Introduction
Worldwide, breast cancer (BC) is the most frequently diagnosed cancer among women.1 In Mexico, BC is the leading cause of cancer death among women.2 As in other Latin-American countries, the BC survival rates observed in Mexican females are lower than those of developed nations,3 partly due to delay in both the diagnosis and the start of the treatment.4 More than 45% of women are treated for advanced clinical stages of cancer in Mexico, compared to less than 15% in the United Kingdom.5
Considering that early access to chemo and radiotherapy determine, in part, the survival of BC patients, the Mexican Government included in 2007 this malignant tumor to the list of diseases funded by the Catastrophic Health Expenditures Fund (FPGC, Spanish acronym).6 Through the FPGC, accredited medical centers received funding for a limited set of procedures to diagnose and treat beneficiaries of the Seguro Popular with BC or other expensive diseases.7 However, even with appropriate treatment, women with advanced BC have a lower survival rate than women diagnosed at earlier clinical stages.8
Delays between the time when the first symptoms occur and the time when a woman seeks medical care, and between the time of the diagnosis and the time when the treatment is started, could account for the high proportion of women diagnosed and treated at advanced stages. Therefore, these indicators should be included in the evaluation of any program aimed at reducing BC-related mortality. The former indicator represents patient’s delay, and the latter, health system’s delay.9 Patient’s delay occurs due partly to the patient’s lack of financial resources, fear, and lack of information,10 among other reasons, while treatment delay is due to the characteristics of the health systems, including referral mechanisms, high volume of patients, longer distance to the clinic,10 and problems related to the untimely acquisition of cancer treatment drugs.11
Mexico is currently undergoing a major health system reform, with the replacement of the Seguro Popular with the National Institute of Health for Welfare (Insabi, Spanish acronym).12 Therefore, an analysis of the key determinants of survival becomes relevant to guide the decisions of policy makers. Under this scenario, we hypothesize that women attended after BC was included in the list of diseases of the FPGC had a lower delay in seeking health care or a lower delay in starting treatment than those who received care before the disease was included in the fund. Therefore, the aim of this study was to assess whether the FPGC reduced the time since the first perception of symptoms and seeking medical care, and from diagnosis to the start of treatment.
Materials and methods
Study design and setting
We conducted a before and after (2004 - 06 vs. 2007 - 09) cross-sectional study in four accredited hospitals for the care of BC patients through the FPGC. We selected one healthcare setting from each of the following regions in Mexico: Center (C), North (N), West (W) and Southeast (S).
Data sources and measurement
Data were obtained through direct interviews with BC patients or with key informants and from medical records. Key informants provided information when the participants had died or when their health status was a limitation for the interview. Responses were checked and verified. Collected data included age at diagnosis, educational level, healthcare setting, paid job, wealth index, affiliation to any medical insurance at the time of the diagnosis, and family history of breast cancer (mother, sister, daughter). For quality control, during the survey, a field supervisor verified that the interviews were carried out at the patients’ homes. The data were entered into an intelligent pdf format screen and the entering of data for each questionnaire was checked against the questionnaire. In addition, telephone calls were made to a sub-sample of participating women in order to corroborate the veracity of some responses. Clinical data (date of diagnosis, clinical stage, and date of the start of treatment) were drawn from the medical records.
Study population
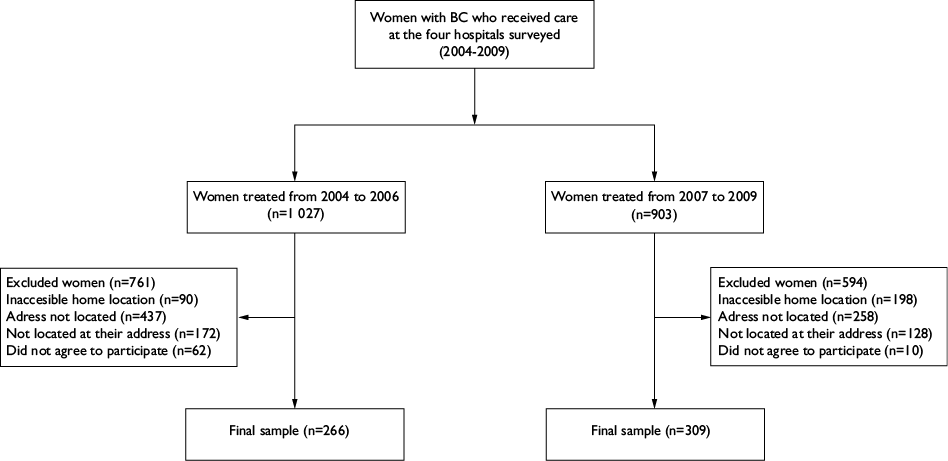
Eligible women were selected from a census of the total number of women treated for BC three years before (n= 1 027) and three years after (n= 903) the hospitals were accredited to receive the FPGC. Individuals residing further than 90 minutes away from the hospital, and those whom we were unable to locate at their addresses, or with incomplete provided data or incomplete medical records were excluded (figure 1). Regarding the years 2004 to 2006, we ended up with data from 266 treated women for analysis. Out of 1 027 homes, 761 addresses were excluded (inaccessible home location= 90; address not located= 437; women or proxy not located at their address= 172; and women who did not agree to participate= 62). As for the 2007-2009 period, we analyzed data from 309 treated women. Out of 903 homes, 594 were excluded (inaccessible home location= 198; address not located= 258; not located at their address= 128; did not agree to participate= 10) (figure 1).
Outcomes
There were two outcomes: a) delay in seeking medical attention (natural days elapsed from the date of onset of symptoms to the date of first contact with a physician, < 90 vs ≥ 90 days)13 and b) delay in the start of treatment (business days elapsed from the date of the diagnosis to the date of starting the treatment, ≤ 10 vs > 10 days). International standards established that no more than 10 business days should elapse between date of histopathologic diagnosis and date of start of the treatment, according to the European guidelines,14 and no more than 30 days, in accordance with the criteria of the Centers for Disease Control (CDC).13
Potential confounders
The following variables were considered as potential confounders: age at diagnosis (years), educational level (none/elementary and middle-school/high school or above), healthcare setting (Center, North West, and East), paid job (yes/no), wealth index (low, medium, and high), medical insurance at diagnosis (yes/no), family history of breast cancer (yes/no), and clinical stage at diagnosis (early: 0 to IIA vs late: IIB or above).
We used a principal component analysis to calculate the wealth index as a proxy of the socioeconomic status.15 The index was further categorized into low, middle, and high.
Statistical analysis
Summary statistics were computed, and stratified estimates were obtained before and after the hospitals were accredited to receive the FPGC. To assess whether FPGC was associated with the odds of delay in seeking medical attention and delay in starting treatment, multiple logistic regression models were used. In both cases, a dichotomous variable was constructed (1 = delay, 0 = no delay) where the cut-off points for the dependent variable were 90 natural days or more for the former,13 and 10 business days for the latter.14 First, we selected potential confounders (by their theoretical relevance) that reached a p value under 0.25 in the bivariate analysis. In order to obtain a parsimonious model, we used the backward regression technique, placing all the variables in the model and sequentially eliminating those that did not improve model performance.16 All statistical analyses were carried out with the Stata software, version 13.0.
Results
Data from 575 women were analyzed. Table I shows the characteristics of the study population by the selected variables. The proportion of women with medical insurance at the time of diagnosis decreased significantly from 23 to 14% (p<0.001), when we compared the women before and after the FPGC. BC cases were more likely to be diagnosed at an early stage (0 to IIA) after the FPGC than before it (34 vs. 23%, respectively p=0.026) (table I).
Table I Characteristics of the population for selected variables before and after the FPGC.* Mexico 2004-2009
|
Characteristics |
FPGC* |
p-value‡ |
|
|
Before |
After |
||
|
2004-2006 |
2007-2009 |
||
|
n= 266 (%) |
n= 309 |
||
|
Age at diagnosis (years)§ |
52 (13) |
52.3 (12) |
0.523 |
|
Education level# | |||
|
None |
80 (30) |
76 (25) |
0.105 |
|
Elementary |
78 (29) |
82 (27) |
|
|
Middle-school |
43 (16) |
73 (24) |
|
|
High-school or above |
65 (24) |
76 (25) |
|
|
Health-care setting |
|||
|
Center |
115 (43) |
108 (35) |
0.187 |
|
North |
86 (32) |
118 (38) |
|
|
West |
50 (19) |
68 (22) |
|
|
South East |
15 (6) |
15 (5) |
|
|
Paid job# |
|||
|
Yes |
107 (69) |
127 (41) |
0.766 |
|
Wealth index |
|||
|
Low |
88 (33) |
109 (35) |
0.173 |
|
Medium |
86 (32) |
115 (37) |
|
|
High |
92 (35) |
85 (28) |
|
|
Medical insurance at diagnosis of BC‡ | |||
|
Social security |
60 (23) |
42 (14) |
< 0.001& |
|
Other |
17 (6) |
2 (1) |
|
|
None |
179 (67) |
250 (81) |
|
|
Family history of breast cancer# | |||
|
Yes |
58 (23) |
65 (25) |
0.413 |
|
Clinical stage at diagnosis# | |||
|
Early (0 to IIA) |
62 (23) |
106 (34) |
0.026 |
|
Late (IIB or above) |
155 (58) |
172 (55) |
|
* FPGC: Catastrophic Health Expenditures Fund, from its acronym in Spanish. This fund was given since 2007 to accredited hospital to cover BC health expenditures
‡Chi-Square
§Standard deviation
#Percentages do not add 100% due to missing values
&Fisher exact test
BC: Breast Cancer
When we compared the time elapsed from the date of the onset of the symptoms to the date of first contact with a physician, we found no statistically significant differences between the two periods (table II). Only 58% of women before the FPGC and 60% of women after the FPGC sought medical care before 90 natural days since the appearance of symptoms (table II).
Table II Natural days elapsed from the date of starting symptoms to the date of first contact with a physician. Mexico 2004-2009
|
Healthcare setting |
Before the FPGC 2004-2006 |
After the FPGC 2007-2009 |
|||||
|
n |
Median (IQR) |
< 90 natural days* (%) |
n |
Median (IQR) |
< 90 natural days* (%) |
p-value‡ |
|
|
Center |
99 |
60 (8-180) |
54 |
96 |
60 (7-120) |
59 |
0.171 |
|
North |
74 |
15 (2-90) |
73 |
109 |
15 (3-90) |
69 |
0.545 |
|
West |
45 |
60 (3-180) |
53 |
63 |
60 (8-150) |
52 |
0.946 |
|
South East |
13 |
150 (30-365) |
31 |
12 |
210 (53-365) |
25 |
0.185 |
|
Total§ |
231 |
30 (3-180) |
58 |
280 |
45 (5-150) |
60 |
0.625 |
FPGC: Catastrophic Health Expenditures Fund,for its acronym in Spanish
IQR: Interquartile range
* European Breast Guidelines for breast cancer screening and diagnosis: acceptable
‡The p-value is derived from Mann-Whitney tests
§Missing data. 13% before and 9% after the FPGC
The median time from diagnosis to treatment was 30 business days and 29 business days before and after the FPGC, respectively. The interquartile range was 12 to 57 and 14 to 57 for the former and the latter periods, respectively (table III). No statistically significant differences regarding the proportion of women diagnosed within an optimal (< 10 days, European Breast Guidelines for breast cancer screening and diagnosis (EBG) or an acceptable period (< 15 days, EBG; < 30 days, CDCwere observed at any of analyzed hospitals. After the implementation of the FPGC, the Southeastern center reduced the median time for providing treatment from 66 days to 17 days. However, this trend was reversed at all the other centers that had higher median treatment delays after the FPGC.
Table III Median natural days elapsed from date of diagnosis to date of starting treatment according to medical center. Mexico 2004-2009
|
Healthcare setting |
n |
Median |
IQ range |
EBG (%) |
CDC (%) |
|
|
Optimal |
Acceptable |
Acceptable |
||||
|
Before the FPGC (2004-2006) | ||||||
|
Center |
102 |
45 |
(30-72) |
4 |
7 |
14 |
|
North |
68 |
16 |
(5-32) |
41 |
49 |
60 |
|
West |
42 |
12 |
(5-30) |
48 |
57 |
71 |
|
South East |
9 |
66 |
(28-122) |
11 |
22 |
22 |
|
Total |
221 |
30 |
(12-57) |
24 |
30 |
40 |
|
After the FPGC (2007-2008) | ||||||
|
Center |
100 |
51 |
(29-73) |
7 |
9 |
14 |
|
North |
99 |
19 |
(3-32) |
32 |
41 |
58 |
|
West |
57 |
24 |
(6-48) |
33 |
37 |
48 |
|
South East |
12 |
17 |
(12-38) |
25 |
42 |
58 |
|
Total |
268 |
29 |
(14-57) |
23 |
28 |
39 |
IQ range: Interquartile range; EBG: European Breast Guidelines for breast cancer screening and diagnosis (optimal, < 10 business days; acceptable, < 15 business days); CDC: Centers for Disease Control and Prevention (acceptable, < 30 business days); FPGC: Catastrophic Health Expenditures Fund, for its acronym in Spanish
There was no statistical association between either delay and the FPGC (table IV). Several factors were associated as statistically significant with the delay in seeking medical care. The odds of delay in seeking medical care were 0.55-times lower (95%CI: 0.32-0.96; p=0.035) among women with a family history of breast cancer, compared with women without a family history of breast cancer, adjusting for hospital, age, wealth index and medical insurance at diagnosis, education level and clinical stage. Moreover, women with a higher wealth index were associated with statistically significant lower odds of delay in seeking medical care (p-trend = 0.049). After controlling for confounding variables, women patients at the Northern clinic had 0.56-times the odds (95%CI: 0.34 -0.92; p=0.023) of treatment delay compared with the women receiving care at the Central clinic. Finally, women with medical insurance had 0.55 times the odds of diagnostic delay compared with women without medical insurance, after adjusting for potential confounders (95%CI: 0.32-0.97; p=0.039) (table IV).
Table IV Factors associated with seeking medical care and start of treatment delays.* Mexico 2004-2009
|
Variable |
Multiple analysis‡ |
p-value |
|
OR (95%CI) | ||
|
Model 1: Diagnostic delay§ | ||
|
FPGC |
||
|
Before (2004-2006) |
1.00 |
|
|
After (2007-2009) |
0.69 (0.44-1.08) |
0.105 |
|
Age at diagnosis, years |
1.02 (1.00-1.04) |
0.080 |
|
Family history of breast cancer | ||
|
No |
1.00 |
|
|
Yes |
0.55 (0.32-0.96) |
0.035 |
|
Wealth index |
||
|
Low |
1.00 |
0.045 |
|
Medium |
0.59 (0.35-0.99) |
0.110 |
|
High |
0.63 (0.35-1.11) |
0.049# |
|
Medical insurance at diagnosis | ||
|
No |
1.00 |
|
|
Yes |
0.55 (0.32-0.97) |
0.039 |
|
Health-care setting |
||
|
Center |
1 |
|
|
North |
0.56 (0.34-0.92) |
0.023 |
|
West |
1.43 (0.74-2.76) |
0.292 |
|
Southeast |
3.31 (0.96-11.45) |
0.059 |
|
Model 2: Treatment delay& | ||
|
FPGC |
||
|
Before (2004-2006) |
1.00 |
|
|
After (2007-2009) |
1.24 (0.68-2.27) |
0.490 |
|
Paid job |
||
|
No |
1.00 |
|
|
Yes |
0.55 (0.31-0.99) |
0.046 |
|
Clinical stage at diagnosis | ||
|
Early (0 to IIA) |
1.00 |
|
|
Late (IIB or above) |
2.23 (1.23-4.04) |
0.009 |
|
Family history of breast cancer |
1.00 |
|
|
No |
||
|
Yes |
0.61 (0.31-1.19) |
0.149 |
|
Education level |
||
|
None |
1.00 |
|
|
Elementary - middle school |
1.04 (0.49-2.22) |
0.910 |
|
High-school or above |
0.37 (0.15-0.89) |
0.027 |
|
Health-care setting |
||
|
Center |
1.00 |
|
|
North |
0.04 (0.01-0.11) |
< 0.001 |
|
West |
0.05 (0.01-0.15) |
< 0.001 |
|
Southeast |
0.09 (0.02-0.47) |
0.005 |
FPGC: Catastrophic Health Expenditures Fund, for its acronym in Spanish
* Seeking medical attention delay (natural days elapsed from date of start of symptoms to the date of first contact with a physician, < 90 vs ≥ 90 natural days) and b) start of treatment delay (natural days elapsed from date of diagnosis to date of starting treatment, ≤ 10 vs > 10 business days)
‡The odds ratios (OR) and 95% confidence intervals (CI) were computed through logistic regression models
§In model one, the odds ratios were adjusted for education level, clinica stage and for the variables in the table
#P for linear trend
&In model 2, the odds ratios were adjusted for age at time of diagnosis, medical insurance at diagnosis and for the variables in the table
The multiple logistic regression model demonstrated that the introduction of the FPGC was not associated with the delay in starting the treatment (OR=1.24; 95%CI: 0.68-2.27). Compared to women at early stages of the disease, those with advanced clinical stages had 2.2 times the odds of treatment delay (95%CI: 1.23-4.04). Women with paid job had 0.55 times the odds of starting treatment delay compared with women who were not economically active (95%CI: 0.31-0.99). The odds of treatment delay among women with high-school or higher education were 0.37 times the odds among women with no education (95%CI: 0.15-0.89) (table IV).
Discussion
We conducted a before and after cross-sectional study to assess if women treated after the FPGC had lower delays in seeking medical care and in starting treatment, compared to those who received care before the fund was implemented.
After adjusting for potential confounders, we found no association between the FPGC and delay in seeking medical care. We expected a decrease in this delay because, once the fund was implemented, women could consider seeking free medical care. However, the main reasons women gave for not seeking treatment on time were not having money or time, as well as fear. This is consistent with an ethnographic study in Mexico that showed that delay in seeking medical care was associated with fear and lack of information.10 It is very likely that the women in our study did not seek treatment on time because they were not informed about the FPGC benefits.
We did not observe an association between the FPGC and the delay in starting treatment. Although our data do not support the hypothesis that higher coverage for the uninsured increases patient delay in a middle-income country due to the lack of proper infrastructure and human resources, this may partially explain our findings.17 The effect of increased coverage for the uninsured is different in more developed countries, like the United States of America (USA). The implementation of the Affordable Care Act (ACA) in 2010 was not associated with treatment delay for breast cancer.18 The ACA is a financing mechanism that shares some characteristics with the Seguro Popular. Not all the states in the USA have fully implemented the ACA, and some have even promoted disenrollment of patients from Medicaid, providing the conditions to conduct quasi-experimental studies. For instance, Tennessee did not experience a decrease in treatment delay although it stopped covering 4% of its non-elderly beneficiaries.19 In contrast, at the national level, women with higher levels of Medicaid coverage had shorter delays for breast cancer surgery.20 These results are relevant, given the recent debates regarding the expansion of health coverage in Mexico and in the USA.
In our study, the odds of seeking medical care delay were lower in women with a family history of breast cancer, with a medium or high socioeconomic status, having medical insurance, and resorting to the Northern healthcare setting. Socioeconomic status and medical insurance have also been associated with delay in seeking medical care in Colombia.21 Although clinical stage was not associated to seeking medical care, other studies have found that higher clinical stages are associated to longer delays.21 Clinical breast examination has been associated with reduced delay and diagnosis of the disease at an earlier clinical stage;22 however, we did not assess this characteristic.
In this study, the odds of starting treatment delay were lower in women with a paid job, a family history of breast cancer, high-school education or above, and treated in the North, West, and Southeast healthcare settings, while the odds were higher in those diagnosed at a late clinical stage. In accordance with our findings, Mexican women with stage I breast cancer received treatment 26 days after their diagnosis, whereas patients at stage IV were treated 49 days after their biopsy.4 Similarly, health system’s delay increased the probability of being diagnosed with breast cancer at clinical stages III and IV.23 Other factors associated with a higher likelihood of treatment delay were lack of high school education and lack of a paid job. Delaying the start of BC treatment after experiencing symptoms has a negative impact on cancer survival. For instance, patients with total delays of more than three months had 12% less survival compared with those with less delay.24 In Mexico, having longer waiting times between the biopsy and the start of treatment lowers the survival rate of women with breast cancer.4 Therefore, reducing diagnosis and treatment delays should be a priority for breast cancer health policy makers.25 Delays in seeking medical care and starting treatment may explain why certain institutions or states perform better in terms of breast cancer survival. Therefore, they could be used as key performance indicators at the National Institute of Health for Welfare (Instituto de Salud para el Bienestar, Insabi)12 that will start to operate in Mexico in January 2021 after the disappearance of the Seguro Popular, which has already taken place. Insabi replaces Seguro Popular, and its objective is to ensure the provision of free high-quality health services, medicines, and supplies to all those people who lack social security.12
Financing mechanisms such as the FPGC focused on preventing catastrophic out-of-pocket spending by increasing access to expensive therapies. However, this Fund failed to remove other barriers like the lack of infrastructure, trained professionals, and equipment maintenance.26 Recognizing that these efforts may not suffice to improve the survival of patients with breast cancer, some Mexican states have already acted towards reducing treatment delay. Such is the case of Alerta Rosa, a program in Nuevo León27 that has focused on helping patients with symptoms of breast cancer or abnormal imaging to navigate the healthcare system. Alerta Rosa also represents an example of how programs can be tailored to the local needs of every population. Nevertheless, in order to become aware of these needs, policymakers must identify the barriers for timely care at every stage of the natural history of breast cancer, both at the patient and the health system levels.9 Therefore, the Insabi should analyze diagnostic and treatment delays, providing real-time feedback to the learning health system.
The median patient delay was 30 days before the beginning of the FPGC and 45 days afterwards. Only 24% of the patients with breast cancer sought medical care in a timely fashion. In terms of patient delay, our results are comparable to those of other studies performed in Mexico.4,14 However, other countries in Latin America report lower proportions of patient delay. For instance, 34% of patients in Colombia exhibit delays of over 30 days.21 In contrast, low-income countries like Uganda report median patient delays of up to 13 months.28
The median treatment delay was 30 days before and 29 days after the FPGC was implemented. Only 23% of the patients with breast cancer received optimal timely treatment in our population. In terms of the treatment interval, our results are consistent with those of similar studies performed in diverse settings in Mexico.4,14,18 However, small studies performed at specialized clinics report shorter patient delays.29 In contrast, other reports in the Latin American region have found waiting times of 69 days for starting treatment.30
When we compared the stages at which women were diagnosed before and after the FPGC, we observed a 23% decrease in the proportion of women diagnosed with advanced breast cancer. It is worth considering that, besides the FPGC, the Seguro Popular also included preventive care in the form of early cancer detection. Likewise, the Preventive services provision of the ACA in the USA shifted the diagnosis of breast cancer to lower stages.31 Furthermore, the expanded medical coverage provided by the ACA reduced the likelihood of metastatic cancer disease.32 Because survival for patients at more advanced stages of breast cancer is less than five years,33 increasing the proportion of women diagnosed at early stages should be a priority for any breast cancer program.
Our study has several strengths. For instance, the outcome was measured using data from the medical records, preventing the memory bias of survey designs. Moreover, our methodology included a protocol for data quality assurance. Finally, the states where the participating hospitals were located represent 40% of the incident cases of BC in Mexico. Despite these strengths, our study faces some limitations. Given its cross-sectional design, we need to consider our results cautiously. Although policy interventions offer natural experiments that can be evaluated, our design has the risk of unmeasured confounding. Moreover, for feasibility reasons, we were not able to assess individuals who lived further away than 90 minutes from the clinics. Therefore, future studies using administrative databases should focus on this population to confirm our results. We only evaluated delay in seeking medical care and in starting treatment, leaving aside other components of delay from the health system’s perspective. Researchers have validated surveys to specifically assess each component of patient’s and health system’s delays.34 Future studies measuring the impact of health policy for breast cancer should also consider performance indicators to evaluate the level of maturity of the quality improvement at the different levels of management.35,36
In order to ensure effectivity, efficiency, efficacy and equity, Insabi and other institutions could consider other key performance indicators (KPI) in accordance with the Methodology for Productive Management of Health Systems.35 Besides patient and treatment delays, the Methodological Manual Towards Excellence recommends measuring coverage (mammography, clinical evaluation, diagnostic evaluation, and treatment), treatment opportunity, the proportion of breast cancer detected with screening, and the proportion of women diagnosed at early stages.36
The Seguro Popular addressed some of the barriers to access to expensive medical treatment for breast cancer through the FPGC. In doing so, it accomplished financial protection and increased coverage. Nevertheless, lengthy delays in treatment precluded the Seguro Popular from achieving the goal of providing quality care. Future reforms aiming at universal healthcare (such as Insabi) in Mexico and elsewhere must consider metrics like patient and treatment delay in order to measure the quality of care and provide timely and actionable feedback.











 nueva página del texto (beta)
nueva página del texto (beta)