Servicios Personalizados
Revista
Articulo
Indicadores
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Salud mental
versión impresa ISSN 0185-3325
Salud Ment vol.33 no.3 México may./jun. 2010
Artículo original
The association between type of confidant and depressive symptomology in a sample of Mexican youth
Jóvenes mexicanos y depresión: el rol de confidentes
Mirna Ponce,1,2 Yvonne N. Flores,2,3 Jyoti Mudgal,2 Gerardo Huitrón,3 Elizabeth Halley,4 Katia Gallegos–Carrillo,2 Jorge Salmerón2
1 Department of Epidemiology, University of California, Los Angeles (UCLA), Los Angeles, CA.
2 Unidad de Investigación Epidemiológica y en Servicios de Salud, Instituto Mexicano del Seguro Social (IMSS), Morelos, Mexico.
3 UCLA Department of Health Services, School of Public Health and Jonsson Comprehensive Cancer Center, Los Angeles, CA.
4 Universidad Autónoma del Estado de México, Toluca.
*Correspondence:
Dr. Yvonne N. Flores,
Unidad de Investigación Epidemiológica y en Servicios de Salud,
Instituto Mexicano del Seguro Social (IMSS),
Av. Plan de Ayala esq. Calle Central s/n
Col. Chapultepec, 62450
Cuernavaca, Morelos.
Tel/Fax (52–777) 100–1364;
Email: ynflores@ucla.edu
Recibido primera versión: 25 de marzo de 2009.
Segunda versión: 20 de noviembre de 2009.
Aceptado: 20 de enero de 2010.
Abstract
Background
The current lifetime prevalence of depression among females in Mexico is 9.1% and 2.9% among males. The overall lifetime prevalence of depression is 6.2% among the general population of Mexico. Individuals that experience depressive symptomology at a young age are more likely to experience a depressive episode later in life. The risk of recurrence 24 months after the first episode of depression is 37.3%. There is scarce information about the prevalence of depression among adolescents in Mexico. However, a study of adults in Mexico City by Benjet et al. found that 2.8% of females and 1.1% of males experienced a depressive episode during adolescence. Research indicates that adolescents are especially vulnerable to mental and physical health problems. During the developmental transition, females are more vulnerable to these problems than males, including depression. The ways in which adolescents adapt and become adults can either protect or put them at risk for depressive symptomology and subsequent mental and physical disorders. The act of disclosure (talking to a confidant), which involves the sharing of personal thoughts and ideas with others, is an important mechanism through which adults and children form intimate relationships and develop good mental health.
Objectives
The objective of this study was to determine the association between type of confidant and depressive symptomology, and to identify some potential risk and protective factors of depression, including differences by gender, among a sample of Mexican youth. We hypothesized that not having a confidant would be associated with greater levels of depressive symptomology, and that this would differ by gender.
Methods
We used cross–sectional data obtained from 1,079 youths and adolescents aged 11 to 20 who were recruited to participate in the Health Worker Cohort Study (HWCS) between the years of 2004 and 2006. The HWCS included children and relatives of workers from the Instituto Mexicano del Seguro Social (IMSS) in Morelos and from Instituto Nacional de Salud Pública, both located in Cuernavaca. Participants were also selected from a similar sample of workers from the Universidad Autónoma del Estado de México (UAEM) in Toluca, capital of the State of Mexico. The participants from all three study sites are being followed in an ongoing cohort study of lifestyle and health. A self–reported questionnaire was administered to obtain information on lifestyle factors, socio–demographic data, health status, and quality of life. Bivariate and multivariate analyses were conducted to determine the association between confidant type and levels of depressive symptomology while controlling for demographic factors. Stratified analyses were also carried out, as it was hypothesized that the effect of disclosure to a confidant would vary by gender.
Results
In our study population, males had significantly lower levels of depressive symptomology than females; the mean BDI score for males was 5.6 and for females it was 8.7. Among both males and females, having only peer confidants is associated with higher levels of depressive symptomology, and having family confidants is associated with lower levels of depression. Males with peer confidants have the highest levels of depressive symptomology followed by those with no confidants, and those with family and peer confidants, as compared to males who reported having only a family confidant. Females with no confidant or with only peer confidants have higher levels of depressive symptomology than females with only family confidants. Among females, depressive symptomology increases with age, with females aged 17–20 having the highest levels of depressive symptomology. Financial symptomology predicts depressive symptomology among both males and females.
Conclusions
Our study shows that having a family member to talk to may be a protective factor against depressive symptomology among this sample of Mexican youth. Adolescents with a family confidant were found to have significantly lower levels of depressive symptomology than those who have only peer or no confidants. In the transition to adulthood, the presence of a family confidant positively influences the emotional well–being of boys and girls. Interventions that address the different disclosure needs of male and female adolescents may help reduce or prevent depressive symptomology among this population.
Key words: Adolescents, Mexico, mental health, depressive symptomology, confidants.
Resumen
Antecedentes
La prevalencia actual de depresión en México es de 9.1% en las mujeres y de 2.9% entre los hombres. En conjunto, la prevalencia de depresión entre la población general de México es de 6.2% durante el transcurso de la vida. Diversos estudios señalan que los individuos que presentan a edades tempranas un trastorno depresivo es más probable que más tarde en su vida sufran un episodio depresivo. El riesgo de presentar una recurrencia de depresión 24 meses después del primer episodio es de 37.3%. En México hay escasa información sobre la prevalencia de depresión entre los adolescentes. Las investigaciones señalan que los adolescentes son vulnerables a padecer problemas de salud tanto físicos como mentales. Durante la transición del desarrollo de la adolescencia, las mujeres son más vulnerables que los hombres a padecer este tipo de problemas, entre los que se encuentra la depresión. Las formas en que los adolescentes se adaptan y se convierten en adultos pueden protegerlos o ponerlos en riesgo de presentar trastornos depresivos y subsecuentes trastornos físicos y mentales. El acto de divulgar (platicar con un confidente) implica compartir pensamientos e ideas personales con otros y es un importante mecanismo por medio del cual los adultos y los niños forman relaciones cercanas y desarrollan una buena salud mental.
Objetivos
El objetivo de este estudio fue determinar la asociación entre el tipo de confidente y el trastorno depresivo e identificar algunos riesgos potenciales y factores protectores de depresión en una muestra de jóvenes mexicanos. Planteamos la hipótesis de que no contar con un confidente podría estar asociado con niveles más altos de sintomatología depresiva, asociación que podría ser distinta de acuerdo con el sexo.
Métodos
Se utilizaron los datos transversales recabados en 1079 jóvenes y adolescentes de 11 a 20 años, quienes fueron reclutados para participar en el Estudio Cohorte de Trabajadores (ECT) entre los años de 2004 a 2006. El ECT incluye niños y familiares de trabajadores del Instituto Mexicano del Seguro Social (IMSS) en Morelos y del Instituto Nacional de Salud Pública, ambos localizados en la ciudad de Cuernavaca. También se seleccionó una muestra similar de participantes de los trabajadores de la Universidad Autónoma del Estado de México (UAEM) en Toluca, capital del Estado de México. Los participantes de las tres sedes están en seguimiento en el estudio de cohorte prospectivo sobre salud y estilos de vida. Se administró un cuestionario autoaplicado para obtener información sobre datos sociodemográficos, estilos de vida, estado de salud y calidad de vida. Se realizaron análisis bivariados y multivariados para determinar la asociación entre el tipo de confidente y niveles de sintomatología depresiva controlando por factores sociodemográficos. Adicionalmente, se realizaron análisis estratificados bajo la hipótesis de que el efecto de divulgación a un confidente (platicar con un confidente) podría variar por sexo.
Resultados
En nuestra población de estudio, los hombres reportaron niveles significativamente más bajos de trastorno depresivo que las mujeres; la media de la puntuación del Inventario de Depresión de Beck (BDI) fue de 5.6 para hombres y de 8.7 para las mujeres. Entre ambos, tanto hombres como mujeres, contar sólo con amigos como confidentes se asocia con altos niveles de trastorno depresivo y contar con familiares como confidentes se asocia con menores niveles de depresión. Los hombres que cuentan con amigos como sus confidentes tienen los niveles más altos de sintomatología depresiva, seguidos por aquellos que cuentan con confidentes y de quienes cuentan como confidentes a amigos y familiares. Las mujeres que no tienen confidentes o que sólo cuentan con amigos como confidentes tienen niveles más altos de sintomatología depresiva que las que sólo cuentan con familiares como confidentes. Entre las mujeres, la sintomatología depresiva se incrementa con la edad; como lo señalan nuestros resultados las mujeres de 17 a 20 años presentaron los niveles más altos de sintomatología depresiva. En relación con otros factores asociados, encontramos que, tanto en hombres como en mujeres, el estrés financiero es un predictor de sintomatología depresiva.
Conclusiones
Nuestro estudio señala que contar con un miembro de la familia con quien platicar es un factor protector contra el trastorno depresivo en esta muestra de jóvenes mexicanos. Los adolescentes que cuentan con un familiar como confidente presentan niveles de sintomatología depresiva significativamente menores que aquellos que sólo cuentan con amigos o quienes no tienen confidentes. En la transición hacia la adultez, la presencia de un familiar como confidente influye positivamente en el bienestar emocional de niñas y niños. Las intervenciones que toman en cuenta las diferentes necesidades de divulgación de los adolescentes (de contar con un confidente) podrían ayudar a reducir o prevenir la sintomatología depresiva en esta población.
Palabras clave: Adolescentes, México, salud mental, depresión, confidentes.
INTRODUCTION
The current lifetime prevalence of depression among females in Mexico is 9.1% and 2.9% among males. The overall lifetime prevalence of depression is 6.2% among the general population of Mexico.1 Individuals that experience depressive symptomology at a young age are more likely to experience a depressive episode later in life.2,3 The risk of recurrence 24 months after the first episode of depression is 37.3%.4 There is scarce information about the prevalence of depression among adolescents in Mexico. However, a study of adults in Mexico City by Benjet et al. found that 2.8% of females and 1.1% of males experienced a depressive episode during adolescence.2
Research indicates that adolescents are vulnerable to mental and physical health problems.2,5–7 Females are more vulnerable to these problems than males during the developmental transition,8 including depression.9,10 The ways in which adolescents adapt and become adults can either protect or put them at risk for depressive symptomology and subsequent mental and physical disorders. One of the important changes that occur in adolescence is a shift in confidant type. For example, adolescents begin to disclose their thoughts and problems to their friends more than their families as they get older.11,12
The act of disclosure, which involves the sharing of personal thoughts and ideas with others, is an important mechanism through which adults and children form intimate relationships and develop good mental health.11 Research has been conducted to trace the pattern of disclosure from childhood to adulthood in the United States and other countries. Studies have found that children pattern their relationships after parent–child methods of disclosure.13–15 Children 11 years and younger do not differentiate between family and peers, but after this age a change takes place from disclosure to both family and peers to disclosure only to peers.11,12 For girls, the period of disclosure transition occurs in early adolescence (12 to 14 years) and for boys it occurs after the age of 15.12
If confidants are not kept or replaced during this period, cognitive distortions and loneliness may increase16 and cause a rise in levels of depressive symptomology. If examples of peer and familial relationships as well as models of social networking are not provided by the family, adolescents may be more susceptible to depression as they seek sources for disclosure.17,18 Additionally, studies have found that males disclose more to an opposite sex friend than a same sex friend,11,12,16–18 which would indicate a different disclosure pattern between males and females. Consistent with notions of gender roles, females disclose more to same sex friends and report more disclosure.11,12,16 Conversely, males are less likely to report disclosure and are more likely to form relationships and express emotions through action rather than through disclosure.13 Therefore, the impact of disclosure on depressive symptomology may be less for adolescent boys than for girls because they have other ways to express themselves.
Some other effects of disclosure on the well–being of youths and adolescents include assistance in the development of problem solving skills and the process of disclosure also contributes to the adolescent perception of the world.14,19 One of the roles of the family is to impart tradition and to reinforce acceptable behavior.20,21 Parents and older family members also help to establish how children and adolescents choose and relate to certain peers.17 Primarily, peers are equals that share ideas and assist each other in forming individual identities.11,13 Given the different functions of peer versus family, the shift from family to peer confidants may have an overall negative impact on the development and health of the adolescent if the shift occurs too early or if there is an inadequate model for social networking.15 In addition to the aforementioned gender and developmental issues, other risk factors for high levels of depressive symptomology include adolescents living in single parent or step–parent homes22 and low socioeconomic status.23
The objective of this study was to determine the association between type of confidant and depressive symptomology, and to identify some potential risk and protective factors of depression, including differences by gender, among a sample of Mexican youth. We hypothesized that not having a confidant would be associated with greater levels of depressive symptomology, and that this would differ by gender.
METHODS
Study population and subject recruitment
The study population consisted of a sample of youths between the ages of 11 and 20 who enrolled, along with their parents, in the Health Worker Cohort Study (HWCS) between March 2004 and April 2006. The study participants included children of workers from the Mexican Institute of Social Security (IMSS) and the National Institute of Public Health, both located in Cuernavaca, in addition to children of workers at the Universidad Autónoma del Estado de México in Toluca, the capital of the neighboring state. The participants from all three study sites are being followed in an ongoing cohort study of life style and health. The specifics of the study design, methodology and baseline characteristics of participants are described elsewhere.24,25 The ethical committees of all participating institutions approved the study protocol and consent forms for the cohort study. Written consent was obtained from all study subjects, and parental consent was obtained for all participants under the age of 18.
A total of 2345 children and adolescents between the age of 6 and 20 years, whose parents were participating in the HWCS, joined the study during this period. Participants who had missing data on age, gender, education, or living structure were excluded from the analysis. Study participants who indicated that they were married, living with a partner or separated were also excluded from the analysis. A total of 1079 adolescents between 11 and 20 years of age met the study inclusion criteria. The following information was obtained from the self–reported questionnaires that the participants completed: socio–demographic data, lifestyle factors, health status, and quality of life. The results reported for this analysis represent the baseline findings of what will be a multi–phase longitudinal cohort study.
Measures
Depression
For this study, depression was measured using the Beck's Depression Inventory for Youth (BDI). This scale has shown excellent internal consistency, reliability, adequate test–retest reliability,26–29 and has been validated to measure depressed mood among adolescents.30 The scale has been used and tested extensively in various populations with good results, although it was originally intended for clinical populations.31 The scale was translated by researchers working on the Health Worker Cohort Study, and this is the first time it has been used in a Mexican adolescent population. Cronbach's alpha shows a reliability of 0.88 in the study population. The BDI includes 21 items to assesses symptoms of depression during the past two weeks, with items scored from 0–3, where 0 = no symptom and 3= high level of symptom. This scale includes items such as: <<I do not feel sad>>; <<I feel sad sometimes>>; <<I am pretty sad all the time>>; <<I am so very sad that I can't stand it.>> A total BDI score is calculated by summing across the items. The range of BDI scores in our study population is from 0 to 44.
Demographic characteristics
The age, gender, level of education and family structure of respondents was included in the analysis to control for demographic characteristics. Age was divided into four categories: 11–12, 13–14, 15–16 and 17–20 for the analysis. Education was included as a categorical variable: (1) elementary school, (2) secondary, and (3) preparatory, professional school, and college, which were aggregated into one category (preparatory or more). The family living structure was classified into one of three categories: (1) living with two biological parents, (2) living with one parent, and (3) living with one biological parent and one step–parent.
Financial security
A four–question scale of financial strain was created to measure the effects of economic strain on depressive symptomology. Participants were asked how frequently they felt their family had enough money available to cover certain necessities such as <<the type of food their family should have>> and <<the medical attention their family should have.>> Items were scored: 1= Never, 2= Sometimes, 3= Frequently, and 4= All the time. The range in scores was 4 to 16 with 16 representing the highest level of financial distress, and 4 the lowest level of financial distress.
Confidant Variable
Participants were asked to report if they had someone with whom they discuss their private and personal issues. They were also asked to indicate who they talk to from a list of response choices that was provided along with an open–ended response category. The confidant type variable was categorized as: (1) family members (mother, father, stepmother, step–father, sister and/or brother), (2) peers (friend and/or boy/girlfriend) and (3) none. These categories were used because we found no detectable differences for each specific type of family or peer confidant in this sample. Psychologists and priests were also listed as confidant response choices, but they were not included in the analysis because few participants chose these options as a source of disclosure.
Analysis
Statistical tests were run to ensure comparability across sub–populations within the sample. One way ANOVA testing was conducted to identify differences in levels of depressive symptomology among the various data collection sites. Multivariate regression was used to determine the association between the confidant variables and differing levels of depressive symptomology while controlling for demographics. Analyses were conducted with STATA 8.0.32
RESULTS
Table 1 shows the distribution of the mean BDI scores by gender, age, education, family living structure, confidant type, and financial distress in the study population. As indicated in column 1, more females participated in the study than males, 55% vs. 45%, respectively. Males have significantly lower levels of depressive symptomology than females: the mean BDI score for males is 5.6 and for females it is 8.7. Adolescents aged 15 and older have higher levels of depressive symptomology than adolescents between the ages of 11 to 14. Participants who reported that they were in secondary school have greater depressive symptomology than those who were in elementary school. Respondents who indicated that they live with one parent and a stepparent have a higher level of depressive symptomology than those who reported living with both biological parents or with one parent. Participants who stated that they have no confidants or only a peer confidant have higher levels of depressive symptomology than those with family confidants or family and peer confidants. Financial distress is also associated with higher levels of depressive symptomology in this population.
Columns 2 and 3 of table 1 report the differences observed among the male and female study participants. Males who reported having no confidants or a peer confidant have more depressive symptomology than males with family confidants (table 1, column 2). Females over the age of 13 have significantly higher levels of depressive symptomology than those aged 11 to 12. Females with a secondary education or more have higher depressive symptomology than those with a primary education or less. Females living with one parent and a step–parent have higher levels of depressive symptomology than females living with both parents. Females who reported having no confidants or a peer confidant have higher levels of depressive symptomology than females with family confidants (table 1, column 3).
The results reported on table 2 indicate the change in depressive symptomology after adjusting for age, education, family living structure, and financial distress. Respondents without a confidant or with peer confidants experience higher levels of depressive symptomology in comparison to those who report having family confidants. Females are more likely to experience depressive symptomology than males. Study participants aged 17 to 20 also have higher levels of depressive symptomology than those aged 11 to 16. Financial distress is a predictor of levels of depressive symptomology as well (table 2).
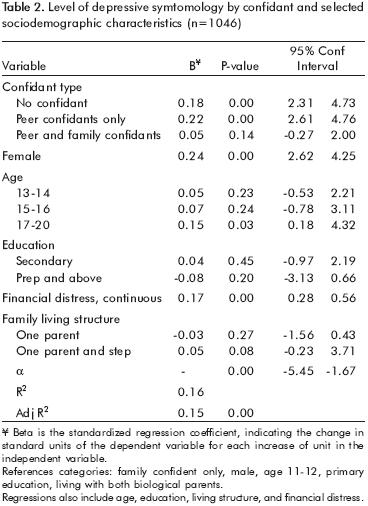
Table 3 shows the results of a gender stratified analysis that controlled for age, education, and family living structure. When compared to males with only family confidants, males with only peer confidants have the highest level of depressive symptomology, followed by having no confidant, and peer and family confidants. Females with no confidant or with only peer confidants have higher levels of depressive symptomology than females with only family confidants. Among females, depressive symptomology increases with age, with females aged 17–20 having the highest levels of depressive symptomology. For females, living with one parent and one step parent results in higher levels of depressive symptomology than living with both biological parents. Financial distress appears to be associated with depressive symptomology among both males and females (table 3). All reported results are significant at the p<0.05 or p<0.01 level.
DISCUSSION
Our study shows that having a family member to talk to may be an important protective factor against depressive symptomology among this sample of Mexican youth. Adolescents with a family confidant have significantly lower levels of depressive symptomology than those who have only peer or no confidants. There is no significant difference in the level of depressive symptomology among adolescents with family confidants versus those with both family and peer confidants. The effect of having a family member confidant, with or without peers, appears to be an independent and significant factor in helping to lower levels of depressive symptomology among male and female adolescents. Whether having a family confidant precedes or buffers against depressive symptomology cannot be determined from this analysis of cross–sectional data.
Females with family confidants appear to be more protected against depressive symptomology than females without family confidants. The finding is consistent with gender roles and the social identities of females as communicators.11,12,33 Female adolescents with a family confidant have slightly lower levels of depressive symptomology than females with both peer and family confidants. A possible explanation may be the cultural emphasis placed on the family and the role of the social female as factors which help to reduce depressive symptomology among adolescent girls.13
Our findings regarding the effect of age on depressive symptomology are somewhat different from what is expected in a healthy adolescent population, because the risk of depressive symptomology among females appears to increase at the age of 13, rather than at the expected age of 15.2,3,9,10 This finding may be attributed to a developmental trajectory that could be different among female adolescents in Mexico and adolescents in the United States. In the multivariate analysis, we controlled for differences in age and other variables to evaluate the actual relationship between depressive symptomology and disclosure.
Males with peer confidants have the highest levels of depressive symptomology followed by those with no confidants, and those with family and peer confidants, as compared to males who reported having only a family confidant. The increased risk of depressive symptomology among males with peer and family confidants and males who reported not having a confidant is similar. The cultural importance of family is clearly associated with lower levels of depressive symptomology among both males and females in our study population. However, we did observe some differences by gender, including the fact that not having a confidant was more strongly associated with depressive symptomology for females than for males. Peer confidants are associated with the highest levels of depressive symptomology for the males in our study, while not having a confidant presents the highest risk of depressive symptomology for females. If we consider that family confidants may be protective against the potentially negative effect of peer confidants, as this analysis suggests, the buffer effect of family confidants appears to have a stronger influence among males.
A limitation of our analysis is that we were not able to determine the gender or age of the confidant. Therefore, apart from the familial support and model provided in early adolescence, one would expect that levels of depressive symptomology would be highest in males until they make the transition to an opposite sex confidant or if they retain their familial confidant. However, for this type of study we would need longitudinal data. The effect of disclosure on depressive symptomology appears to be different among the females in our sample as is evident by the coefficients in the linear regression, as well as in the bivariate analysis. The dependence on the family as confidants by females is not the same. Females have similar levels of depressive symptomology with family confidants as they do with both family and peer confidants, whereas males have differing levels of depressive symptomology between having family confidants versus having both family and peer confidants. However, without data on the quality of the relationships, the mechanisms of the role of the type of confidant cannot be established.
The reliability and validity analyses that were conducted by gender and race show that the BDI scale is reliable and valid for both males and females. However, the diagnostic criteria for depressive symptomology may differ between males and females,34 which may further introduce differences in the relationship between confidant type and depressive symptomology.
Another limitation of these analyses is the lack of generalizability of our findings. These results are limited to the study population, which is representative of youths from low to middle income families in central Mexico. Convenience sampling, sample size, and the type of data available further limited the analyses that could be conducted as part of this study. Another limitation is that the probability of answering the questionnaire may be higher among adolescents that have a good relationship with their family. This may partially explain why family confidants are much higher than even family and peer confidants in boys.
Despite these limitations, our results indicate that the presence of family confidants appears to be associated with lower levels of depressive symptomology among the females and males in our study population. Our findings support the need to establish interventions that assist young females and males in coping and building relationships that satisfy and protect them from depressive symptomology, especially if their families are unable to provide this support. Future research is needed to determine the actual mechanisms of how the type of confidant may cause, prevent, or interact with already pre–existing levels of depressive symptomology.
More research is also needed to determine the mechanisms of the impact of disclosure on the mental health and development of adolescents. A longitudinal study of the impact of familial relationships on Mexican adolescents in relation to depressive symptomology will also address possible differences in the developmental trajectory across cultures and their impact on mental health. Cognitions and coping may be involved in the association between disclosure and depressive symptomology, particularly loneliness.13,15,16 Future research should further examine the association between confidants and good mental health development in Mexican adolescents by looking at the gender, age, and quality of the relationship with the confidant, as well as the depressive status of the parent. A population–based longitudinal study could establish the possible direction of causality.
REFERENCES
1. World Health Organization. Department of Mental Health and Substance Abuse. Mental Health Atlas 2005. Mental Health, Evidence and Research. Geneva; 2005. [ Links ]
2. Benjet C, Borges G, Medina–Mora M, Fleiz Bautista C. Zambrano–Ruiz, J. La depresión con inicio temprano: prevalencia, curso natural y latencia para buscar tratamiento. Salud Publica Mex 2004;46:417–424. [ Links ]
3. Benjet C, Hernandez–Guzman L. A Short–term longitudinal study of pubertal change, gender, and psychological well–being in Mexican early adolescents. J Youth Adolesc 2002;6:429–442. [ Links ]
4. Heinze G, Villamil V, Cortés J. Relapse and Recurrence of Depressed Patients: A Retrospective Study. Salud Mental 2002;25:3–8. [ Links ]
5. Feldman RA, Stiffman AR. Mental Health Disorders in Adolescence: Issues and Prospects. In: Feldman RA, Stiffman AR (eds.). Advances in Adolescent Mental Health Vol. 1, Part A. Connecticut: Jai Press Inc; 1986; pp. 1–18. [ Links ]
6. Scheiman S, Van Gundy K, Taylor J. The relationship between age and depressive symptoms: A test of competing explanatory and suppression influences. J Aging Health 2002;14:260–285. [ Links ]
7.Butcher JN, Mineka S, Hoolet JM. Abnormal psychology. Boston, MA: Pearson Education, 2007. [ Links ]
8. Benjet C, Hernandez–Guzman L. Gender differences in psychological well–being of Mexican early adolescents. Adolescence 2001;36:47–65. [ Links ]
9. Weiss B, Garber J. Developmental differences in the phenomenology of depression. Development Psychopathology 2003;15:403–430. [ Links ]
10. Cohen–Kettenis P, Everaerd. Gender role problems in adolescence. In: Feldman RA, Stiffman AR (eds.). Advances in adolescent mental health. Vol 1, Part B. Greenwich: Jai Press, Inc; 198; pp. 1–28. [ Links ]
11. Rotenberg K (ed.). Disclosure processes in children and adolescents. Cambridge studies in social and emotional development. New York: Cambridge University Press; 1995. [ Links ]
12. Mussen PH, Conger JJ, Kagan J, Huston AC. Child development and personality. New York: Harper Row Publishers; 1990. [ Links ]
13. Buhrmester D, Prager K. Patterns and functions of self–disclosure during childhood and adolescence. In: Rotenberg K (ed.). Disclosure processes in children and adolescents. Cambridge studies in social and emotional development. New York: Cambridge University Press; 1995; pp. 10–11. [ Links ]
14. Rotenberg KJ. Moral development and children's differential disclosure to adults versus peers. In: Rotenberg K (ed.). Disclosure processes in children and adolescents. Cambridge studies in social and emotional development. New York: Cambridge University Press; 1995; pp. 135–147. [ Links ]
15. Fagot BI, Luks K, Poe J. Parental influences on children's willingness to disclose. In: Rotenberg K (ed.). Disclosure processes in children and adolescents. Cambridge studies in social and emotional development. New York: Cambridge University Press; 1995; pp. 148–165. [ Links ]
16. Rotenberg K. Loneliness and the perception of the exchange of disclosures. J Soc Clin Psychol 1997;16:259–276. [ Links ]
17. Trad PV. Social Support as a risk factor for infant and childhood depression. In: Trad PV. Infant and Childhood Depression: Developmental Factors. New York: John Wiley & Sons (Wiley–Interscience Publication). 1987; pp. 159–174. [ Links ]
18. Hankin, BL. Adolescent depression: Description, causes and interventions. Epilepsy Behav 2006;8:102–114. [ Links ]
19. Thomas RM. Recent theories of human development. London: Sage Publications; 2001. [ Links ]
20. Kindermann T. Children's relationships and development of person–context relations. In: Valsiner J, Connolly KJ (eds.). Oxford: Handbook of Developmental Psychology. Oxford University Press; 2003; pp. 450–488. [ Links ]
21. Bosma H, Gerlsma C. From early attachment relations to the adolescent and adult organization of self. In: Valsiner J, Connolly KJ (eds.). Handbook of developmental psychology. Oxford: Oxford University Press; 2003; pp. 407–430. [ Links ]
22. Carlson C, Trapani J. Single parenting and step–parenting. In: Bear GG, Minke KM (eds.). Children's needs III: Development, prevention, and intervention. Washington, DC: National Association of School Psychologists; 2006; pp. 783–797. [ Links ]
23. Wight RG, Aneshensel CS, Botticello AL, Sepulveda JE. A multilevel analysis of ethnic variation in depressive symptoms among adolescents in the United States. Soc Sci Med 2004;60:2073–2084. [ Links ]
24. Halley EC, Borges G, Talavera JO, Orozco R, Vargas–Alemán C et al. Body mass index and the prevalence of metabolic syndrome among children and adolescents in two Mexican populations. J Adolesc Health 2007;40:521–526. [ Links ]
25. Katon JG, Flores Y, Salmerón J. Sexual maturation and metabolic profile among adolescents in the Mexican Institute of Social Security Health Worker Cohort Study. Salud Publica Mex 2009;51(3):219–226. [ Links ]
26. Cantwell DP, Carlson G. Problems and prospects in the study of childhood depression. J Nerv Ment Dis 1979;167:522–529. [ Links ]
27. Teri, L. The use of the Beck Depression Inventory with adolescents. J Abnorm Child Psychol 1982;10:277–284. [ Links ]
28. Beck AT, Steer RA, Brown GK: Manual for Beck Depression Inventory II (BDI–II). San Antonio, TX; Psychology Corporation. 1996. [ Links ]
29. Weiss B, Weisz JR, Politano M, Carey M, Nelson WM et al. Developmental differences in the factor structure of the Children's Depression Inventory. Pyschol Assess 1991;3:38–45. [ Links ]
30. Compas BE, Ey S, Grant KE. Taxonomy, assessment and diagnosis of depression during adolescence. Psychol Bull 1993;114:323–344. [ Links ]
31. Robinson JP, Shaver PR, Wrightsman LS. Measures of personality and social psychological attitudes: Volume 1 in Measures of social psychological attitudes series. San Diego, CA: Academic Press; 1991. [ Links ]
32. Stata. Statistical Software: Release 8.0. College Station, TX: Stata Corp., 2003. [ Links ]
33. Hunter F. Adolescents' perception of discussions with parents and friends. Dev Psychol 1985;21:433–440. [ Links ]
34. Hankin BL, Mermelstein R, Roesch L. Sex differences in adolescent depression: Stress exposure and reactivity models. Child Development 2007;78:279–295. [ Links ]
NOTA
* Artículo sin conflicto de intereses














