Introduction
The Covid-19 pandemic has strained health systems worldwide with a burden of mild and severe cases of illness and deaths.1 The responses have relied on the health systems’ capacity, ability, and resources, and they have varied according to the structure of social security in each country. For example, in Japan, the public sector covered diagnosis and treatment of Covid-19 through their national health insurance system at the state level.2 In the United States, the Center for Disease Control and Prevention has covered some of the Covid-related costs. States such as New York and Washington have ordered insurance companies to give up copays and deductibles for testing.3 In Benin, the government is responsible for the isolation, care, and treatment of suspected and confirmed cases of Covid-19.4 Invariably, the government’s role and the public health response have been crucial to containing the spread of the epidemic and its consequences on people’s health and lives.
By March 2021, Mexico accumulated more than 2.2 million cases of Covid-19 and over 200 000 deaths.5 Early in 2020, the government adapted hospitals to provide care for Covid-19 patients.6 With a fragmented structure designed to serve populations based on their employment status,7 the Mexican health system was ill-prepared to confront the epidemic in 2020. While half of the population had access to social security and accessible and quality health care, the other half -those unemployed or working in the informal sector of the economy- had access to precarious services offered by the Ministry of Health and no social security coverage. Furthermore, over the past decade, an increasing share of the population has sought health care in the private sector; by 2018, only 41% of those with a health problem at the national level received care in the public sector.8
This study describes the Mexican health system’s response to the Covid-19 pandemic from the households’ perspective. We adapted the health care continuum framework previously described as the “cascade of care”.9 Specifically, this paper describes three versions of the Covid-19 cascade of care following the population with symptoms compatible with Covid-19, overall and by tertile of municipalities’ contribution to total Covid-19 deaths and the population positive to SARS-CoV-2 antibodies test. As such, the cascade starts identifying the population that reported symptoms compatible with Covid-19 or positive to antibodies. Then, we measured the proportion who sought care, received care, were tested, were diagnosed positive, and survived. Along each step, their own choices or the health system’s barriers exclude people from the continuum. We investigate whether, in the end, public or private services resolved their needs related to Covid-19. We also estimated factors associated with the probability of receiving care in public or private services.
Materials and methods
We used data from the National Health and Nutrition Survey Covid-19 (Ensanut Covid 2020), collected in a sample of 10 216 households between august 18 and November 13, 2020.10 The Ensanut Covid 2020 is representative at the national, regional (nine regions), and urban and rural levels. The survey’s objective was to estimate the prevalence of SARS-CoV-2 and relevant comorbidities (diabetes, hypertension, and obesity) and document health services’ utilization.
Thus, we aim to report health care services utilization contextualized by the health needs of the Mexican population amid the Covid-19 pandemic. A relevant consideration to this end is that health services’ utilization results from the interaction between the public and their needs and decisions on one side (the demand side), and the health system’s accessibility and availability, and health providers’ responsiveness, on the other (the supply side). The frame we used to describe this interaction is the cascade of care.9 We describe the cascade for three subpopulations; for the population with symptoms compatible with Covid-19 -overall and by tertiles of mortality; and for those who tested positive to SARS-CoV-2 antibodies. We present the former nationally and by Covid-19 mortality at the municipality level.
The analytical sample varies by analysis. From the 10 216 households, 36 103 members responded the questionnaire. The cascades of care include the population of all ages and the regression models applied only to adults.
The first Covid-19 cascade starts with the population reporting symptoms consistent with Covid-19 (n=2 511). Sequentially, we then followed the share of them who sought care, received care, were tested, diagnosed, and survived. The household member selected as the key informant for the survey reported for all members of the household any symptoms or signs related to Covid-19 between March and the survey´s date. The informant selected symptoms experienced by each member of the household from a list all potential Covid-19 symptoms. We identified respondents with a combination of symptoms consistent with the Ministry of Health’s “operational definition” of suspect cases, i.e., having at least one of the main four symptoms and one or more minor symptoms.11 The former included cough, fever, headache, and shortness of breath, and the latter difficulty breathing, body aches, sore throat, runny nose, chills, rapid respiration, loss of smell or taste, red eyes; and chest pain. We also investigated reasons for not seeking and not receiving care, as reported by the respondents. Finally, we documented the status at the moment of the survey of all individuals who experienced Covid-19 symptoms, either fully recovered, still recovering, recovering with sequels, or deceased. Along the cascade, we distinguished the proportion of people who sought and received care from public institutions or private providers.
The second cascade of care starts with the population who tested positive to a SARS-CoV-2 antibodies test from a randomly selected subsample of respondents (n=2 152).10 The sampling strategy of respondents who provided blood samples for the estimation of SARS-COV-2 antibodies was based on the Covid-19 seroprevalence rate and the response rate reported in the literature from other countries. A stratified sampling design at the household and individual level was used to collect 9 464 blood samples from men and women from all ages, representative at the national, region and urban/rural levels.10 The cascade of care includes all individuals who tested positive for SARS-CoV-2 antibodies, regardless of symptoms. We then show the proportion who experience symptoms and the percentage who sought care, received care, were tested, diagnosed, and survived. In this case, we also report reasons for not seeking care and status. The cascade documents the experience and decisions of the population who tested positive for SARS-CoV-2 antibodies; whether they had symptoms, sought and received care, and place where they received it.
Thirdly, we present the cascade for the 2 511 individuals with symptoms compatible with Covid-19 divided into tertiles of Covid-19 mortality rates at the municipality level (n=937 for the highest mortality rate, n=826 for the medium tertile and n=748 for the lowest mortality rate tertile). Mortality burden at the municipality level was estimated using data from January to December 2020 from confirmed Covid-19 reported at the epidemiological national surveillance system for Covid-19.5 We estimated the contribution of deaths in each municipality over total national Covid-19 deaths. We then created tertiles by dividing municipalities in three groups, ranked by mortality burden and each group containing one third of the total Mexican population.
To further investigate the health system’s response, we described the relationship between affiliation to social security and the institution that provided care for the population with Covid-19 symptoms who received care (n=1 617). In the public sector, affiliations include Instituto Mexicano del Seguro Social (IMSS), the social security system for those employed in the private sector; Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado (ISSSTE) for government employees; and other public health insurance systems such as army, navy, or oil for government employees in those sectors. The population employed in the informal sector of the economy (roughly half of the working population) has no health insurance affiliation. Concerning health care provision, all the social security systems (IMSS, ISSSTE, army, navy, and oil) are also health care providers in facilities of their own. People without social security are entitled to receive care in health facilities governed by the Ministry of Health (SS). A small private health insurance market targets mostly high-income households who receive care in private clinics and hospitals. Finally, a vast and increasing market of private medical offices in pharmacies (MOP) supplies primary care to people from all affiliations. In our analysis, we distinguished MOP and other private providers.
To understand the choices of health care providers among adults with Covid-19 symptoms, we used three multivariate probit regression models to identify sociodemographic factors associated with the probability of: 1) seeking care versus not seeking care; 2) receiving care in public facilities versus not receiving care; 3) received care in private facilities versus not receiving care. The first model includes the 2 007 adults with symptoms, the second model applies to 992 adults who sought care and either received or not care; and the last model includes 1 611 adults who received care in private facilities and those who did not receive care; all excluding missing values.
The analyses included the following sociodemographic independent variables: age (20-39, 40 to 59, or more than 60), sex, education (no education, primary, secondary, high school, college, or more), and socioeconomic status (SES) (low, middle, high). We estimated the SES categories based on a wealth index of household durables (such as TV, fridge, wash machine, computer), housing characteristics (floor, wall, ceiling, and roof materials), and services (electricity, running water, home fuel, sewer system, toilet). We used principal component analysis to estimate an index, divided into tertiles. In the regressions, we also included variables measuring labor status, specifically whether people were employed at the time of the survey (at least one hour the previous week), and a binary variable to measure whether respondents were affiliated to any social security system. We also measured the presence of at least one comorbidity diagnosed by a medical doctor -diabetes, obesity, hypertension, cardiovascular disease, chronic lung disease, cancer, or HIV/AIDS. Finally, we measured whether participants reported contact with a suspected or confirmed case of Covid-19 between March and the date of the survey. We looked at the correlation between independent variables and all of them had very low correlations.
For all analyses, descriptive and regression models, the complex design of the survey was applied.
The Research Ethics Committee of the National Institute of Public Health approved this study.
Results
Seven percent of the total population reported Covid-19 related symptoms between March and November 2020 (figure 1). Two-thirds of them sought health care (66.7%), and mostly received it (64.4%), mainly in the private sector -three quarters of them. Only 15.4% of the people with symptoms were tested for SARS-CoV-2, and 21.2% were positive, confirmed either by tests or symptomatically. Most (21.1%) of the population with Covid-19 like symptoms who were diagnosed as positive (21.2%) survived. Although fewer people received care in public facilities (24.7%) than in private offices, proportionally more were tested (38.3%) and diagnosed (28.4%) in the public sector.
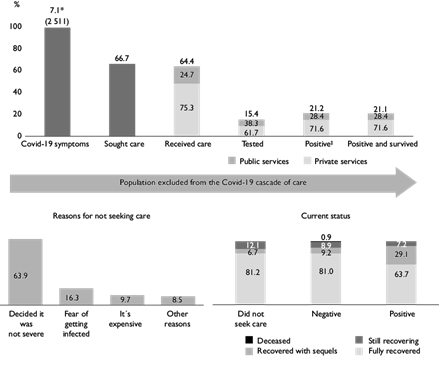
Authors’ estimations using data from the 2020 Covid-19 National Health and Nutrition Survey (Encuesta Nacional de Salud y Nutrición, Covid-19, 2020) on July 2021.
Top panel: the Covid-19 cascade of care shows the percentage of the population with Covid-19-like-symptoms, the proportion who sought care, received care, were tested, were diagnosed, and survived. Bottom left: reasons for not seeking care for those excluded from the cascade after the second column. Bottom right: current status of individuals with Covid-19 symptoms who did not seek care, those with a negative test and Covid-19 survivors. * Proportion of the population who reported having Covid-19 like-symptoms. ‡ The “positive” column is smaller than the “tested” column because there are people who report having been diagnosed only by their symptoms, without a test.
Figure 1 The Covid-19 cascade of care for people with symptoms compatible with Covid-19, reasons for not seeking care and current status. México 2021
Approximately one-third of the population with any symptom did not seek care. The main reasons were: they decided that their symptoms were not severe (63.9%), they were fearful of getting infected (16%), or they thought it would be expensive or had no money (9.7%).
By the time of the survey, most people who did not seek health care had fully recovered (81.2%), 12.1% were still recovering, and 6.7% had sequels. Among the confirmed cases that survived, 63.7% fully recovered by the date of the survey, 29.1% had sequels, and 7.2% were still recovering.
From those who received care at public health facilities, 84.3% received outpatient care, 10.9% were seen at an emergency room, 8.3% were hospitalized, and 2.5% were treated at an intensive care unit. As for those who received care at private health facilities, the majority were seen in outpatient visits (96.4%), and only 3%, at an emergency room (results not shown).
Figure 2 shows the cascade of care for those who tested positive for SARS-CoV-2 antibodies. Twenty-three percent of the population tested positive. Of these, 23.2% reported symptoms compatible with Covid-19. Approximately one-fourth of the positives sought care; 22.5% received care (25.9% in public services and 74.1% in private providers).
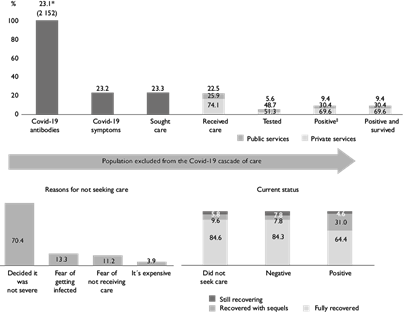
Authors’ estimations using data from the “Encuesta Nacional de Salud y Nutrición, Covid-19, 2020” on July 2021.
Top panel: the cascade of care shows the percentage of the population who tested positive to a SARS-CoV-2 antibodies test, the proportion of those with Covid-19 like-symptoms, who sought care, received care, were tested, were diagnosed, and survived after diagnosis. Bottom left: reasons for not seeking care for those excluded from the cascade after the second column. Bottom right: current status of individuals with Covid-19 symptoms who did not seek care, those with a negative test, and Covid-19 survivors. * Percentage of people from the population who had Covid-19 antibodies. ‡ The “positive” column is smaller than “tested” because there are people who report having been diagnosed without test, only by their symptoms.
Figure 2 The Covid-19 cascade of care for people who were positive to SARS-CoV-2 antibodies, reasons for not seeking care and current status. México 2021
Among the population with a positive SARS-Cov-2 antibodies test, only 5.6% were tested for and 9.4% were diagnosed with Covid-19, confirmed either by a test or symptomatically. Most of the diagnosed people survived. Among those who did not seek care, 70.4% reported that their problem was not severe, 13.3% were fearful of getting infected, and 11.2%, of not receiving care. The distribution of the “current status” is similar to that of the previous cascade.
The mortality burden seems to have influenced the decisions of the population and of the providers. Figure 3 shows the cascade of care by tertiles of mortality at the municipality level for the population with Covid-19 symptoms. We found relatively small differences in the proportion of the population with Covid-19 symptoms among the three groups of municipalities -between 6.2 and 7.8% of the total. However, the share of those who sought and received health care was different, with a significantly higher proportion seeking (and receiving) care in the high mortality areas (73.6%) than in the medium and low mortality regions of the country (68.1 and 57.1%, respectively.) The mortality burden also influenced the providers’ decisions to test people, with 19.5, 15.5, and 10.4% of people tested in the high, medium, and low mortality areas. Positivity rates were also consistent with mortality levels, being significantly higher in high and medium than in low mortality municipalities.
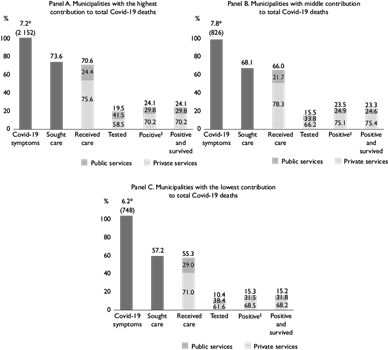
Authors’ estimations using data from the “Encuesta Nacional de Salud y Nutrición, Covid-19, 2020” on July 2021.
* Percentage of people from the population who had Covid-19 symptoms
‡ The “positive” column is smaller than the “tested” column because there are people who report having been diagnosed without test, only by their symptoms. Each tertile comprises one third of the total Mexican population.
Figure 3 The Covid-19 cascade of care by Covid-19 mortality rates at the municipality level. México 2021
In figure 4, we analyze the population’s choices regarding health providers versus their health insurance affiliation. Each column groups the people by their primary affiliation, and on the top, we display the share of the total population that accounted for each group. The sections within each column represent the proportion that chose different health providers.
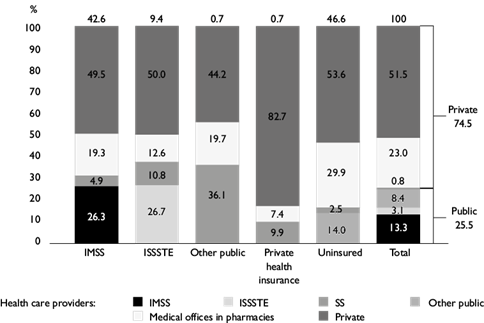
Authors’ estimations using data from the “Encuesta Nacional de Salud y Nutrición, Covid-19, 2020” on July 2021.
Each column groups the population by their primary health insurance affiliation. The distribution of health care providers used for Covid-19 care is displayed within each column. The top of each column shows the proportion affiliated to the primary health insurance institution.
IMSS: Instituto Mexicano del Seguro Social, ISSSTE: Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado, SS: Secretaría de Salud.
Figure 4 Distribution of health care providers by affiliation for the population with Covid-19 symptoms who received care. México 2021
The column on the right depicts the distribution of the whole population. Overall, only 25.5% of all the people who had Covid-19 symptoms and received care did so in public health facilities (13.3% in IMSS, 8.4% in SS, 3.1% in ISSSTE, and 0.8% in other), while 74.5% did so from private providers (23% in MOP, and 51.5% in other).
Among IMSS affiliates -- 46.2% of the total population -- only 26.3% received care from IMSS facilities, and 68.8% from private providers, including 19.3% from MOP. Regarding ISSSTE affiliates (10.2% of the total), 26.7% received care from ISSSTE facilities and 62.5% from the private sector (12.6% MOP). Only 14% of the uninsured population -- 42.1% of the total -- received care at the Ministry of Health facilities (SS), and 83.5%, at private facilities (29.9% MOP).
Table I shows factors associated with the likelihood of seeking care or receiving care at public or private facilities. Model 1 estimates the probability of seeking care versus not seeking care among individuals with Covid-19 symptoms. The population with comorbidities and contact with suspected or confirmed cases (compared to no contact) were more likely to seek care. However, social security and higher socioeconomic status (versus low) also increased the probability of seeking care. The results were similar in regard to the probability of seeking care in public facilities versus not seeking care, except that socioeconomic status did not increase the latter. Social security affiliation increased significantly more the likelihood of attending a public site than not attending any site. In contrast, higher socioeconomic status, and urbanicity significantly increased the probability of seeking care in the private sector versus none.
Table I Factors associated with the probability of seeking and receiving care in public or private health facilities among adults with symptoms compatible with Covid-19. Mexico 2021
|
Model 1. Sought care versus did not seek care |
Model 2. Received care in public facilities versus not receiving care |
Model 3. Received care in private facilities versus not receiving care |
|
|
n = 2 007 |
n = 992 |
n = 1 611 |
|
|
Age (ref: 20-39 years) |
|||
|
40-59 |
0.020 |
0.026 |
0.022 |
|
≥60 |
0.018 |
-0.043 |
0.048 |
|
Men (ref: women) |
-0.022 |
0.015 |
-0.040 |
|
Comorbidity (at least one) |
0.073* |
0.073‡ |
0.086* |
|
Covid contacts (ref: no contacts) | |||
|
Suspected case |
0.096* |
0.164* |
0.074‡ |
|
Confirmed case |
0.170* |
0.214* |
0.167* |
|
Social security (ref: uninsured) |
0.105* |
0.279* |
0.046§ |
|
Currently working |
-0.0003 |
0.014 |
-0.001 |
|
Education (ref: no education-preschool) | |||
|
Primary school |
-0.043 |
0.042 |
-0.061 |
|
Secondary school |
-0.010 |
0.062 |
-0.027 |
|
High school |
-0.012 |
0.070 |
-0.029 |
|
College or more |
-0.075 |
-0.024 |
-0.091 |
|
Socioeconomic level (ref: low) |
|||
|
Middle |
0.058‡ |
-0.040 |
0.097* |
|
High |
0.123* |
-0.016 |
0.183* |
|
Urban (ref: rural) |
0.040 |
-0.005 |
0.067‡ |
Own estimations using data from the “Encuesta Nacional de Salud y Nutrición, Covid-19, 2020” on July 2021. Marginal effects of probit models. * significant at 1%, ‡ significant at 5%, § significant at 10%. For model 1, the analytical sample are 2 007 adults with Covid-19 symptoms. For model 2, the sample is 992 adults with Covid-19 symptoms (642 that did not receive care and 350 who received care in the public sector). For model 3, the sample is 1 611 (969 who received care at a private health facility and 642 did not receive care).
Discussion
This paper reports that 7.1% of the population had symptoms compatible with Covid-19. Of them, 64.4% received health care, and 15.4% tested positive for SARS-CoV-2. We also found that among the population living in municipalities with the highest Covid-19 mortality rates, a higher percentage sought and received care than in medium and low mortality areas.
Our paper also shows that, of the 23.1% of the population who tested positive for SARS-CoV-2 antibodies -- regardless of whether or not they had symptoms--, only 22.5% sought and received care. Approximately two-thirds of the positives were asymptomatic; 23.2% reported symptoms consistent with the “operational definition” of Covid-19.
A noteworthy finding of our study is that three out of every four people with Covid-19 symptoms that received care relied on the private sector (74.5%). The use of private health services was extensive even among the population with social security. This result reflects a previously documented critical challenge of the Mexican health system, namely, the growing dependence of Mexicans on private health services, prominently on MOP.8
In 2018, 41% of the population reporting a health problem received care in public health facilities, and even the population with social security used private services.8 Although affiliation to Seguro Popular (the public health insurance for the unemployed and the informal workers) increased rapidly between 2003 and 2010, providing coverage for the uninsured, the enrollment rate was not matched by the availability of public health facilities.8 Furthermore, between 2010 and 2018, MOP grew considerably while the amount of primary public health facilities from SS remained unchanged.8
The fact that so many people received care from private providers is not reassuring. MOP supplied 34% of the total private-sector care. Since MOP are unregulated and potentially vulnerable to significant conflicts of interest, they may fail to follow treatment guidelines and have incentives to overprescribe medications. Indeed, studies have shown that doctors in MOP have less experience and earn less than public practitioners, and patients pay more in those facilities.12,13
One-third of the population with Covid-19 symptoms did not seek health care. The reported reasons are varied, and some of them are expected, such as “considering that the problem was not severe” (63.9%). However, other reasons were linked to the pandemic, particularly “fear of getting infected with SARS-CoV-2” (16.3%). Fortunately, 93% of all the people with symptoms who did not seek care were either fully recovered or recovering by the time of the survey.
We found that the population with at least one comorbidity, those in contact with a suspected Covid-19 case, and those in contact with a confirmed Covid-19 case had a higher probability of seeking versus not seeking care (model 1), of receiving care in public health facilities versus not receiving care (model 2) and of receiving care in private facilities versus not receiving care (model 3). Social security increased the likelihood of receiving care in public and private facilities, albeit more so in the former. Higher socioeconomic status, higher education, and urbanicity increased the probability of seeking care and of doing so in the private sector. Unfortunately, these findings are consistent with a recent study that documented the increasing preference for private providers in Mexico.7
An important limitation of the study is that self-reporting of Covid-19 symptoms may be biased. Firstly, recall bias is a possibility, since the respondents had to report the presence of symptoms within a relatively long period -between March and the interview date, which could have been in November. Additionally, some of the relevant symptoms are not Covid-19-specific and may be related to other conditions. Another limitation is that the only private provider we can identify is medical offices in pharmacies. Apart from MOP, there is a vast landscape of private providers in Mexico, heterogeneous in quality and prices. However, it is essential to identify MOP, given their relative importance and potential drawbacks.
The models for the probability of receiving care are conditional on seeking care. We acknowledge that seeking care is potentially endogenous, and our models do not account for this potential source of bias in some of the parameters.
Our study has the strength that for the first time, the Ensanut Covid-19 opened questions to people who died (responded by proxy, usually by the head of household or the main respondent); therefore, we believe that there is no selection bias, or that it is negligible. With this information, we were able to add in the last column of the cascade those who survived.
Despite these limitations, our study documents vital aspects of the response to the Covid-19 pandemic in Mexico. One of the most relevant findings of our study is the large proportion of the population with Covid-19 symptoms who sought and received care in private facilities. The private sector is unregulated, its quality is heterogeneous, and it increases out-of-pocket expenditures. This is an essential aspect for decision-makers to consider as the current health reform moves forward in Mexico.











 nueva página del texto (beta)
nueva página del texto (beta)


