Introduction
Mortality rates of cardiovascular diseases (CVD) have been increasing since 1990 in every region of the world, except for countries with high sociodemographic index.1Particularly in Mexico, CVD has been the main cause of mortality from 1990 to 2012, and have moved from position four to two as a cause for disability-adjusted life years (DALYs) in the same time period.1Several risk calculators estimate the risk of CVD based on well-known risk factors such as age, gender, smoking status, high blood pressure as well as high density lipoprotein cholesterol (HDL-C) and total cholesterol.2,3,4,5Furthermore, dyslipidemias are modifiable risk factors for the development and control of CVD.6 By 1994, high levels of low density lipoproteins (LDL) cholesterol were considered the second most common risk factor for CVD mortality in Mexico and worldwide, only after arterial hypertension.1Also, high cholesterol is one of the main risk factors for mortality in the Mexican population.6Lipid disorders are among the main contributors to the development of atherosclerosis.7
Since 1988, several National surveys in Mexico have been able to document the prevalence of dyslipidemias accounting for sociodemographic variables.8,9,10,11According to the 2006 National Health and Nutrition Survey (Ensanut, by its acronym in Spanish), 43.6% of adults older than 20 years had high levels of cholesterol, 31.5% of triglycerides and 60.5% low levels of HDL-C.11Prevalence of awareness has been reported previously by body mass index categories and diabetes.11However, prevalence of treated and controlled population has not been reported previously.
The present study aims to describe the prevalence of major dyslipidemias in Mexican adults by sociodemographic characteristics, as well as the status of awareness, treatment and control in our population study with Ensanut 2012 data. Furthermore, a comparative of the prevalence through several national surveys since 1994 is presented.
Materials and methods
Study design
This is an analysis of the data collected in the Ensanut 2012. This survey is representative at national, state, urban and rural level. The objective of the Ensanut is to quantify the frequency, distribution and trends of health and nutrition conditions and its determinants. The collection of information from Ensanut 2012 was carried out between October 2011 and May 2012, and information was obtained from 50 528 households, and 96 031 individuals of different age groups. Data on risk factors and sociodemographic characteristics were collected through questionnaires. Also, anthropometric measurements, blood pressure, diet, and physical activity information were collected.
Regarding the information obtained in adults 20 years of age and older, previously trained and standardized personnel made anthropometric and clinical measurements that included: weight, height, waist and hip circumference, blood pressure measurements, as well as validated questionnaires to obtain information on risk factors, personal history of chronic diseases, and affiliation to health systems, among others. Detailed information on the methodology of the survey has been previously published.12
Definition and selection of population
Blood samples were obtained from a random subsample of about 33% calculated through probabilistic methods. The present analysis included 9 566 adults ≥20 years old in Ensanut 2012, with fasting ≥8 hours and with complete information on the concentration of triglycerides, total cholesterol and HDL-C. In addition, the concentrations of non-HDL cholesterol (nonHDL-C) (n=9 565) and LDL-C (n=9 006) were estimated.
Lipid assessment
A blood sample was collected in one tube with ethylenediaminetetra-acetic acid (EDTA) and another sample without any substance to obtain a tube of whole blood and another tube of serum. To obtain serum, samples were centrifuged in-situ. Subsequently, they were stored in cryotubes and transported in nitrogen tanks to the INSP (Mexico’sInstituto Nacional de Salud Pública) laboratory, where they were stored at -70°C until analysis.
A minimum volume of 250 microliters of serum was used to determine triglycerides, total cholesterol and HDL-C concentrations. For the determination of triglycerides, the enzymatic method of glycerol phosphate oxidase was used, for cholesterol the enzymatic colorimetric method of quinonimine was used and HDL-C was determined by the enzymatic method via peroxidase that additionally uses accelerated and selective washing with a surfactant. For these determinations, the Abbott Architect CI8200 equipment was used. Non HDL-C concentrations were obtained from subtracting total cholesterol minus HDL-C concentrations. While concentrations of LDL-C were obtained with the Friedewald formula only in participants with triglycerides levels below 400 mg/dL.13
National Cholesterol Education Program recommendations were used as the criteria to define the presence of dyslipidemias. These thresholds were applied for the analyses of the previous Mexican health surveys; the definitions have not been modified in the current guidelines. Hypercholesterolemia, hypertriglyceridemia, and hypoalphalipoproteinemia were defined as total cholesterol levels equal or greater than 200 mg/dl, triglycerides levels equal or greater than 150 mg/dl and HDL-C levels less than 40 mg/dl, respectively.14In addition, the cut points for elevated non HDL-C and LDL-C were 130 mg/dL and 100 mg/dL, respectively.
Dyslipidemia phenotypes were classified according to combinations of total cholesterol, triglyceride and HDL-C thresholds.
Statistical analysis
The mean values of the lipid traits (mg/dL), the prevalence of dyslipidemias and their phenotypes were obtained in the total sample, by sex, and age group, with their respective confidence intervals. Means were compared with Student’s t-test. The prevalence of dyslipidemias by education level, socioeconomic status (SES), and affiliation to health service, area, and region in the country were estimated.
Prevalence of awareness, treated and controlled adults were calculated in the study population and by gender. Awareness was considered as the self-report of previous diagnosis of hypercholesterolemia. In adults that reported previous diagnosis, treatment for hypercholesterolemia was inquired. This variable included statins (pravastatin, simvastatin, atorvastatin, rosuvastatin or fluvastatin), recommendation to reduce the intake of fat or cholesterol in foods, and to increase physical activity in the last 12 months. Specifically, statin treatment variable was analyzed separately from dietary and physical activity recommendations. Uncontrolled adults were considered as a report of previous diagnosis of hypercholesterolemia or treated with statins, with hypercholesterolemia at the moment of the interview.
Analyses were adjusted for age and design of complex surveys. In order to maintain the representative nature of the sample at the national level and by strata, an expansion factor was included, using the SVY module for complex samples, with the statistical software Stata version 14.
Ethical considerations
During the data collection of the Ensanut 2012, the study subjects were informed of the objective and management of the information as well as the confidentiality of the data. Those who agreed to participate were asked to sign an informed consent form, in which they agreed to the interview and to the blood sample collection. These forms and the draft were approved by the Ethics Committee of the National Institute of Public Health (Instituto Nacional de Salud Pública, INSP). The authors of this manuscript did not have access to the personal data of the study participants.
Results
The overall mean of total cholesterol, HDL-C, LDL-C, nonHDL-C and triglycerides was 180.7 mg/dL (95%CI 178.8-182.6), 39.8 mg/dL (95%CI 39.3-40.2), 106.6 mg/dL (95%CI 105.0-108.2), 141.3 (95%CI 139.5-143.1) and 179.2 (95%CI 174.2-184.3), respectively (table I). After adjusting for age, men had higher mean levels of triglycerides and nonHDL-C, and lower mean levels of HDL-C (p<0.05). Total cholesterol and LDL-C concentrations were significantly higher only in men in the age group of 20-29 years compared to women in the same age group. In contrast, women aged 60-79 had higher mean levels of total cholesterol and women aged 50-79 had higher LDL-C mean levels, compared to men in the same age groups (table I).
table I Lipid concentrations of Mexican adults, stratified by age and sex. Mexico, Ensanut 2012
| Age group (years)* | Both sexes (n= 9 566) Mean (95%CI) | Men (n= 3 716) Mean (95%CI) | Women (n= 5 850) Mean (95%CI) | |||
| Cholesterol (mg/dl) | ||||||
| 20-29 | 164.3 (160.6-168.0) | 168.0 (161.3-174.6) | 160.4 (156.9-163.8)‡ | |||
| 30-39 | 178.1 (174.9-181.4) | 180.9 (174.5-187.3) | 176.1 (172.2-179.9) | |||
| 40-49 | 188.8 (183.9-193.8) | 190.1 (181.9-198.4) | 187.6 (182.0-193.3) | |||
| 50-59 | 191.4 (185.6-197.1) | 188.1 (180.6-195.6) | 194.3 (186.4-202.2) | |||
| 60-69 | 197.8 (192.8-202.8) | 189.6 (182.2-196.9) | 205.0 (198.6-211.5)‡ | |||
| 70-79 | 195.2 (189.1-201.3) | 181.3 (172.9-189.7) | 203.9 (196.4-211.4)‡ | |||
| ≥ 80 | 183.8 (172.1-195.6) | 178.8 (160.1-197.4) | 190.4 (182.4-198.4) | |||
| Total ≥ 20 | 180.7 (178.8-182.6) | 180.9 (177.9-184.0) | 180.5 (178.1-182.9) | |||
| HDL-cholesterol (mg/dl) | ||||||
| 20-29 | 40.1 (39.3-40.9) | 38.3 (37.0-39.6) | 42.0 (41.0-43.0)‡ | |||
| 30-39 | 39.2 (38.3-40.1) | 36.3 (35.1-37.5) | 41.4 (40.1-42.6)‡ | |||
| 40-49 | 38.7 (37.8-39.6) | 36.5 (35.4-37.7) | 40.7 (39.5-41.9)‡ | |||
| 50-59 | 38.6 (37.5-39.7) | 35.2 (33.9-36.5) | 41.6 (40.3-42.9)‡ | |||
| 60-69 | 41.6 (40.6-42.7) | 40.1 (38.8-41.3) | 43.0 (41.5-44.5)‡ | |||
| 70-79 | 44.4 (41.7-47.1) | 41.0 (38.4-43.5) | 46.6 (42.9-50.3)‡ | |||
| ≥ 80 | 40.7 (38.1-43.3) | 37.9 (34.4-41.3) | 44.3 (41.8-46.9)‡ | |||
| Total ≥ 20 | 39.8 (39.3-40.2) | 37.3 (36.7-37.9) | 41.9 (41.3-42.6)‡ | |||
| Triglycerides (mg/dl) | ||||||
| 20-29 | 149.5 (140.0-159.1) | 167.3 (150.0-184.6) | 130.5 (122.6-138.5)‡ | |||
| 30-39 | 176.0 (167.4-184.6) | 205.4 (189.5-221.3) | 154.2 (144.6-163.8)‡ | |||
| 40-49 | 207.3 (195.3-219.4) | 220.2 (200.4-239.9) | 195.6 (181.7-209.5)‡ | |||
| 50-59 | 206.6 (190.9-222.3) | 243.3 (214.3-272.3) | 173.8 (162.3-185.2)‡ | |||
| 60-69 | 181.8 (170.9-192.6) | 178.8 (163.5-194.1) | 184.4 (169.0-199.7) | |||
| 70-79 | 171.0 (157.2-184.9) | 164.3 (142.6-185.9) | 175.3 (156.6-193.9) | |||
| ≥ 80 | 187.3 (151.6-222.9) | 203.4 (146.6-260.1) | 166.3 (153.6-178.9) | |||
| Total ≥ 20 | 179.2 (174.2-184.3) | 199.0 (189.9-208.1) | 161.7 (156.8-166.6)‡ | |||
| Non-HDL-cholesterol (mg/dl) | (n = 9 565) | (n = 3 715) | (n = 5 850) | |||
| 20-29 | 125.3 (122.2-128.5) | 132.0 (126.6-137.4) | 118.3 (115.0-121.7)‡ | |||
| 30-39 | 138.9 (135.7-142.1) | 144.6 (138.3-150.8) | 134.7 (130.8-138.6)‡ | |||
| 40-49 | 150.1 (145.2-155.1) | 153.6 (145.6-161.6) | 147.0 (140.8-153.1) | |||
| 50-59 | 152.8 (147.4-158.2) | 152.9 (145.4-160.3) | 152.7 (145.4-160.0) | |||
| 60-69 | 156.2 (151.3-161.1) | 149.5 (142.6-156.4) | 162.0 (155.4-168.6)‡ | |||
| 70-79 | 150.8 (145.6-156.0) | 140.3 (131.5-149.2) | 157.3 (151.2-163.5)‡ | |||
| ≥ 80 | 143.1 (133.1-153.1) | 140.9 (124.4-157.3) | 146.1 (138.6-153.5) | |||
| Total ≥ 20 | 141.3 (139.5-143.1) | 144.3 (141.5-147.1) | 138.6 (136.2-141.0)‡ | |||
| LDL-cholesterol (mg/dl) | (n = 9 006) | (n = 3 390) | (n = 5 616) | |||
| 20-29 | 96.5 (94.2-98.8) | 99.4 (95.7-103.2) | 93.5 (90.7-96.4)‡ | |||
| 30-39 | 104.6 (101.8-107.4) | 104.6 (99.2-110.0) | 104.6 (101.4-107.7) | |||
| 40-49 | 110.3 (105.9-114.7) | 110.5 (103.4-117.6) | 110.1 (104.7-115.5) | |||
| 50-59 | 113.7 (108.4-118.9) | 107.1 (100.2-113.9) | 119.0 (112.2-125.7)‡ | |||
| 60-69 | 120.4 (116.6-124.1) | 113.5 (108.5-118.4) | 126.3 (121.3-131.4)‡ | |||
| 70-79 | 117.7 (112.5-122.9) | 107.6 (99.6-115.6) | 124.2 (118.3-130.1)‡ | |||
| ≥ 80 | 107.6 (91.3-123.9) | 102.8 (75.3-130.2) | 113.6 (107.2-120.0) | |||
| Total ≥ 20 | 106.6 (105.0-108.2) | 105.5 (102.9-108.1) | 107.5 (105.4-109.5) |
Lipid concentrations presented as means (95%CI).
*Adults were in a ≥8h fasting state. Estimates were adjusted for age and the complex survey design
‡ p<0.05 compared to men
Ensanut: Encuesta Nacional de Salud y Nutrición
LDL: low density lipoprotein
HDL: high density lipoprotein
Table II shows the prevalence of five lipid abnormalities. The most prevalent dyslipidemia among Mexican adults was hypoalphalipoproteinemia (55.2%, 95% CI 53.2-57.3), followed by high LDL-C (56.1%, 95%CI 53.9-58.2), hypertriglyceridemia (47.4%, 95%CI 45.3-49.6) and hypercholesterolemia (30.6%, 95%CI 28.7-32.6). Regardless of the age group, the prevalence of hypoalphalipoproteinemia was significantly higher in men, with values between 55.5 and 74.0%. Likewise, the prevalence of hypertriglyceridemia was higher in men aged 20-59 years and in the study population (p<0.05). On the other hand, the prevalence of hypercholesterolemia was significantly lower in women aged 20-29 years old and higher in women aged 60 years or older (p<0.05). The highest prevalence of elevated LDL-C was observed in men and women between 60 and 79 years old, with a higher prevalence in women. A higher prevalence of elevated nonHDL-C was found in men and, specifically, men aged 20-39 years old. The highest prevalence of elevated nonHDL-C was observed in women between 70-79 years old (52.5%, 95%CI 42.8-62.1)
table II Prevalence of lipid disorders by age and sex groups in Mexican adults. Mexico, Ensanut 2012
| Age group (years)* | Both sexes (n= 9 566) | Men (n= 3 716) | Women (n= 5 850) | |||
| Cholesterol ≥ 200 mg/dl | ||||||
| 20-29 | 19.2 (16.1-22.6) | 23.4 (18.2-29.4) | 14.7 (11.7-18.3)‡ | |||
| 30-39 | 27.9 (24.2-31.8) | 30.5 (24.5-37.2) | 25.9 (21.4-31.1) | |||
| 40-49 | 37.4 (33.4-41.6) | 40.0 (34.0-46.2) | 35.0 (29.9-40.5) | |||
| 50-59 | 36.8 (31.5-42.4) | 36.9 (29.6-44.8) | 36.7 (29.7-44.4) | |||
| 60-69 | 43.1 (36.8-49.6) | 33.0 (24.4-42.9) | 51.9 (43.1-60.5)‡ | |||
| 70-79 | 45.4 (37.4-53.6) | 28.6 (20.2-38.7) | 55.9 (45.6-65.7)‡ | |||
| ≥ 80 | 32.6 (22.2-45.0) | 20.3 (10.5-35.7) | 48.5 (37.5-59.7)‡ | |||
| Total ≥ 20 | 30.6 (28.7-32.6) | 31.4 (28.5-34.2) | 29.9 (27.5-32.4) | |||
| HDL-cholesterol < 40 mg/dl | ||||||
| 20-29 | 52.3 (47.9-56.6) | 60.6 (53.7-67.1) | 43.3 (38.6-48.2)‡ | |||
| 30-39 | 58.5 (54.3-62.6) | 68.0 (60.6-74.6) | 51.5 (46.2-56.9)‡ | |||
| 40-49 | 58.9 (54.6-63.1) | 68.7 (63.0-73.8) | 50.0 (44.2-55.8)‡ | |||
| 50-59 | 58.7 (53.2-63.9) | 74.0 (67.1-79.9) | 44.9 (37.9-52.1)‡ | |||
| 60-69 | 47.3 (41.2-53.4) | 56.2 (48.5-63.7) | 39.4 (31.4-48.0)‡ | |||
| 70-79 | 41.9 (33.7-50.5) | 55.5 (42.7-67.5) | 33.4 (24.5-43.6)‡ | |||
| ≥ 80 | 51.0 (36.9-65.0) | 61.6 (39.3-79.9) | 37.2 (28.1-47.4)‡ | |||
| Total ≥ 20 | 55.2 (53.2-57.3) | 65.2 (62.1-68.3) | 46.4 (43.7-49.1)‡ | |||
| Triglycerides ≥ 150 mg/dl | ||||||
| 20-29 | 32.3 (28.7-36.1) | 38.7 (32.4-45.4) | 25.5 (21.7-29.7)‡ | |||
| 30-39 | 45.4 (41.2-49.7) | 55.9 (48.3-63.2) | 37.7 (32.9-42.7)‡ | |||
| 40-49 | 58.4 (53.9-62.8) | 63.7 (57.0-69.8) | 53.7 (47.9-59.3)‡ | |||
| 50-59 | 60.1 (54.7-65.3) | 68.5 (60.7-75.4) | 52.6 (45.5-59.6)‡ | |||
| 60-69 | 53.4 (46.1-60.6) | 53.3 (42.1-64.2) | 53.5 (44.2-62.6) | |||
| 70-79 | 51.5 (43.2-59.6) | 48.6 (35.4-62.1) | 53.3 (42.3-64.0) | |||
| ≥ 80 | 51.5 (35.9-66.8) | 58.3 (35.5-78.0) | 42.7 (28.3-58.5) | |||
| Total ≥ 20 | 47.4 (45.3-49.6) | 54.1 (50.9-57.3) | 41.5 (38.9-44.1)‡ | |||
| Non-HDL-cholesterol ≥ 130 mg/dl | (n = 9 565) | (n = 3 715) | (n = 5 850) | |||
| 20-29 | 40.4 (36.6-44.1) | 46.3 (39.7-52.9) | 34.1 (29.7-38.5)‡ | |||
| 30-39 | 57.8 (53.9-61.7) | 63.5 (56.7-70.4) | 53.5 (48.3-58.8)‡ | |||
| 40-49 | 63.7 (59.6-67.9) | 66.8 (60.3-73.2) | 60.9 (55.1-66.8) | |||
| 50-59 | 65.6 (60.5-70.6) | 67.1 (58.6-75.6) | 64.2 (58.0-70.4) | |||
| 60-69 | 69.6 (63.3-75.9) | 67.8 (60.9-74.6) | 71.2 (61.2-81.2) | |||
| 70-79 | 68.9 (62.7-75.1) | 57.1 (45.1-69.1) | 76.3 (68.9-83.7)‡ | |||
| ≥ 80 | 60.7 (44.7-76.7) | 55.6 (29.5-82.0) | 67.0 (58.5-75.6) | |||
| Total ≥ 20 | 56.8 (54.9-58.7) | 59.9 (56.8-63.0) | 54.0 (51.4-56.6)‡ | |||
| LDL-cholesterol ≥ 100 mg/dl | (n = 9 006) | (n = 3 390) | (n = 5 616) | |||
| 20-29 | 41.7 (37.7-45.8) | 45.4 (38.6-52.3) | 38.1 (33.4-42.9) | |||
| 30-39 | 56.8 (52.3-61.1) | 58.2 (50.5-65.5) | 55.8 (50.3-61.1) | |||
| 40-49 | 61.3 (56.7-65.6) | 64.1 (57.0-70.6) | 58.8 (52.5-64.8) | |||
| 50-59 | 61.7 (55.6-67.4) | 55.6 (45.4-65.4) | 66.5 (60.3-72.2) | |||
| 60-69 | 73.1 (68.2-77.5) | 66.4 (59.1-73.0) | 78.9 (72.5-84.1)‡ | |||
| 70-79 | 68.0 (61.2-74.1) | 58.1 (45.8-69.4) | 74.3 (65.7-81.3)‡ | |||
| ≥ 80 | 61.1 (43.7-76.0) | 53.9 (28.1-77.7) | 70.03 (60.5-78.1) | |||
| Total ≥ 20 | 56.1 (53.9-58.2) | 55.8 (52.1-59.5) | 56.3 (53.6-58.9) |
Data are presented as percentages (95%CI).
*Adults were in a ≥8h fasting state. Estimates were adjusted for age and the complex survey design.
‡p<0.05 compared to men.
Ensanut: Encuesta Nacional de Salud y Nutrición
Mixed hyperlipidemia is associated to an atherogenic risk profile (table III). This phenotype was observed in one in every five Mexican adults (women 19.9%, 95%CI 17.8-22.0 vs. men 24.6%, 95%CI 22.1-27.1,p<0.05), with a higher prevalence in the 60-69 years old group. (31.0%, 95%CI 25.6-37.0). Similarly, it was observed that more than one third of the adults had hypertriglyceridemia and hypoalphalipoproteinemia (34.5%, 95%CI 32.5-36.6%), and the prevalence was significantly higher in men compared to women. The highest prevalence of this phenotype was observed in the 50-59 years age group (43.7%, 95%CI 37.9-49.7). Less than half of the Mexican adults had normal levels of triglycerides and total cholesterol (44.1%, 95%CI 42.0-46.1).
table III Prevalence of lipid disorders by phenotypes in Mexican adults. Mexico, Ensanut 2012
| High TG/Low HDL-C | Normal TG/ Low HDL-C | High TG/High Chol | High TG/Normal Chol | Normal TG/High Chol | Normal TG/Normal Chol | |||||||
| Total (n= 9 566) | 34.5 (32.5-36.6) | 20.7 (18.9-22.5) | 22.1 (20.5-23.7) | 25.3 (23.3-27.3) | 8.5 (7.3-9.7) | 44.1 (42.0-46.1) | ||||||
| Men (n= 3 716) | 43.1 (39.8-46.4) | 22.0 (19.3-24.8) | 24.6 (22.1-27.1) | 29.5 (26.3-32.7) | 6.8 (5.0-8.5) | 39.1 (35.9-42.3) | ||||||
| Women (n= 5 850) | 26.9 (24.5-29.3)* | 19.5 (17.3-21.7) | 19.9 (17.8-22.0)* | 21.6 (19.5-23.8)* | 10.0 (8.4-11.7)* | 48.5 (45.9-51.1)* | ||||||
| Age, years‡ | ||||||||||||
| 20-29 | 24.1 (20.8-27.6) | 28.2 (24.3-32.4) | 13.7 (11.1-16.9) | 18.6 (15.8-21.7) | 5.5 (3.9-7.6) | 62.2 (58.2-66.1) | ||||||
| 30-39 | 35.2 (31.3-39.2) | 23.4 (19.8-27.4) | 19.2 (16.6-22.1) | 26.3 (22.7-30.2) | 8.7 (5.9-12.6) | 45.9 (41.7-50.1) | ||||||
| 40-49 | 43.3 (38.8-48.0) | 15.6 (12.7-19.0) | 29.1 (25.3-33.1) | 29.4 (25.1-34.1) | 8.3 (6.7-10.4) | 33.3 (29.2-37.6) | ||||||
| 50-59 | 43.7 (37.9-49.7) | 14.9 (12.0-18.4) | 28.5 (23.7-33.9) | 31.6 (25.8-38.0) | 8.2 (6.0-11.2) | 31.6 (27.1-36.6) | ||||||
| 60-69 | 32.3 (26.8-38.5) | 14.9 (10.6-20.6) | 31.0 (25.6-37.0) | 22.5 (18.0-27.6) | 12.1 (8.8-16.4) | 34.5 (27.1-42.7) | ||||||
| 70-79 | 29.9 (22.2-38.9) | 12.0 (8.2-17.3) | 27.0 (21.1-33.7) | 24.5 (17.1-33.9) | 18.4 (11.6-27.9) | 30.1 (24.2-36.8) | ||||||
| ≥ 80 | 36.8 (21.4-55.4) | 14.2 (8.5-23.0) | 19.7 (13.4-28.0) | 31.8 (16.5-52.4) | 12.9 (6.1-25.0) | 35.6 (24.5-48.6) |
Data are presented as percentages (95%CI).
*p<0.05 compared to men.
‡Adults were in a ≥8h fasting state. Estimates were adjusted for age and the complex survey design.
Ensanut: Encuesta Nacional de Salud y Nutrición
Higher prevalence of hypercholesterolemia, elevated LDL-C and nonHDL-C were observed in adults with high school level compared to adults with studies less than elementary. Hypertriglyceridemia and hypoalphalipoproteinemia lowest prevalences were observed in high SES compared to low SES and medium SES categories, respectively. The prevalence of hypercholesterolemia, elevated LDL-C and nonHDL-C was lower in Mexico City and the metropolitan area, compared to the northern region of the country. On the contrary, higher prevalence was observed in the same region compared to the northern region of the country. Hypertriglyceridemia prevalence was higher in southern and center regions compared to northern region.15
Awareness, treatment and control prevalence are presented in figure 1. Almost one in four Mexican adults had hypercholesterolemia at the moment of the survey and did not reported previous diagnosis (24.2%, 95%CI 22.5-25.9). From those aware of having hypercholesterolemia, less than half did not have treatment. From the treated adults, less than half were controlled at the moment of the survey. There were no statistically significant differences in awareness, treatment and control prevalence between men and women. The prevalences of awareness, treatment and control of dyslipidemia were 12.6, 3.7 and 3.1%, respectively.
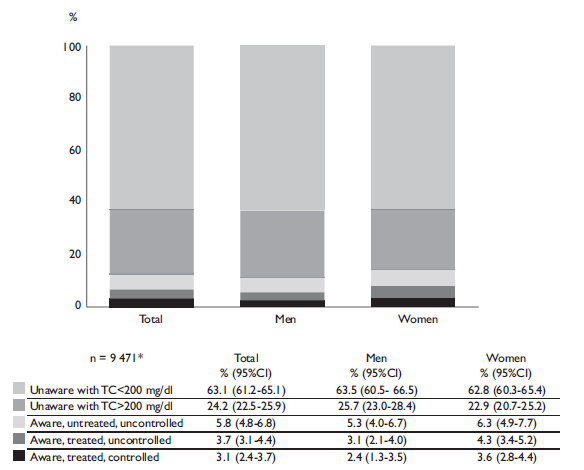
*95 adults did not have information of previous diagnosis
Ensanut MC: Encuesta Nacional de Salud y Nutrición de Medio Camino
Figure 1 Age-adjusted prevalence of awareness, treatment and control of hypercholesterolemia in Mexican adults. Ensanut 2012
Based on four national surveys (ENN 1994, ENSA 2000, Ensanut 2006 and 2012), no trend was observed in the prevalence of hypercholesterolemia, hypertriglyceridemia and hypoalphalipoproteinemia in men and women.15
Discussion
Previous national surveys have reported dyslipidemias as one of the most prevalent cardiovascular disease risk factor in Mexican adults. Our main findings were that hypoalphalipoproteinemia and elevated LDL-C were the most prevalent dyslipidemias among Mexican adults. There were differences in the prevalence of all dyslipidemias by gender, age group, and sociodemographic characteristics. Also, almost a quarter of the population was identified with hypercholesterolemia in the survey without previous diagnosis. A low proportion of awareness is reported, with a very low treatment and control rate. No observable trend along surveys was observed.
One in two Mexican adults has a LDL-C concentration that is considered above the optimal and it is well established that such levels confer an increased risk for cardiovascular disease.11According to the Global Burden of Disease project, LDL-C is ranked as the second metabolic risk factor associated to CVD mortality and DALYs.1Solid evidence from diverse sources associate elevated LDL-C with a higher risk of heart disease. Along with this, clinical trials have demonstrated that therapy focused on reducing LDL level, reduces the risk of coronary heart disease (CHD). The most recent version of current guidelines considers LDL-C as the primary target of therapy, along with a risk assessment that includes other risk factors.16
However, no consensus has been made regarding the use of LDL-C in primary care as a biomarker of atherogenic lipoproteins. LDL-C measurements and calculations have limitations associated, mainly, with triglyceride levels and fasting samples. The recent recommendation for lipid assessment considered non-HDL-C over LDL-C as the best biomarker of atherogenic lipoproteins. The benefits of non-HDL-C are that it only requires total cholesterol and HDL-C for its calculation, and it does not rely on triglyceride levels. NonHDL-C can be used in settings of non-fasting and it does not incur additional expense to the patient or health care system. The prevalence of high nonHDL-C and high LDL-C in our population study are quite similar (56.8% vs. 56.1%), and combined prevalence of high nonHDL-C/LDL-C accounts for almost half of the adults with altered nonHDL-C or LDL-C (47.5%, data not presented in tables). The recommendation for clinical laboratories is to proactively report calculated nonHDL-C with LDL-C on all lipid profiles, and physicians’ conceptual understanding of this combination needs to be addressed.17
Additionally, more than half of the Mexican adults had hypoalphalipoproteinemia. Although in some observational studies, HDL-C levels were considered as an independent risk factor for CHD, the combination of low HDL-C and high triglyceride levels is considered an atherogenic profile. Up to a third of the study population had this profile, with a higher proportion of men compared to women. Currently, no drug therapy is focused to increase HDL-C levels; treatment of hypoalphalipoproteinemia is based on the correction of hypertriglyceridemia, excess body weight, physical inactivity and cigarette smoking. Also, genetic factors and diets with carbohydrate intake >60% of the total energy intake are major determinants of the low concentrations of HDL-cholesterol in Mexicans.16According to national reference data for 2012, obesity and overweight are present in 73% of the adults, 12% of the population are current smokers, 30% of the adults are physically inactive and have diets with excessive intake of added sugars, saturated fats and insufficient intakes of fiber and other micronutrients.12,18In this scenario, the approach to reduce the prevalence of hypoalphalipoproteinemia must consider a therapy that includes lifestyle changes to reduce the risk of CHD.
Differences among age groups and by gender were observed, although no patterns were identified. Education level, SES and region of the country were environmental factors associated with differences in dyslipidemias. Hypercholesterolemia was mainly found in adults with high school level or living in northern Mexico. Hypertriglyceridemia was less prevalent in high SES levels and more prevalent in the southern region of the country. Hypoalphalipoproteinemia prevalence was lower in high SES and in the Mexico City area. The highest prevalence of elevated LDL-C was found in adults with high school or more, or living in the northern region.
Almost 25% of the Mexican adults had hypercholesterolemia at the moment of the interview and did not report a previous diagnosis of this condition. The prevalence of awareness is 12.6% and, although more than half are treated, less than half are controlled. US and China data from national surveys report higher and lower prevalences of hypercholesterolemia, respectively. But the prevalences of awareness in Mexico is a third of the awareness reported in China and 15% of that of the US.19Despite treatment, almost half of the adults have cholesterol levels above 200 mg/dl. The positive effects of statins may not be enough in countries like Mexico, where quality of nutrition is low, and there is still a high prevalence of physical inactivity and sedentarism.18,20,21Along with the low adherence to statin treatment, low adherence to recommendations of diet and physical activity may contribute to our results.22,23,24Previous surveys have not reported this information and acknowledging the situation of undetected, untreated and uncontrolled population may impact the current guidelines and screening processes in primary care medical services. Public policies to increase awareness, access to therapy and sustained control are urgently needed.
Some methodological aspects need to be considered in the interpretation of these results. The design and sampling methods of the study allow having representative results at national and regional level. The selected cut point for high LDL-C considers <100mg/dL as the optimal level for LDL-C.14Future survey analyses may address the comparison of different LDL-C cut points along with different cardiovascular risk profiles to identify the proportion of the population that need to be treated under these considerations. Direct comparisons between surveys are limited by the differences in the analytical methods in each survey. Awareness and treatment variables had self-reported information. Although it is not the most precise method to assess adherence therapy, similar instruments to collect information have been used in surveys in other countries.
Our data confirm that hypertriglyceridemia and elevated LDL-C are highly prevalent in Mexican adults and some environmental characteristics are associated with higher prevalence of dyslipidemias. Screening processes are deficient and preventive strategies should focus on reducing the prevalence of unaware cases of dyslipidemias.











 nueva página del texto (beta)
nueva página del texto (beta)


