Introduction
We are currently experiencing one of the most intense pandemics humanity has ever registered, which has caused a large number of infections and deaths that have impacted the global health, economy and society. According to reports in the literature, this pandemic originated at the end of December 2019 in Wuhan, Hubei Province, China. It is a zoonosis that caused an outbreak of pneumonia of unknown aetiology, produced by a novel beta-coronavirus called nCov-2019, officially known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1,2
SARS-CoV-2 belongs to the order Nidovirales, family Coronaviridae, subfamily Orthocoronavirinae, genus Betacoronavirus; it exclusively infects mammals and causes infections mainly in the respiratory and gastrointestinal tract.3,4 It is an enveloped virus with a positive-sense, single-stranded RNA genome.5 Regarding its origin, genome sequencing studies show 87.99% similarity with bat SARS-like coronavirus (CoVZC45), 79% similarity with SARS-CoV, and 50% similarity with MERS-CoV.6 The life cycle of SARS-CoV-2 in the host consists of attachment, penetration, biosynthesis, maturation, and release, and it contains the structural proteins spike (S), membrane (M), envelope (E), and nucleocapsid (N). The most immunogenic proteins of the virus are S and N.7 Protein S is a class I fusion protein consisting of a transmembrane trimer, the second domain of which is the receptor binding domain (RBD) that binds to the angiotensin II converting enzyme (ACE2) of the lungs, heart, ileus, kidneys, and bladder.8 This protein has two subunits: S1, the amino-terminal part, and S2, the carboxyl-terminal part, which is a key target for the development of vaccines and therapeutic antibodies and for the development of diagnostic and prevention strategies, as it determines the entry of the virus into host cells and constitutes the main region that neutralizes antibodies.9,10,11
The disease caused by the novel coronavirus 2 is called Covid-19, manifesting as a severe acute respiratory syndrome (SARS-CoV-2).12,5 From December 2019 to February 2021, coronavirus 2 has infected approximately 120 million people and caused nearly 2.6 million deaths worldwide, constituting a serious threat to public health.13
The emergence of an infectious disease comprises three vital elements: the source of infection, the route of transmission, and the susceptible population.14 The main source of SARS-CoV-2 infection is infected patients, who produce an enormous amount of viruses in the upper respiratory tract during the prodromal period.15 These patients can transmit the infection starting in the viral incubation period (with mild symptoms), which can be very long (1-24 days), making it difficult to track infections.16 Another source of infection is asymptomatic carriers who acquired the virus but do not exhibit clinical manifestations.17 Thus, understanding the transmissibility of SARS-CoV-2 is crucial to predict the course of the pandemic and the probability of sustained transmission.18
The immune response generated against SARS-CoV-2 is humoral and cellular. Proinflammatory cytokines, T cells and B cells are produced, activating the latter to transform into antibody-producing plasma cells.19 The antibody response is of particular interest for the following reasons: 1) it is a parameter of the transmissibility of the infection in the population; 2) it serves to identify cases and past contacts; 3) it is an indicator of natural protection against infection, and 4) it could be an alternative therapy in patients with severe cases of pneumonia.20,21,22,23
In this study, our objective was to determine the levels of IgG anti-S1 protein of SARS-CoV-2 (anti-SARS-CoV-2 IgG) in sera from healthy Mexican subjects (blood donors) not exposed to the virus, collected before the pandemic, and in sera of Mexican asymptomatic subjects for Covid-19 (blood donors and patients with diverse neurological diseases), collected during the pandemic, in order to determine the degree of viral spread and analyse the individual levels of IgG anti-S protein of SARS-CoV-2 and their possible association to demographics data, comorbidities, and exposure to Covid-19 patients.
Materials and methods
Study participants
This was a cross-sectional study in which sera from healthy blood donors and neurological patients asymptomatic for Covid-19 from the National Institute of Neurology and Neurosurgery of Mexico, collected before and during the pandemic, were analysed. The pre-pandemic samples were collected from January 2018 to December 2019 and came from the blood bank donor serum library, whose operation and disposal of biological material is governed by the Official Mexican Standard 253-SSA1-2012.24 The participants of this stage agreed that their serum was part of the bank and that it could be used in subsequent research studies. The pandemic samples were collected from October to December 2020 and came from blood donors and neurological patients who came to the Clinical Laboratory for routine studies. Among the patients, the most common diagnoses were central nervous system tumours, epilepsy, cerebrovascular events, dementia, depression, headache, and neuropathy. A clinical questionnaire was applied to all participants in the pandemic sample to rule out Covid-19 symptoms (fever, cough, laboured breathing, general weakness, fatigue, headache, muscle ache, joint pain, painful swallowing, runny nose, appetite loss, nausea, vomiting, diarrhoea, or altered mental state) and to determine whether they had had contact with positive cases of Covid-19, as well as their comorbidities (diabetes mellitus, arterial hypertension, asthma, and thyroid disorders). Sociodemographic data of the participants (sex, age, education, occupation, marital status, immunization schedule, history of drinking alcohol, smoking and drug addiction, and place of origin) were recorded. Patients with a previous diagnosis of Guillain-Barré syndrome (who could have an early-stage form of Covid-19) were excluded. All participants provided written informed consent. The study was approved by the Institutional Research, Bioethics and Biosafety Committees under registration number 86/20.
Enzyme immunoassay (ELISA)
The determination of anti-SARS-CoV-2 IgG antibodies was performed with a commercial kit (EUROIMMUN Medizinische Labourdiagnostika AG, https: www.euroimmun.com) according to the manufacturer’s instructions. We determined the optical density at 450 nm and calculated the ratio of the extinction values of the control or patient sample and the extinction value of the calibrator of the kit (which defines the upper limit of the reference range of uninfected individuals or cut-off value), interpreting the proportion obtained as follows: ≤1.1, negative; >1.1, positive. This corresponds to a sensitivity of 43.7% for confirmed positive patients with less than 10 days of infection and 94.4% for patients with infection for over 10 days. The specificity, with these same cut-off points, was 96.3% obtained in samples from healthy subjects of diverse age groups, patients with other human pathogenic coronaviruses, with common seasonal influenza, and with rheumatoid factors.
Before determining the serum antibodies of the collected samples, precision, sensitivity, and specificity studies were carried out to ensure the reliability of the reagents and the assay. The precision among runs performed on the same day and among runs performed on five separate days was determined using a positive external control (ACCURUN Anti-SARS-CoV-2 Controls Kit Series 2000, Seracare Life Sciences, USA) (diluted 1:10), according to guideline EP05-A3 of the Clinical and Laboratory Standard Institute.25 Differences in repeatability and between runs were determined, and the coefficients of variation of both parameters (within run precision, CVR; within lab precision, CVWL) were obtained by one-way analysis of variance. The observed values were lower (CVR= 1.78%; and CVWL= 3.23%) than those reported by the kit manufacturer (<12% and <15%, respectively).25 Both the sensitivity and specificity of the anti-SARS-CoV-2 ELISA were 100%, determined by contingency table analysis with the results of 7 sera from individuals diagnosed with Covid-19 (confirmed by PCR), an external positive control, 10 sera from healthy/non-Covid-19 subjects, and an external negative control, which were also run following the chemiluminescence method (Vitros SARS-CoV-2 IgG assay, Ortho Clinical Diagnostics, USA).
Statistical analysis
A descriptive analysis of the sample was performed based on the level of measurement of the variables, the proportions of positive anti-SARS-CoV-2 IgG antibodies in sera collected before and during the Covid-19 pandemic were determined, and their relationship with demographic and clinical variables were analysed. To compare the level of positivity, the means and standard deviations (SD) of the ratio of the extinction values of the patient sample and the extinction value of the kit calibrator were calculated among the samples with positive values (ratio >1.1). From these values, four groups were created: minus to 2.1 (≤ -1 SD); 2.2 to 4.5 (mean to -1 SD); 4.6 to 6.9 (mean to +1 SD), and 7.0 to the maximum value (≥ +1 SD). The comparisons were performed using the Chi-square difference test and the Jonckheere-Terpstra trend test was carried out, considering a p-value ≤0.05 as statistically significant. All analyses were performed using Stata 14.2.*
Results
We analysed 1 093 sera: 538 obtained from healthy donors before the pandemic; and 555 obtained during the pandemic (243, from healthy donors, and 312, from neurological patients) (table I). The percentage distribution of age from 36 to 59 years, secondary or higher education, sex, marital status, and occupation between the pre-pandemic and pandemic donors was similar; but it was higher in neurological patients with 60 or more years, divorced or widowed marital status, and homemaker occupation (p< 0.001). The percentage distribution of anti-SARS-CoV-2 IgG antibodies was considerably higher in pandemic donors (29.6%) and neurological patients (15.7%) than that in pre-pandemic donors (0.6%), in whom there were antibodies in only three out 538 cases (table II). The sample collection date of the positive subjects in the pre-pandemic sample was November 2018 and May and November 2019, which corresponded to a woman, aged 44 years, and two men, aged 45 and 28 years, respectively.
Table I Demographic data of pre-pandemic and pandemic participants, date of collection and origin of the samples. Mexico, January 2018 to December 2019
|
Sex and age of the participants and sample data |
Pre-pandemic participants (n= 538) |
Pandemic participants (n= 555) |
|
|
Donors |
Donors (n= 243) |
Neurological patients (n= 312) |
|
|
Women (n) |
223 |
97 |
190 |
|
Men (n) |
315 |
146 |
122 |
|
Age, mean ± standard deviation |
39.7 ± 11.9 |
36.1 ± 11.7 |
46.7 ± 16 |
|
Date of the sample collection |
1/1/2018-31/12/2019 |
1/10/2020-31/12/2020 |
|
|
Sample origin |
Blood bank |
Clinical laboratory |
|
Table II Percentage distribution of demographic characteristics of participants and of the presence or absence of anti-SARS-CoV-2 IgG antibodies in sera obtained before and during the pandemic. Mexico, January 2018 to December 2019
|
Demographic characteristics |
Pre-pandemic donors n= 538 |
Pandemic |
p value |
||
|
Donors n= 243 |
Patients n= 312 |
||||
|
Age group |
17-25 |
12.8 |
21.0 |
11.9 |
<0.001 |
|
26-35 |
28.1 |
32.5 |
14.7 |
||
|
36-45 |
25.7 |
23.9 |
19.6 |
||
|
46-59 |
27.3 |
19.3 |
32.7 |
||
|
60 and older |
6.1 |
3.3 |
21.2 |
||
|
Education |
Null/primary |
29.2 |
16.5 |
34.3 |
<0.001 |
|
Secondary |
27.7 |
28.8 |
28.9 |
||
|
Higher |
39.4 |
46.1 |
32.4 |
||
|
Postgraduate |
3.7 |
8.6 |
4.5 |
||
|
Marital status |
Single |
37.4 |
50.2 |
43.0 |
<0.001 |
|
Married/with partner |
58.4 |
45.7 |
44.6 |
||
|
Divorced/widowed |
4.3 |
4.1 |
12.5 |
||
|
Occupation |
Sales/services |
28.4 |
24.7 |
22.1 |
<0.001 |
|
Unemployed |
2.2 |
2.9 |
17.3 |
||
|
Clerical and other |
11.0 |
12.4 |
7.4 |
||
|
Not specified |
21.0 |
16.1 |
5.5 |
||
|
Professional/ student |
25.5 |
35.4 |
21.2 |
||
|
Homemaker |
11.9 |
8.6 |
26.6 |
||
|
Anti-SARS-CoV-2 IgG |
Negative |
99.4 |
70.4 |
84.3 |
<0.001 |
|
Positive |
0.6 |
29.6 |
15.7 |
||
|
Total |
100.0 |
100.0 |
100.0 |
||
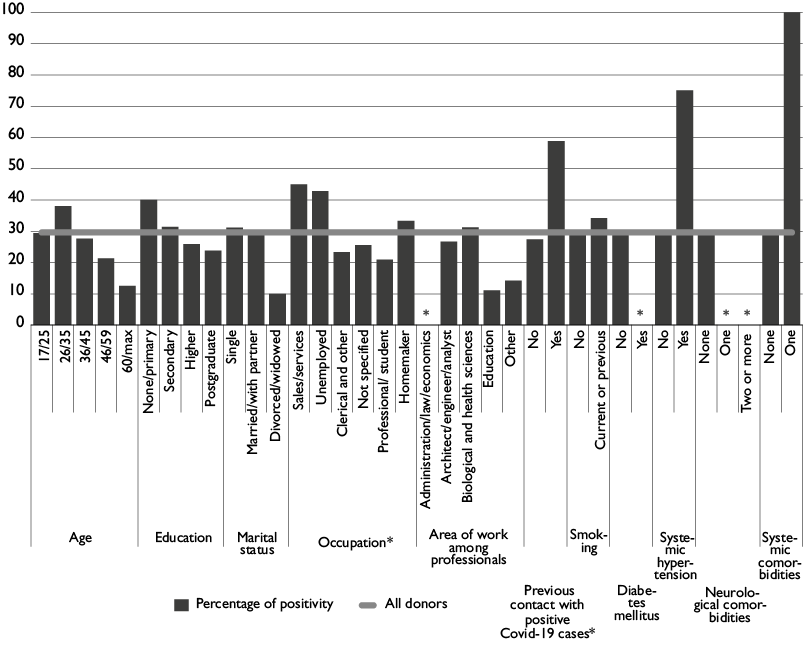
The characteristics significantly associated with a higher rate of positive anti-SARS-CoV-2 IgG antibodies in pandemic donors and neurological patients were also the occupation and previous contact with Covid-19 cases (table III and figure 1).
Table III Distribution of the positivity of anti-SARS-CoV-2 IgG antibodies according to demographic variables, contact with Covid-19, sample origin and comorbidities of the participants recruited during the pandemic. Mexico, January 2018 to December 2019
|
Donors n= 243 |
Patients n= 312 |
|||||||
|
Anti-SARS-CoV-2 IgG |
Negative |
Possitive |
p value* |
Negative |
Possitive |
p value* |
||
|
Demographic characteristics |
Age |
17-25 |
70.6 |
29.4 |
0.276 |
86.5 |
13.5 |
0.774 |
|
26-35 |
62.0 |
38.0 |
84.8 |
15.2 |
||||
|
36-45 |
72.4 |
27.6 |
85.3 |
14.8 |
||||
|
46-59 |
78.7 |
21.3 |
80.4 |
19.6 |
||||
|
60 and older |
87.5 |
12.5 |
87.9 |
12.1 |
||||
|
Education |
None/primary |
60.0 |
40.0 |
0.363 |
81.3 |
18.7 |
0.405 |
|
|
Secondary |
68.6 |
31.4 |
82.2 |
17.8 |
||||
|
Higher |
74.1 |
25.9 |
89.1 |
10.9 |
||||
|
Postgraduate |
76.2 |
23.8 |
85.7 |
14.3 |
||||
|
Marital status |
Single |
68.9 |
31.2 |
0.452 |
85.8 |
14.2 |
0.743 |
|
|
Married/with partner |
70.3 |
29.7 |
83.5 |
16.6 |
||||
|
Divorced/widowed |
90.0 |
10.0 |
82.1 |
18.0 |
||||
|
Occupation |
Sales/services |
55.0 |
45.0 |
0.040 |
79.7 |
20.3 |
0.033 |
|
|
Unemployed |
57.1 |
42.9 |
85.2 |
14.8 |
||||
|
Clerical and other |
76.7 |
23.3 |
100.0 |
0.0 |
||||
|
Not specified |
74.4 |
25.6 |
70.6 |
29.4 |
||||
|
Professional/student |
79.1 |
20.9 |
90.9 |
9.1 |
||||
|
Homemaker |
66.7 |
33.3 |
80.7 |
19.3 |
||||
|
Professionals’ work area |
Administration/law/economics |
100.0 |
0.0 |
0.428 |
100.0 |
0.0 |
0.691 |
|
|
Architect/engineer/analyst |
73.3 |
26.7 |
80.0 |
20.0 |
||||
|
Biological and health sciences |
68.8 |
31.3 |
86.7 |
13.3 |
||||
|
Education |
88.9 |
11.1 |
100.0 |
0.0 |
||||
|
Other |
85.7 |
14.3 |
88.9 |
11.1 |
||||
|
Clinical variables |
Covid-19 cases |
No contact |
72.6 |
27.4 |
0.011 |
86.3 |
13.7 |
0.035 |
|
Contact |
41.2 |
58.8 |
74.0 |
26.0 |
||||
|
Smoking |
No |
71.2 |
28.8 |
0.562 |
84.9 |
15.1 |
0.403 |
|
|
Current or previous |
65.8 |
34.2 |
77.8 |
22.2 |
||||
|
Diabetes mellitus |
No |
70.4 |
29.6 |
- |
86.2 |
13.8 |
0.041 |
|
|
Yes |
- |
- |
72.7 |
27.3 |
||||
|
Systemic hypertension |
No |
71.1 |
28.9 |
0.079 |
84.6 |
15.4 |
0.836 |
|
|
Yes |
25.0 |
75.0 |
83.0 |
17.0 |
||||
|
Neurological comorbidities |
None |
69.6 |
30.4 |
0.183 |
90.6 |
9.4 |
0.099 |
|
|
One |
100.0 |
0.0 |
81.6 |
18.4 |
||||
|
Two or more |
- |
- |
80.0 |
20.0 |
||||
|
Systemic comorbidities |
None |
70.7 |
29.3 |
0.296 |
84.1 |
15.9 |
1.000 |
|
|
One |
0.0 |
100.0 |
100.0 |
0.0 |
||||
|
Total |
70.4 |
29.6 |
84.3 |
15.7 |
||||
* Corresponding to Fisher’s exact test
*p< 0.05 corresponds to the Fisher exact test
Figure 1 Percentage of anti-SARS-CoV-2 IgG antibodies according to demographic variables, previous Covid-19 contact, sample origin and comorbidities. The antibody determinations were made in the Clinical Laboratory of National Institute of Neurology and Neurosurgery of Mexico from December 2020 to January 2021
The highest levels of anti-SARS-CoV-2 IgG antibodies were significantly associated with two conditions: being a woman and having had contact with positive cases of Covid-19 (table IV) (p= 0.009 and p= 0.005, respectively).
Table IV Distribution of the positivity of anti-SARS-CoV-2 IgG antibodies according to demographic variables, contact with Covid-19 and comorbidities of participants recruited during the pandemic. Mexico, January 2018 to December 2019
|
Anti-SARS-CoV-2 IgG |
p values |
|||||
|
Demographic characteristics |
1.1/2.1 |
2.2/4.5 |
4.6/6.9 |
≥7.0 |
||
|
Age group |
17-25 (n=20) |
30.0 |
35.0 |
30.0 |
5.0 |
0.725* 0.085‡ |
|
26-35 (n=38) |
18.4 |
39.5 |
23.7 |
18.4 |
||
|
36-45 (n=27) |
22.2 |
37.0 |
18.5 |
22.2 |
||
|
46-59 (n=30) |
16.7 |
30.0 |
30.0 |
23.3 |
||
|
60 and older (n=9) |
22.2 |
22.2 |
11.1 |
44.4 |
||
|
Sex |
Female (n=57) |
12.3 |
29.8 |
26.3 |
31.6 |
0.009* 0.001‡ |
|
Male (n=67) |
28.4 |
38.8 |
22.4 |
10.5 |
||
|
Education |
None/Primary (n=37) |
21.6 |
35.1 |
24.3 |
18.9 |
0.190* 0.716‡ |
|
Secondary (n=39) |
10.3 |
41.0 |
23.1 |
25.6 |
||
|
Higher (n=41) |
34.2 |
26.8 |
26.8 |
12.2 |
||
|
Postgraduate (n=7) |
0.0 |
42.9 |
14.3 |
42.9 |
||
|
Marital status |
Single (n=57) |
21.1 |
38.6 |
21.1 |
19.3 |
0.415* 0.962‡ |
|
Married/with partner (n = 59) |
18.6 |
28.8 |
30.5 |
22.0 |
||
|
Divorced/widowed (n = 8) |
37.5 |
50.0 |
0.0 |
12.5 |
||
|
Occupation |
Sales/services/unemployed (n=53) |
24.5 |
35.9 |
18.9 |
20.8 |
0.212* 0.294‡ |
|
Not specified (n=15) |
13.3 |
26.7 |
53.3 |
6.7 |
||
|
Professional, clerical other (n=32) |
25.0 |
37.5 |
21.9 |
15.6 |
||
|
Homemaker (n=24) |
12.5 |
33.3 |
20.8 |
33.3 |
||
|
Professionals’ work area |
Architect/engineer/analyst (n=5) |
0.0 |
60.0 |
40.0 |
0.0 |
0.256* 0.918‡ |
|
Biological and health sciences (n=7) |
0.0 |
42.9 |
14.3 |
42.9 |
||
|
Education (n=1) |
0.0 |
0.0 |
100.0 |
0.0 |
||
|
Other (n=3) |
33.3 |
33.3 |
33.3 |
0.0 |
||
|
Previous contact with positive Covid-19 cases |
No (n=98) |
22.5 |
39.8 |
21.4 |
16.3 |
0.005* 0.001‡ |
|
Yes (n=23) |
8.7 |
13.0 |
39.1 |
39.1 |
||
|
Sample origin |
Donor (n=72) |
20.8 |
40.3 |
23.6 |
15.3 |
0.234* 0.099‡ |
|
Patient (n=49) |
18.4 |
26.5 |
26.5 |
28.6 |
||
|
Smoking |
No (n=102) |
18.6 |
32.4 |
25.5 |
23.5 |
0.238* 0.062‡ |
|
Current/previous (n=19) |
26.3 |
47.4 |
21.1 |
5.3 |
||
|
Diabetes mellitus |
No (n=109) |
20.2 |
35.8 |
24.8 |
19.3 |
0.690* 0.322‡ |
|
Yes (n=12) |
16.7 |
25.0 |
25.0 |
33.3 |
||
|
Systemic hypertension |
No (n=109) |
19.3 |
35.8 |
25.7 |
19.3 |
0.587* 0.712‡ |
|
Yes (n=12) |
25.0 |
25.0 |
16.7 |
33.3 |
||
|
Neurological comorbidities |
None (n=81) |
18.5 |
38.3 |
23.5 |
19.8 |
0.790* 0.867‡ |
|
One (n=36) |
22.2 |
25.0 |
27.8 |
25.0 |
||
|
Two or more (n=4) |
25.0 |
50.0 |
25.0 |
0.0 |
||
|
Systemic comorbidities |
None (n=120) |
20.0 |
35.0 |
25.0 |
20.0 |
0.276* 0.156‡ |
|
One (n=1) |
0.0 |
0.0 |
0.0 |
100.0 |
||
|
Total (n=168) |
19.8 |
34.7 |
24.8 |
20.7 |
||
* Corresponding to Fisher’s exact test
‡Corresponding to the Jonckheere-Terpstra tendency test
Subjects recruited during the pandemic came from: Mexico City (292/555, 50%), the State of Mexico (168/555, 30%), and other states (95/555, 20%). The proportion of anti-SARS-CoV-2 positivity was higher in subjects from Veracruz (42%), Guerrero (36%), State of Mexico (26%), and Mexico City (20%). The highest proportion of subjects with IgG anti-SARS-CoV-2 was found in the State of Mexico municipalities of: Nezahualcóyotl (42%), Naucalpan (29%), and Ecatepec (23%), and the Mexico City counties of Miguel Hidalgo (36%), Álvaro Obregón (30%), and Iztapalapa (30%).
Discussion
The percentage of anti-SARS-CoV-2 antibodies in the sera of asymptomatic participants during the pandemic (21.8%) was higher than that reported in asymptomatic subjects from other countries (Italy, 4%; Germany, 2.3%; Iceland, 0.9%).26,27,28 The presence of anti-SARS-CoV-2 antibodies in three of the 538 asymptomatic donor sera obtained before the pandemic could be explained by the presence of antibodies generated against other coronaviruses (for example, those of the common cold), since it is known that the S1 protein (N-terminal subunit of the spike protein) shares homology with other beta- and alpha-coronaviruses,29,30 leading to pre-existing humoral immunity against SARS-CoV-2 in humans.9 Another explanation for having found anti-SARS-CoV-2 antibodies in the sample of November 2019 is that the virus was present in the community on a date prior to February 2020. However, this hypothesis does not seem to explain the presence of cases in November 2018 and September 2019.
The greater proportion of positive subjects found among male individuals aged 26 to 35 years old and working in the sales or service sectors could be related to the greater mobility and exposure of this population to infected subjects. The difference of anti-SARS-CoV-2 IgG percentage distribution in pandemic donors and neurological patients (29.6 and 15.7, respectively), may reflect that patients who are known to have a disease (neurological in this case) are taking greater preventive measures (greater distance, confinement, use of face mask, and others) than those who are known to be healthy.
Regarding the occupation, sales and service workers are more likely to acquire the infection because they are more exposed by coming into greater proximity to other people. The condition of having had contact with positive cases of Covid-19 indicated that asymptomatic subjects had acquired the infection, which shows the high infectivity of the virus and could also be related to receiving a higher viral inoculum through physical contact or constant closeness.
In the positive participants, the highest levels of anti-SARS-CoV-2 antibodies were observed in the presence of two conditions: being a woman and having had contact with positive cases of Covid-19. In regard to elevated antibody levels in women, these could be related to an increased antibody response by hormones and genes of the X chromosome in women,22,31 to an increased B lymphocyte activation,32 or to the fact that, from a social standpoint, women participate more in the care of the sick -conditions that may be causing them to develop high levels of antibodies. In regard to the elevated levels of antibodies in individuals with previous contact with positive Covid-19 cases, this finding reinforces what has already been reported by other studies.33,34,35
This study shows a high percentage of subclinical or asymptomatic positivity in the study sample and suggests, from an epidemiological point of view, that prevention measures should be continued to limit viral transmission, since the lack of knowledge of the infectious status among asymptomatic patients could be very high, and this could perpetuate transmission to subjects who continue to be exposed. However, this could also mean that, in specific populations, probably with high mobility, such as adults with primary or secondary education who work in sales or service, up to one-fifth could have anti-SARS-CoV-2 antibodies, which suggests some level of protection until mass vaccination of the population to contain Covid-19 is achieved. We consider it important to highlight that a treatment strategy for critically ill patients with Covid-19 is passive transfer of plasma with high antibody levels36,37 although trials are still being carried out to determine its effectiveness.38,39 In addition, it is critical to continue studying other aspects of humoral immunity, including assessing the current vaccination campaign and the durability of immune responses among the Mexican population.
The highest proportion of positive cases in the sample studied was found in the central states of Mexico (Metropolitan Area: Mexico City and the State of Mexico; Veracruz, and Guerrero), the municipalities and counties with the highest proportion of cases being Nezahualcóyotl, Naucalpan, Ecatepec, Miguel Hidalgo, Álvaro Obregón, and Iztapalapa, in which the seroprevalence must be monitored through subsequent trials and where specific preventive measures must be applied in order to limit the spread of infection.
Another aspect indicated by our results is the fact that there is a large number of individuals who do not develop symptoms, as reported in other studies.40 Therefore, it will be necessary to investigate the determining factors of protective immunity in order to establish health education policies to implement actions that will limit viral transmission. It will be important to carry out SARS-CoV-2 seroprevalence follow-up studies in the general population and donors.
Main limitations of the present study are that the subjects studied were asymptomatic healthy blood donors and neurological patients recruited from only one Mexican health institution; therefore, there is a selection bias, and the sample studied is not representative of the general population. Nevertheless, the presence of anti-SARS-CoV-2 that we report provides interesting data of epidemiological aspects, such as the association of these antibodies with occupation in sales or services and previous contact with positive Covid-19 cases. Another limitation is that although the test has a high sensitivity (94.4%) in patients with 10 days of infection or more, the evidence of the efficacy of the assays (in general) and particularly of antibodies is limited. Very few tests report sensitivity and specificity values considering the time of infection, the assays performed in asymptomatic or reinfected subjects are even fewer, and the duration of antibodies is unknown. This could lead to a certain underestimation of cases. However, we would expect that very few people have been accepted as donors if they had the “flu” within the previous ten days or were infected with SARS-CoV-2 infections more than a year ago.
SARS-CoV-2 seroprevalence follow-up studies must be favoured in the general population, being mandatory in donors.











 nueva página del texto (beta)
nueva página del texto (beta)


