Serviços Personalizados
Journal
Artigo
Indicadores
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Salud mental
versão impressa ISSN 0185-3325
Salud Ment vol.31 no.2 México Mar./Abr. 2008
Artículo original
Terminal versus non–terminal care in physician burnout: the role of decision–making processes and attitudes to death
Bernardo Moreno–Jiménez,1 * Raquel Rodríguez–Carvajal,1 Eva Garrosa Hernández,1 Ma. Eugenia Morante Benadero1
1 Dpto. Psicología Biológica y de la Salud , Facultad de Psicología, Universidad Autónoma de Madrid, España.
*Correspondencia:
Benardo Moreno–Jiménez.
Carretera Colmenar Viejo,
Km. 15. 28049,
Madrid, Spain.
correo electrónico: bernardo.moreno@uam.es
Recibido primera versión: 4 de mayo de 2007.
Segunda versión: 1 de noviembre de 2007.
Aceptado: 12 de noviembre de 2007.
Abstract
Introduction
Physicians are often overloaded with high demands of patient care in an environment where organizational resources are frequently scarce, leading to occupational stress and physician burnout. When physicians suffer from these disorders, the potential negative influence on patient care is likely to be much greater and they are more prone to make errors of judgment in decision–making processes.
Some authors have proposed that physicians perceive decision–making as the main stressor, especially in chronic and terminal care. Caring for the dying is a remarkably stressful work. Many physicians feel helpless in the face of a patient's struggle with terminal illness. In this context, some questions arise: What is the interplay role of attitudes to death in decision–making processes in physicians' suffering from burnout? Are there any differences according to attitudes to death, target patients (i.e., terminal patients), or the classic sociodemographic variables? To what extent?
This study has attempted to examine these differences in the burnout process in physicians attending adult patients versus children, and terminal versus non–terminal cases, considering also the decision–making process and physicians' attitudes to death; to determine the core personal variables implied in this process, and to identify educational opportunities to improve physicians' well–being.
Method
A total of 130 physicians working in six general hospitals and two health centers in downtown Madrid completed and returned the questionnaire (response rate 72.2%). The sample resembles the overall area population in age distribution as well as in health status and sociodemographic characteristics. Participation was voluntary and anonymous; no incentives were offered to participants.
Results
Results suggested that the effects of burnout have more to do with chronic and terminal care than with the classic sociodemographic variables. Among the univariate tests for the first criterion variable doctors attending child versus adult patients, only avoidance of death was significantly higher in pediatricians. Univariate tests for scores of physicians working with terminal versus non–terminal patients (the second criterion variable) revealed significant effects for two of the ten variables. Physicians who attended terminal patients had higher exhaustion scores and lower scores in acceptance of death. Taking together both criterion variables, pediatricians' self–reports revealed significantly lower acceptance of death scores in the terminal care condition, whereas physicians working with adult patients had a significantly higher fear of choice scores in the terminal care condition. Additionally, through hierarchical regression analyses, anxiety about the decision–making process was the main precursor of burnout, controlling for age, gender and terminal versus non–terminal care of child versus adult patients. Attitudes to death, that is, acceptance or avoidance of death, were revealed as moderators of the relationship between decision–making processes and burnout.
Conclusions
Findings are discussed concerning the burnout process and the need for educational interventions in death and communication. The results were in keeping with the contention that, during explorations of career choice and even in the admission process, understanding of what the helping role implies should be increased, and the personal variables that are necessary to increase physicians' performance and well–being should be explicitly identified.
Key words: Burnout, physicians, decision–making, attitudes to death, chronic care.
Resumen
Introducción
Como grupo profesional los médicos enfrentan frecuentemente una sobrecarga laboral con elevadas demandas en el cuidado de los pacientes y en un entorno en que muchas veces faltan recursos organizacionales. En ocasiones, lo anterior conduce al estrés ocupacional y al desgaste profesional (burnout). Actualmente, desde una perspectiva psicosocial y procesual, el síndrome del desgaste profesional se ha conceptualizado como una respuesta al estrés laboral crónico que se desarrolla por la interacción de características del entorno laboral y características personales. Como consecuencia, la presencia del desgaste profesional facilita el error médico, lo que, a su vez, contribuye a todo tipo de consecuencias negativas en el cuidado del paciente y, principalmente, en los procesos de toma de decisiones. Algunos autores han planteado la toma de decisiones como el principal estresor percibido en los médicos, principalmente en el cuidado crónico y terminal. El cuidado paliativo en el paciente terminal se convierte entonces en un trabajo potencialmente estresante. Muchos médicos se sienten impotentes ante la agonía de un paciente en fase terminal. En este contexto surgen algunas interrogantes: ¿Cuál es el papel de las actitudes ante la muerte en el complejo proceso de toma de decisiones en los médicos desgastados profesionalmente? ¿Existen diferencias procesuales en función de las actitudes hacia la muerte, el tipo de pacientes (v.gr., pacientes terminales) o las clásicas variables sociodemográficas relacionadas con el síndrome? ¿En qué medida?
Este estudio intentará examinar estas posibles divergencias en el proceso de desgaste profesional en médicos que trabajan con adultos versus niños, en fase terminal versus no terminal, considerando asimismo los procesos de toma de decisiones y las actitudes hacia la muerte. De este modo se podrán determinar las variables personales implicadas en el proceso, que permitan desarrollar posteriormente programas de prevención y formación para aumentar el nivel de bienestar de estos profesionales.
Método
Un total de 130 profesionales médicos, que trabajaban en seis hospitales generales y en dos centros de salud de Madrid capital, rellenaron y devolvieron el cuestionario (tasa de respuesta de 72.2%). La muestra obtenida fue semejante en edad, estado de salud y otras características sociodemográficas a la población de referencia. La participación fue totalmente voluntaria y anónima sin ningún tipo de incentivos por la colaboración.
Resultados
Los resultados obtenidos sugieren que los efectos del desgaste profesional se encuentran más relacionados con el cuidado crónico y terminal que con las clásicas variables sociodemográficas. Mediante análisis univariados se observó que los médicos pediatras frente a los que trabajaban con adultos mostraron niveles significativamente mayores de actitudes de evitación ante la muerte. En cuanto a los médicos que trabajaban con pacientes terminales versus no terminales, los análisis univariados mostraron efectos significativos en dos variables. Aquellos médicos que atendían a pacientes en fase terminal mostraron niveles significativamente mayores de desgaste emocional y menores niveles de aceptación de la muerte. Finalmente, al cruzar ambas variables (médicos que atendían a pacientes niños vs. adultos, terminales vs. no terminales), los pediatras obtuvieron niveles significativamente menores de aceptación de la muerte en los niños en fase terminal, mientras que los especialistas que trabajaban con adultos en fase terminal puntuaron significativamente más alto en la dimensión de miedo a la elección del cuestionario de toma de decisiones. Por otra parte, mediante análisis de regresión jerárquica, la ansiedad ante la toma de decisiones resultó ser el principal precursor del desgaste profesional, una vez controlados los efectos debidos a la edad, el género y el grupo médico (atención a niños vs. adultos, terminales vs. no terminales), mientras que las actitudes ante la muerte (v.gr., aceptación o evitación de la muerte) mostraron un efecto moderador en la relación entre los procesos de toma de decisiones y el desgaste profesional.
Conclusiones
Los principales resultados encontrados con respecto al estudio del proceso de desgaste profesional reflejan la necesidad de realizar programas de prevención y formación en el afrontamiento de la muerte. Los resultados son congruentes con las reflexiones realizadas principalmente en contextos de formación y procesos de admisión donde se enfatiza la necesidad de aumentar la comprensión del rol de ayuda y su repercusión, e identificar explícitamente aquellas variables personales que permitan aumentar los niveles de rendimiento y bienestar de los profesionales médicos.
Palabras clave: Desgaste profesional, médicos, toma de decisiones, actitudes ante la muerte, cuidado crónico.
INTRODUCTION
The medical profession is generally considered to be quite stressful, and fundamental changes in the organization, financing and delivery of health care have brought about additional problems.1 Demands at work, such as restrictions on time and resources, have increased; at the same time, physicians have had to deal simultaneously with many different types of illnesses and heavy patient demands.2 Likewise, influences over one's work and intellectual stimulation from work have decreased. This situation leads to a sense of diminished control over both administrative and clinical aspects of the practice, wich results in turn in negative attitudes about the practice environment, and facilitate the development of the burnout syndrome. Burnout is considered as an effect of the interaction with recipients, mainly in human services, characterized by emotional exhaustion, depersonalization and decreased personal accomplishment. Emotional exhaustion measures <<feelings of being emotionally overextended and exhausted by one's work>>. Depersonalization measures <<an unfeeling and impersonal response toward recipients or one's service, care, treatment, or instruction>>, and the third dimension, reduced personal accomplishment, measures <<feelings of competence and successful achievement in one's work with people>>.3 Prevalence of burnout among physicians has been reported in the range of 12–30%, depending on the measure used.4 In addition, several studies report that physicians have higher rates of mortality, suicide, psychiatric admissions and general physical illness than the general population.4
When physicians suffer from these disorders, then the potential negative influence on patient care is likely to be much greater, as they are more likely to treat patients poorly, both medically and psychologically, and they are more prone to make errors of judgment.1,5 In this context, physicians can make mistakes in decision–making processes, especially in relation to the type of ethical dilemmas involved in the use of new antibiotics, artificial nutrition, cardiopulmonary resuscitation, mechanical ventilation, and so on. Decision–making in clinical services is complex, involves intuitive and rational factors, and requires going beyond the disease itself and taking into account value judgments, as well as social, psychological and moral factors. Making this kind of decisions may cause anxiety, and there are often high associated risks. Some authors, such as Firth–Cozens,5 have proposed that physicians perceive decision–making as the main stressor, especially in chronic and terminal care.
Caring for the dying is a remarkably stressful work. Many physicians feel helpless in the face of a patient's struggle with terminal illness. Medical students also experience patients deaths as emotionally draining even when they were not close to the patients.6 One common response is simply to disappear, leaving the care of such a patient in the hands of other members of the health care team or to the family. Another common response to the physician's feelings of helplessness is a need to take control, to <<fix it>>. Doctors tend to be most comfortable when they can <<do>> something: prescribe medications, order tests or even develop new communication skills. Some studies have examined these doctors' attitudes to death,1 and dying.7
Because of the fact that intervention protocols exist, the relevance of studying decision–making processes on physician burnout may be related to complex situations quite often related in turn to diverse ethical dilemmas, from using different techniques to deadling with death in children. In this context, some questions arise: What is the interplay role of death attitudes in the complexity of decision–making processes on physicians suffering from burnout? Are there any differences according to death attitudes, the target patients (i.e. terminal patients) or the classical sociodemographic variables? To what extent?
Previous research on physician burnout has emphasized the importance of these sociodemographic, organizational and personality variables. In the context of sociodemographic variables, Deckard et al.8 found that emotional exhaustion was higher in younger physicians and female physicians, groups previously noted by Gerrity et al.8 to be more affected by uncertainty. This suggests that consistently high levels of stress from uncertainty may contribute to physician burnout. At an organizational level, some of the early research on medical burnout has focused on the relative stressfulness according to non–critical care versus critical care settings.7 Demands cited by workers as problematic included working with families and providing psychological support, certifying patients as dead, dealing with drug users, dealing with other agencies and the youth of their patients. Terminal care exposes practitioners to patients who may become sicker and die. Physicians' emotional reactions to patient death affect the personal lives of physicians,9 and increase the likelihood of suffering burnout.10 As regards personality variables, few, if any, empirical studies have examined the relationship between burnout, attitudes to death, and decision–making processes in critical care versus non–critical care.
In an ever–changing environment of hospital restructuring and reengineering, issues of medical burnout demand our attention. Measuring burnout among physicians is important, because physicians' well–being has implications for the stability in the health care provider workforce and for the quality of care it provides. However, many aspects of this process are still poorly understood. Bearing in mind the caveats noted above, the results of previous research were used as a guiding model in our selection of the criterion variables. This model proposes physician burnout as an important effect on decision–making process, and death attitudes as intervening variables between decision–making and burnout. Terminal versus non–terminal care, together with child versus adult patients, served as criterion variables. The primary objective of the present study was to determine whether decision–making processes, death attitudes and burnout differ in physicians treating terminal versus non–terminal and child versus adult patients. A secondary objective was to study how decision–making processes and death attitudes are associated with physician burnout. We hypothesized that death attitudes moderate the effects of decision–making process in physician burnout.
METHOD
Participants and recruitment
The sample resembles the overall area population in age distribution as well as health status and sociodemographic characteristics. Participation was voluntary and anonymous, and no incentives were offered to participants. All those who participated read and signed an information sheet indicating that participation was voluntary. Meetings with representatives of management and staff provided identification of the kind of workers needed for this study. A total of 130 physicians, working in six general hospitals and two health centers in downtown Madrid, filled out and returned the completed questionnaire (response rate 72.2%). This response rate is quite good when compared with other research using institutional populations and no incentives, and is characteristic of physician surveys.11 The sample consisted of 61 male (46.9%) and 69 female (53.1%) physicians. Mean age was 39 years (SD=10.3), with a mean of 13 years (SD=10.0) work experience. As regards the population of patients with whom they worked, 62 (47.7%) worked with terminal patients and the remaining 68 (52.3%) with non–terminal patients. Specifically, 32 physicians (24.6%) worked with non–terminal children, 31 (23.8%) worked with terminal children, 36 (27.7%) were treating non–terminal adults, and the remaining 31 (23.8%) worked with terminal adults. Other demographic and work–related information was gathered on marital status, medical experience, and several work–related factors, such as number of patients seen per shift.
Questionnaires
• Burnout. Burnout was measured using the Spanish version of the Maslach Burnout Inventory–Human Services Survey, MBI–HSS, which consists of three dimensions: emotional exhaustion (nine items), depersonalization (five items), and personal accomplishment (eight items).12 Factor analysis established the structure of three factors that accounted for 44% of the total variance. Internal consistency for all three scales was quite good: emotional exhaustion α=.90, depersonalization α=.79 and personal accomplishment α=.71. Items assess how frequently respondents experience thoughts and feelings related to the burnout components on a 7–point scale from 0 (never) to 6 (daily). Sample item: <<I feel emotionally drained by my work>>.
• Decision–making. Thirty–four items from the Decision Making Scale13 were used to measure decision–making processes on a 4–point scale from 1 (always) to 4 (never). Main component factor analysis with varimax rotation was used to examine the factor structure. The factor analysis identified five factors accounting for 59.2% of the total variance. The five factors corresponded respectively to the <<anxiety in decision–making>>, <<diffusion of responsibility>>, <<rumination>>, <<indecision>>, and <<fear of choice>> subscales of the DMS. A reliability analysis of these derived factors revealed an excellent internal consistency, with Cronbach's alphas ranging from .69 to .86 and the majority exceeding .80. Sample items: anxiety in decision–making: <<Decision–making causes me real anxiety>>; diffusion of responsibility: <<I like to give my opinion but let others take the decision>>; rumination: <<When I have to take a decision, I rack my brain for several days to decide among the options>>; indecision: <<When I take a decision, I always think I should have chosen an other option>>; fear of choice: <<I am afraid of making the wrong decision>>.
• Attitudes to death. Attitudes to death were measured using the Death Attitudes Profile Revised.14 The DAP–R measures attitudes to death by asking respondents to indicate their level of agreement using a 7–point Likert scale ranging from <<strongly disagree>> to <<strongly agree>>. In addition, half of the items are reverse–scored. Before performing the factor analysis, the original data set of 32 items was reduced to adapt the questionnaire to the aims of this study and the sample characteristics. The factor–analyzed DAP–R has two subscales that accounted for 44.71% of the total variance: avoidance of death (four items) and acceptance of death (five items). The avoidance of death scale includes items such as <<Whenever the thought of death enters my mind, I try to push it away>>, and the acceptance of death scale includes items such as <<Death should be viewed as a natural, undeniable and unavoidable event>>. Internal consistency for the current sample was .69 for avoidance of death, and .75 for acceptance of death.
RESULTS
Descriptives, correlations, and MANOVA
Table 1 shows the descriptives and the intercorrelations of the variables in this study.
In order to test whether or not physicians who treated different types of patients differed in the study variables, a MANOVA was performed to compare these two criterion variables: the scores of doctors attending child versus adult patients with the scores of those working with terminal versus non–terminal patients. All ten dependent variables were included: the three burnout dimensions, avoidance and acceptance of death and the five decision–making dimensions, using SPSS 13 (table 2). The multivariate ANOVA revealed significant effect (F(10) = 2.3, p < 0.018).
Among the univariate tests for scores of doctors attending child versus adult patients, only affected frequency reports for one of the ten variables, avoidance of death (F(1) = 6.2, p < 0.014). Pediatricians had higher avoidance of death ratings than physicians treating adult patients (t = 2.49, p < 0.018). No significant main effects were found for the rest of the variables.
Univariate tests for scores of those working with terminal versus non–terminal patients revealed significant effects for two of the ten variables. The strongest effect emerged for emotional exhaustion (F(1) = 5.5, p < 0.021). Physicians who attended terminal patients had higher exhaustion scores than those working with non–terminal patients (t = 2.28, p < 0.029). The effects for depersonalization and personal accomplishment were not significant. This univariate test also showed a significant effect on acceptance of death (F(1) = 4.4, p < 0.037), and the effect was in the predicted direction, with physicians treating terminal patients having lower scores in acceptance of death than those who treated non–terminal patients (t = –1.98, p < 0.047). No further significant main effects were found.
Among the ten variables, two significant results emerged through the univariate tests for both criterion variables (physicians attending adults vs. children patients, and terminal vs. non–terminal ones): acceptance of death and fear of choice (F(1) = 9.3, p < 0.003, and F(1) = 4.8, p < 0.031). For acceptance of death, the terminal factor had no effect on physicians treating adult patients, which were high in both terminal and non–terminal patient conditions (t = 0.77, p = 0.437), but did affected pediatricians' self–reports, which gave significantly lower acceptance of death scores in the terminal condition (t = –3.22, p < 0.003). Nor was there any effect of the terminal factor on pediatricians' fear of choice scores, which were high in both conditions (t = –0.86, p = 0.387). However, there was an effect on physicians working with adult patients, which gave significantly higher fear of choice scores in the terminal care condition (t = 2.15, p < 0.049).
Hierarchical multiple regression
First, we analyzed the hypothesis of homocedasticity, independence, and colinearity. To explore the homocedasticity (homogeneity of variance), we looked at the scatter diagrams of standardised residuals against prognosticated standardised values, and they did not show any deviation in form. Furthermore, the selected models appear to be valid because these graphics did not show any regular shape. Independence was tested by the Durbin–Watson statistic, which uses Studentized residuals. The Durbin–Watson statistic should be between 1.5 and 2.5 for independent observations. Finally, multicollinearity among independent variables was investigated by collinearity diagnostics (e.g. tolerance and variance inflation factor). None of the regression models were disturbed by multicollinearity.
Our two main hypotheses focused on the relationship between the decision–making processes of physicians and their death attitudes, on the one hand, and burnout, on the other hand. Furthermore, we expected both main effects and interaction effects with death attitudes. To determine possible interaction effects, the independent variables were introduced into the equation in five steps.15 In the first step, age, gender, and medical group (physicians attending adults vs. children patients, and terminal vs. non–terminal ones) were entered to control for possible confounding effects. Step two involved the entry of the five dimensions of decision–making processes. In the third step, attitudes to death (i.e., avoidance and acceptance of death) were entered. In the fourth and fifth steps, the ten interaction terms of the five decision–making processes with both avoidance and acceptance of death were entered. To avoid possible problems with multicollinearity, the variables were centered around zero before calculating their crossproduct terms.
Table 3 shows the results of the hierarchical regression analyses. After controlling for gender, age, and medical group, two main effects for exhaustion were found as it was hypothesized: anxiety in decision–making and medical group. Anxiety in physicians' decision–making is related to more feelings of exhaustion. The relationship between medical group and emotional exhaustion was discussed here in before.
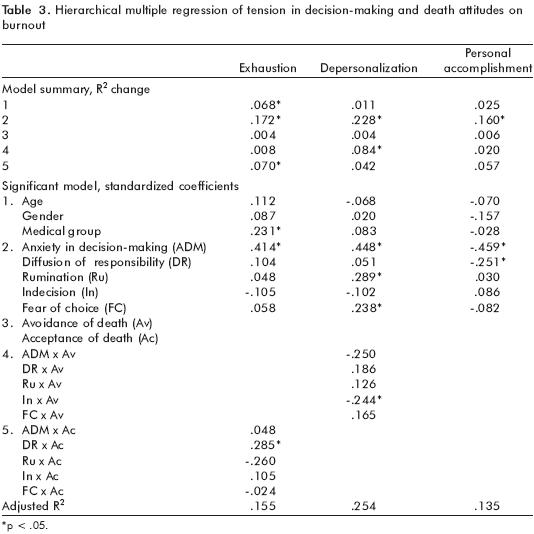
Furthermore, the relationship between physicians' decision–making processes and exhaustion (model 5, table 3) is qualified by a significant interaction: diffusion of responsibility with acceptance of death. Figure 1 shows that under conditions of less diffusion of responsibility, more acceptance of death is related to less exhaustion of physicians. However, under similar conditions of less diffusion of responsibility, less acceptance of death is related to more exhaustion. According to Chaplin16 and Frazier, Tix, and Barron,17 effect sizes for interactions are generally small and small corresponds to an R2 value of .02 or smaller. This analysis has been argued (e.g., 1, 13) as the preferred statistical strategy for identifying the presence and nature of moderating effects. The sample size of this study (i.e., n = 130) was sufficient to detect a moderate effect size of .129.18 With an alpha level of .05, and a non–centrality parameter lambda of 16.893, the power of the interaction was .89.19

There are also main effects of decision–making processes on depersonalization. The decision–making processes of physicians who experienced more depersonalization are related to more anxiety in decision–making, less rumination, and more fear of choice. The relationship between these decision–making processes and depersonalization (model 4, table 3) is qualified by a significant interaction: indecision with avoidance of death. Figure 2 shows that under conditions of less indecision in physicians, less avoidance of death is related to less depersonalization. However, under similar conditions of less indecision in decision–making, more avoidance of death is related to more depersonalization. According to the power test of this interaction, the sample size of this study (i.e., n = 130) was sufficient to detect a moderate to large effect size of .340.18 With an alpha level of .05, and a non–centrality parameter lambda of 44.263, the power of the interaction was .99.19

Experiencing anxiety in decision–making was also related to less personal accomplishment. In addition, more diffusion of responsibility was related to more personal accomplishment. Neither the death attitudes of physicians nor the interaction effects added significant features to the model.
CONCLUSIONS
The purpose of this study was to explore the correspondence of physician staff burnout, decision–making, death attitudes and care to find out the core personal variables implied on this process and to identify educational opportunities for improving physician well–being. Firstly, the findings presented here add weight to know the role of medical perceptions and attitudes in decision–making processes, especially in chronic and terminal care, to explain physician burnout. These perceptions and attitudes concern not only the terminal/non–terminal care dichotomy; they also have different effects depending on whether patients are children or adults. Physicians often have to accept failure, continued suffering on the part of patients and deaths. Thomas Mann once wrote <<A man's death is more the survivor's affair than his own>>.20 This is especially true in the death of a child, whose doctors may be deeply affected, and experience heavy emotional burdens that may create barriers and possible distancing from families and other similar patients.21 In this sense, the results of this study revealed attitudes to death as core factors in these situations, moderating the likelihood of suffering physician burnout above all in the care of terminally–ill children.
Physicians must accept that death is an intrinsic part of the profession, since treatment failures are not altogether uncommon.1 Even worse, active decisions made by the physician may result in the death of the patient. The results of the MANOVA confirmed the importance of these considerations in the care of adult chronic patients, where deciding between new treatments with unpredictable reactions and palliative treatments led to high fear of choice scores. In this context, physicians must learn to function at an optimal emotional and intellectual level in spite of such strong stressors.
Turning now to our results on the role of decision–making in burnout process, we found that anxiety in decision–making is the main precursor of burnout, controlling for age, gender, and medical group (physicians attending adults vs. children patients, and terminal vs. nonterminal ones). Decision–making involves not only medical experience and other rational factors, but also value judgments, moral factors and ethical dilemmas that go into complex decision–making processes which may lead to anxiety and sometimes high risks, such as risk of burnout. In addition, the advancement of complementary (alternative) medicine and easier access to information through Internet has increased medical knowledge and patients' interest in playing a greater part in decision–making processes, thus calling physician decisions more into question.22 Physicians need to develop advanced skills in order to restore patient confidence and decrease anxiety in decision–making.
The variables 'indecision', 'uncertainty' and 'intolerance of ambiguity' in decision–making processes are used to define a tendency for perceiving ambiguous situations as a source of stress. Gerrity et al.8 proposed a conceptual model that takes into account patient, physician and organizational characteristics in the explanation of decision–making process. They assumed that these interact with physicians' uncertainty as the core factor in explaining differences among physicians. This assumption is ratified by our results. The hierarchical regression analyses revealed this indecision as an important variable related to depersonalization, with avoidance of death attitude as a moderator.
The findings presented here provide a starting point for addressing the core factors for prevention and intervention in the physician burnout process. Early intervention with resident physicians and medical units may help avert more serious long–term problems. Nevertheless, there is a positive side to many of these findings. First, our results suggest that personal factors do affect the experience of burnout, though very few empirical studies in the area of physician burnout have adopted an attitudinal perspective. The present study employed a moderating model whereby burnout is seen as a strain consequence moderated by individual characteristics. Second, the fact that some physicians report feeling burnout suggests that it may be possible to identify those at high risk and intervene before they suffer more serious personal and professional consequences. Third, controlling these medical stressors and moderators, it may also be possible to identify individuals most likely to be adversely affected. Finally, based on these empirical results, we should develop strategies to prevent physician burnout through a curriculum content that allow medical students to be trained in coping of death, handling emotions, decision–making and other regulation processes involved in physician daily work life. In this sense, a number of curricula and initiatives have been developed to address burnout either exclusively or as part of a more comprehensive program resident/fellow wellness.23–26
Therefore, in order to prevent the negative effect of stressors, enhancement initiatives should be considered at the individual, group and structural levels. Healthier work conditions and better resources for physicians –such as improved communication and social support–, which will help them deal with daily irritants, should be identified.
The considerations reported here are consistent with the results of a study by Arnetz.1 This author proposes healthier ways for managing the stress of everyday medicine through physicians' focus groups in discussion sessions where they identify positive coping strategies and learn mental imaging. However, structural changes in the work environment at the organizational level would seem to be more effective. For example, increased professional autonomy and decision latitude could be provided through administrative changes affecting task structure and control over resources.4 It has been demonstrated that a systematic approach to reducing organizational stress results in decreased depression scores and increased mental and physiological well–being among physicians.1
The limitations of this study must also be pointed out. First, our independent variables and outcome measures were based on self–reports, as in the majority of burnout and stress studies.27 Self–report data can be contaminated by common method variance, since the dependent and independent variables are based upon a single information source, i.e., the participants. Future research should work with additional measures, such as psychophysiological variables. Second, the analyses in the current study are correlational, and hence do not confirm causality. Furthermore, since the design of the study was cross–sectional, more complex forms of non–recursive linkages could not be examined. In this sense, a longitudinal study would be desirable to comprehend the dynamics on the relationship between burnout and the moderated effect of individual characteristics through time, as a baseline to control the effect of prevention and intervention programs. Future longitudinal research will allow us to examine the effectiveness of these programs controlling by job satisfaction, motivation, workload or social support among others. It would be also interesting to gather physicians' suggestions with a qualitative methodology to enhance the limited knowledge of their current situation considering, for example, the impact of new technologies on their job. Third, although our response rate was quite good when compared with other research using institutional populations and no incentives,28 the fact that we did not know whether responders differed from non–responders may weaken the generalizability of these results.
One of the reasons why people choose to become medical doctors is that they want to help others. There is evidence that choosing to be a health worker is at least partly a reflection of one's early experience. Moreover, some longitudinal studies have found that this early experience also has an effect upon a medical doctor's well–being.29 These results are in keeping with the contention that although there is little that can be done policy–wise about early family relationships, there should be increased understanding of the helping role during explorations of career choice.
In fact, physicians often have to accept failures, continued suffering on the part of patients and deaths. Of the previous studies that have examined educational interventions on communication and death, few have addressed interventions for pediatrics residents.22 This knowledge gap must be filled through future empirical research. Although death remains one of the common threads binding all living things, there is far from a single approach to our understanding of the topic. Terminal care can also be remarkably rewarding, since there are deeper challenges, which require the presence of physicians as human beings. It should be borne in mind that in their clinical decision–making processes, physicians draw on all their knowledge and experience, and a complex reasoning model is used to reach a final decision. A poor psychosocial work environment may have a negative influence on this delicate decision–making process, especially in terminal care.
REFERENCES
1. Arnetz BB. Psychosocial challenges facing physicians of today. Soc Sci Med 2001;52:203–213. [ Links ]
2. Bachman KH, Freeborn DK. HMO physicians' use of referrals. Soc Sci Med 1999;48:547–557. [ Links ]
3. Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd. ed. Palo Alto, CA: Consulting Psychologists Pr; 1996. [ Links ]
4. Schmoldt RA, Freeborn DK, Klevit HD. Physician burnout: recommendations for HMO managers. HMO Pract 1994;8:58–63. [ Links ]
5. Firth–Cozens J. Interventions to improve physicians' well–being and patient care. Soc Sci Med 2001; 52:215–222. [ Links ]
6. Rhodes–Kropf J, Carmody SS, Seltzer D y cols. <<This is just too awful; I just can't believe I experienced that...>>: Medical students' reactions to their <<most memorable>> patient death. Acad Med 2005;80:634–640. [ Links ]
7. Gordon GH: Care not cure: dialogues at the transition. Patient Educ Couns 2003;50:95–98. [ Links ]
8. Gerrity MS, Devellis RF, Earp JA. Physician's reactions to uncertainty in patient care. Med Care 1990;28:724–736. [ Links ]
9. Jackson V, Sullivan AM, Gadmer NM et al. <<It was haunting ...>>: Physicians' descriptions of emotionally powerful patient deaths. Acad Med 2005;80:648–656. [ Links ]
10. Bonde L. The effects of grief and loss on decision making in HIV–related psychotherapy. In: Anderson JR, Barret RL (eds.). Ethics in HIV–related psychotherapy: Clinical decision making in complex cases. American Psychological Association; 2001: p. 83–98. [ Links ]
11. Rohland BM, Kruse GR, Rohrer JE. Validation of a single–item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health 2004;20:75–79. [ Links ]
12. Maslach C, Jackson SE. Maslach Burnout Inventory Manual (2nd. Ed.). Palo Alto, CA: Consulting Psychologists; 1986. [ Links ]
13. Maciá A, Barberó I, Pérez–Llantada C et al. Estudio interno de una escala de toma de decision: E.T.D. Revista de Psicología General y Aplicada 1996;49:267–278. [ Links ]
14. Wong PTP, Reker GT, Gesser G. Perfil revisado de actitudes hacia la muerte: Un instrumento de medida multidimensional. In: Neimeyer RA, editor. Death anxiety handbook. Research, instrumentation and application. Washington & Londres: Taylor & Francis; 1997. [ Links ]
15. Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park: Sage; 1991. [ Links ]
16. Chaplin WF. The next generation of moderator research in personality psychology. J Pers 1991;59:143–178. [ Links ]
17. Frazier PA, Tix AP, Barron KE. Testing moderator and mediator effects in counseling psychology research. J Couns Psychol 2004;51(1):115–134. [ Links ]
18. Cohen J, Cohen P. Applied multiple regression/correlation analyses for the behavioral sciences. Hillshade, New Jersey: Lawrence Erlbaum Associates, Publishers; 1983. [ Links ]
19. Cohen J, Cohen P, West SG et al. Applied multiple regression/correlation analysis for the behavioral sciences (3rd Ed.). Mahwah, NJ: Erlbaum; 2003. [ Links ]
20. Mann T. The magic mountain: A novel. New York: A. Knopf; 1995. [ Links ]
21. Serwint JR, Rutherford LE, Hutton N, et al. <<I learned that no death is routine>>: description of a death and bereavement seminar for pediatrics residents. Acad Med 2002;77:278–284. [ Links ]
22. Greenberg LW, Ochsenschlager D, O'Donnel R, et al. Communicating bad news: a pediatric department's evaluation of a simulated intervention. Pediatrics 1999; 103:1210–1217. [ Links ]
23. http://www.ama–assn.org/ama/pub/category/10971.html [ Links ]
24. http://www.lifecurriculum.info [ Links ]
25. http://www.hsc.usf.edu/housestaff/assistance.htm [ Links ]
26. http://www.ecfmg.org/acculturation/ian.html [ Links ]
27. Schaufeli WB, Enzmann D. The burnout companion to study and practice: A critical analysis. London: Taylor & Francis Ltd; 1998. [ Links ]
28. Sudman S, Bradburn NM. Asking questions: a practical guide to questionnaire design. San Francisco: Jossey–Bass; 1988. [ Links ]
29. Brewin CR, Firth–Cozens J. Dependency and self–criticism as predicting depression in junior doctors. J Occup Health 1997;2:242–246. [ Links ]














