing with this problem would be to include a wider range of risk factors as selection criteria to identify those with less distress and better adjustment and to invite them to a shorter intervention (e.g., provide them with relevant information on perinatal depression) or not to intervene at all and just to re-assess depressive symptoms at a later time period.
Once women attended at least one session, many of them were able to complete the intervention (>4 sessions) and the follow up 4-6 months postpartum, as indicated by a moderately follow-up retention rate of 73.5%. In particular, an impressive 82% completed the course although a few women (8.5%) missed one of the two follow-up interviews. There was also high group attendance with a mean of 6.7/8 sessions completed. The high retention rate can reflect the intensive efforts aimed at retention (e.g., establishing good rapport with participants; phone call reminders for intervention and interviews) and/or participants' satisfaction with the intervention, which they described as improvement in their well-being and in their current problems.17 The attendance rate in this study was within the range and in some cases higher than those from other previously mentioned studies.13,15,16
Follow-up retention was predicted by employment status, meaning that participants currently or previously employed were more compliant with the intervention and the 4-6 month postpartum interview. Employed mothers receive more help with child-care and house chores than non-working mothers61 and therefore may find it easier to take the time to participate in the course. Conversely, unemployed women have fewer resources, and are therefore more house-bound. This is unfortunate as previous studies show that unemployed mothers are at a higher risk of depression.47
Overall, these results lead us to conclude that retention rates were even lower than what has been found in similar studies, but, at the same time, attendance rates of the course, once the participants had come to one session, were very good. In particular, women at high risk (single, with poor partner relationship quality, more stressful life events and high anxiety) were more committed to participate in the study. This result is consistent with our previous finding on the effectiveness of the intervention, in which better results were found in women with higher initial levels of anxiety and depression;17 consequently, in order to increase both retention and effectiveness, the intervention should target women at a very high risk of depression. Still, those with low educational attainment and homemakers, who are a vulnerable group, were difficult to retain and thus remain a challenge in postpartum depression prevention studies.
Specific actions are recommended at different stages of the intervention to improve retention. First, the selection criteria should be expanded to define a less vulnerable group (those who are less distressed, less anxious, and are satisfied with their partners) within the high risk sample, and to provide them with alternative intervention strategies. This assures that only those at higher risk, and thus those who are more motivated, are selected for study inclusion. Second, it is necessary to take more time to explore and resolve barriers to attend and comply with longitudinal interventions in non-employed mothers and in those with lower education in order to increase the likelihood of their attending the course. In summary, this first study on the prevention of postpartum depression in Mexico has some similarities with international research trials as well as some unique aspects. In both cases, the results are relevant to future studies on the prevention of postpartum depression, particularly in this country.
ACKNOWLEDGEMENTS
This study was supported by Consejo Nacional de Ciencia y Tecnología (CONACyT, Salud-2003-C01.021).
We are very grateful to Centro de Salud José Castro Villagrana, Hospital de Especialidades de la Mujer de la SEDENA and Instituto Nacional de Perinatología Isidro Espinosa de los Reyes. And to theresearch team: Teresa García-Hubard, Cecilia Mattei-Gentili, Gabriela Letechipía, Erika Trujillo, Yazmín Quintero, Sofía Arce, Alejandra Guerrero, Araceli Aguilar, Brenda Jiménez, Rita Acoltzi and Francisco Juárez.
REFERENCES
1. O'Hara MW, Swain AM. Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatry 1996;8:37-54. [ Links ]
2. Bonari L, Bennett H, Einarson A, Koren G. Risks of untreated depression during pregnancy. Can Fam Physician 2004;50:37-39. [ Links ]
3. Goodman S, Gotlib I. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychol Rev 1999;106:458-490. [ Links ]
4. Le HN, Boyd RC. Prevention of major depression: Early detection and early intervention in the general population. Clin Neuropsychiatry 2006;3(1):6-22. [ Links ]
5. Le HN, Lara MA, Perry D. Recruiting Latino women in the U.S. and women in Mexico in postpartum depression prevention research. Archiv Women Ment Health 2008;1 1:159-169. [ Links ]
6. Hogan JW, Roy J, Korkontzelou C. Handling drop-out in longitudinal studies. Stat Med 2004;23:1455-1497. [ Links ]
7. Pickering RM. Describing the subjects in a study. Palliat Med 2001;15:69-75. [ Links ]
8. Stamp GE, Williams AS, Crowther CA. Evaluation of antenatal and postnatal support to overcome postnatal depression: a randomized, controlled trial. Birth 1995;22:138-143. [ Links ]
9. Buist A, Westley D, Hill C. Antenatal prevention of postpartum depression. Archiv Women Ment Health 1999;1:167-173. [ Links ]
10. Brugha TS, Wheatley S, Taub NA, Culverwell A, Friedman T et al. Pragmatic randomized trial of antenatal intervention to prevent post-natal depression by reducing psychosocial risk factors. Psychol Med 2000;30:1273-1281. [ Links ]
11. Elliott SA, Leverton TJ, Sanjack M, Turner H, Cowmeadow P, et al. Promoting mental health after childbirth: A controlled trial of primary prevention of postnatal depression. Br J Clin Psychol 2000;39:223-241. [ Links ]
12. Zlotnick C, Johnson S, Miller I, Pearlstein T, Howard M. Postpartum depression in women receiving public assistance: Pilot study of an interpersonal-therapy-oriented group intervention. Am J Psychiatry 2001;158:638-640. [ Links ]
13. Zlotnick C, Miller I, Pearlstein T, Howard M, Sweeney P. A preventive intervention for pregnant women on public assistance at risk for postpartum depression. Am J Psychiatry 2006;163:1443-1445. [ Links ]
14. Zayas L, Mckee D, Jankowski K. Adapting psychosocial intervention research to urban primary care environments: A case example. Ann Fam Med 2004;2:504-508. [ Links ]
15. Muñoz RF, Le HN, Ghosh Ippen C, Diaz MA, Urizar G, et al. Prevention of postpartum depression in low-income women: development of the mamás y bebés/mothers and babies curse. Cogn Behav Pract 2007;14:70-83. [ Links ]
16. Austin MP, Frilingos M, Lumley J, Hadzi-Pavlovic D, Roncolato W et al. Brief antenatal cognitive behaviour therapy group intervention for the prevention of postnatal depression and anxiety: A randomised controlled trial. J Affect Disord 2008;105:35^44. [ Links ]
17. Lara MA, Navarro C, Navarrete L. Outcome results of a psycho-educational intervention in pregnancy to prevent PPD: A randomized control trial. J Affect Disord 2010;122: 109-117. [ Links ]
18. García L, Ortega-Soto Ha, Ontiveros M, Córtes J. La incidencia de la depresión posparto. México: Anales. Reseña de la VI Reunión de Investigación; Instituto Nacional de Psiquiatría; 1991; pp. 2:54-59. [ Links ]
19. Radloff L. The CES-D Scale: A self-report depression scale for research in the general population. App Psych Meas 1977;1:385^401. [ Links ]
20. Lara MA, Acevedo M, Luna S, Weckmann C, Villarreal AL, Pego C. ¿Es difícil ser mujer? Una guía sobre depresión. México: Pax; 1997. [ Links ]
21. Lara MA, Acevedo M, Luna S. Es difícil ser mujer? Guía didáctica para el trabajo de grupo. México: IMP/Pax; 2001. [ Links ]
22. Lara MA, Navarro C, Rubí NA, Mondragón L. Outcome of two levels of intervention in low-income women with depressive symptoms. Am J Orthopsychiat 2003;73:1-9. [ Links ]
23. Lara MA, Navarro C, Rubí NA, Mondragón L. Two levels of intervention in low-income women with depressive symptoms: Compliance and programme assessment. Int J Soc Psychiatry 2003;49:43-57. [ Links ]
24. Brazelton TB, Cramer B. La relación más temprana: padres, bebés y el drama del apego inicial. Barcelona: Paidós Ibérica; 1993. [ Links ]
25. Nicolson P. Loss, happiness and postpartum depression. Can Psychol 1999;40:162-178. [ Links ]
26. Stern DN. La constelacion maternal: La psicoterapia en las relaciones entre padres e hijos. Barcelona: Paidos Iberica; 1997. [ Links ]
27. Chaudron L, Klein M, Remington P, Palta M, Allen C et al. Predictors, prodromes and incidence of postpartum depression. J Psychosom Obstet Gynaecol 2001;22:103-112. [ Links ]
28. Gotlib IH, Whiffen VE, Wallace PM, Mount JH. Prospective investigation of postpartum depression: factors involved in onset and recovery. J Abnorm Psychol 1991;100:122-132. [ Links ]
29. O'Hara MW, Rehm LP, Campbell SB. Predicting depressive symptomatology: cognitive-behavioral models and postpartum depression. J Abnorm Psychol 1982;91:457-461. [ Links ]
30. Righetti-Veltema M, Conne-Perréard E, Bousquet A, Manzano J. Risk factors and predictive signs of postpartum depression. J Affect Disord 1998;49:167-180. [ Links ]
31. Muñoz FR, Le HN, Ghosh I, Diaz MA, Urizar GG, Lieberman AF. Mother and babies course. San Francisco: University of California/San Francisco General Hospital; 2004. [ Links ]
32. Sholchany LE. Promoting maternal mental health during pregnancy: Theory, assessment and intervention. Seattle: NCAST, University of Washington; 2001. [ Links ]
33. Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inven-tory-II. San Antonio, TX: Psychological Corporation; 1996. [ Links ]
34. Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T et al. Perinatal depression: Prevalence, screening accuracy, and screening outcomes. Evidence Report/Technology Assessment No. 119. (Prepared by the RTI-University of North Carolina Evidence-based Practice Center, under Contract No. 290-02-0016.) AHRQ Publication No. 05-E006-2. Rockville, MD: Agency for Healthcare Research and Quality; February; 2005. [ Links ]
35. Penley JA, Nwosu A, Wiebe JS. Psychometric properties of the Spanish. Beck Depression Inventory- II in a Medical Sample. Psychol. Assessment 2003;15:569-577. [ Links ]
36. Derogatis LR. SCL-90-R. Revised Version Manual 1. USA: 1978. [ Links ]
37. Striegel-Moore RH, Goldman SL, Garvin V, Rodin J. A prospective study of somatic and emotional symptoms of pregnancy. Psychol Women Quart 1996;20:393-408. [ Links ]
38. Cruz-Fuentes C, López L, Blas-Gracia C, González L, Chávez R. Datos sobre la validez y la confiabilidad de la Symptom Check List 90 (SCL-90) en una muestra de sujetos mexicanos. Salud Mental 2005;28:72-81. [ Links ]
39. Lara C, Espinosa I, Cárdenas ML, Fócil M, Cavazos J. Confiabilidad y validez de la SCL-90 en la evaluación de psicopatología en mujeres. Salud Mental 2005;28(3):42-50. [ Links ]
40. Norwood SL. The Social Support Apgar: Instrument development and testing. Res Nurs Health 1996;19:143-152. [ Links ]
41. Diaz MA, Le HN, Cooper BA, Muñoz RF. Interpersonal factors and perinatal depressive symptomatology in a low-income Latina sample. Cultur Divers Ethnic Minor Psychol 2007;13(4):328-336. [ Links ]
42. Lara MA, Navarro C, Navarrete L. Influencia de los sucesos vitales y el apoyo social en una intervención psicoeducativa para mujeres con depresión. Salud Publica Mex 2004;46:378-387. [ Links ]
43. Sharpley CF, Rogers HJ. Preliminary Validation of the Abbreviated Spa-nier Dyadic Adjustment Scale: Some Psychometric Data Regarding a Screening Test of Marital Adjustment. Educ Psychol Meas 1984;44(4): 1045-1049. [ Links ]
44. Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J Marriage Fam 1976;38(1):15-8. [ Links ]
45. Bird HR, Canino GJ, Davies M, Zhang H, Ramirez R et al. Prevalence and correlates of antisocial behaviors among three ethnic groups. J Abnorm Child Psychol 2001;29(6):465-78. [ Links ]
46. Sharpley CF, Cross DG. A psychometric evaluation of the Spanier Dyadic Adjustment Scale. J Marriage Fam 1982;44(3):739-747. [ Links ]
47. Mayberry LJ, Horowitz JA, Declercq E. Depression symptom prevalence and demographic risk factors among U.S. women during the first 2 years postpartum. J Obstet Gynecol Neonatal Nurs 2007;36(6):542-549. [ Links ]
48. Rich-Edwards JW, Kleinman J, Abrams A, Harlow B, Mclaughlin TJ et al. Symptoms among women in a medical group practice. J Epidemioly Community Health 2006;60:221-227. [ Links ]
49. Morales-Carmona F, Luque-Coqui M, Barroso-Aguirre J. Alteraciones emocionales en una muestra de mujeres mexicanas con eventos gineco-obstétricos. Perinatol Reprod Hum 2002;16:157-162. [ Links ]
50. Lara MA, Navarro C, Navarrete L, Cabrera A, Almanza J et al. Síntomas depresivos en el embarazo y factores asociados en pacientes de tres instituciones de salud de la Ciudad de México. Salud Mental 2006;29:55-62. [ Links ]
51. Marcus SM, Flynn HA, Blow FC, Barry KL. Depressive symptoms among pregnant women screened in obstetrics settings. J Womens Health 2003;12:373-380. [ Links ]
52. Lara MA, Le HN, Letechipia G, Hochhausen L. Prenatal depression in Latinas in the U.S. and Mexico. Matern Child Health J 2009;13(4):567-576. [ Links ]
53. Alvarado R, Rojas M, Monardes J, Perruca E, Neves E et al. Cuadros depresivos en el postparto en una cohorte de embarazadas: construcción de un modelo causal Cuadros depresivos en el postparto en una cohorte de embarazadas: construcción de un modelo causal. Rev Chil Neuro-Psiquiat 2000;38:84-93. [ Links ]
54. Canaval G, González M, Martínez-Schalmosser L, Tovar M, Valencia C. Depresión posparto, calidad de vida y apoyo social en mujeres de Cali. Colomb Med 2000;30(1):4-10. [ Links ]
55. Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: A synthesis of recent literature. Gen Hosp Psychiatry 2004;26:289-295. [ Links ]
56. Beck CT. Postpartum depression: It isn't just the blues. Am J Nurs 2006;106:40-50. [ Links ]
57. Bernazzani O, Saucier JF, David H, Borgeat F. Psychosocial predictors of depressive symptomatology level in postpartum women. J Affect Disord 1997;46(1):39-49. [ Links ]
58. Horwitz SM, Briggs-Gowan MJ, Storfer-Isser A, Carter As. Prevalence, correlates, and persistence of maternal depression. J Womens Health 2007;16(5):678-691. [ Links ]
59. Morse C, Durkin S. Staying the distance: Characteristics of women who do not continue in a longitudinal study of pregnancy-related moods. Psychol Health Med 2004;9(3):293-305. [ Links ]
60. Ireys HT, Devet KA, Chernoff R. Who joins a preventive intervention? How risk status predicts enrollment. J Community Psychol 2001;29(4):417-427. [ Links ]
61. Lara MA, Acevedo M, López EK, Fernández M. La salud emocional y tensiones asociadas a los papeles de género en las madres que trabajan y en las que no trabajan. Salud Mental 1993;16(2):13-22. [ Links ]
* Lara MA, García T. Despertando tu amor para recibir a tu bebé. Como prevenir la tristeza y la depresión posparto en el embarazo y después del parto. Pax, México; 2009. Lara MA, García MT. Prevención de la depresión posparto: Guía para orientadoras. Pax, México (in press).














