Many health problems require immediate attention because of their outstanding severity in terms of both morbidity and mortality, as well as the economic impact. In few situations there is an element of opportunity, where the actions implemented on time (today) will prevent or mitigate the predicted catastrophe; this is the case of antibiotic resistance control.1 Antibiotics have been used for the treatment of infectious diseases, with a great benefit for more than seven decades. Thanks to them, millions of lives have been saved and their current use allows success of transplants, cancer chemotherapy, immunodeficiency ancillary treatment, surgical prophylaxis, and many others. The present standard of medical care demands the control of infectious risks mostly with antibiotics.
Since the discovery of antibiotics, the rapid development of resistance has warned us about their excessive use. To compensate the problem, in the last eight decades, a race has been established between the development of resistance and the production of new antimicrobial drugs, but in the last years the number of useful and effective antibiotics decreased considerably. In the World Health Organization (WHO) analysis in May 2017, there were 42 new therapeutic substances (traditional antibiotics and biologicals) that target high-priority and critical pathogens. It is worth noting that treatment options are lacking, especially for multidrug and extensively drug-resistant Gram-negative pathogens.2 It is urgent to establish a rational regulation that allows humanity to continue to benefit from the antibiotics effectiveness. Controls should be established on the use, production, research and development of antibiotics, and they should even be considered a public good.3
Antimicrobial resistance control requires the understanding of a global phenomenon, with multiple interrelated areas or activities: the environment, agricultural production, practice of medicine and food production. One of the main interventions is to achieve a safe and appropriate antibiotic use. A local, regional and national antimicrobial resistance surveillance network is necessary as one of the first steps.
The Universidad Nacional Autónoma de México (UNAM), aware of the challenge that this problem represents for the public health, has proposed through the University Program of Health Research (Programa Universitario de Investigación en Salud, PUIS), an action plan to control antimicrobial resistance in México. As part of the initial activities of this plan, health personnel were invited to collect and share information to establish the current status of antimicrobial resistance and obtained basal data on antibiotic consumption in a network of hospitals in Mexico (PUCRA network for its acronym in Spanish Plan Universitario de Control de la Resistencia Antimicrobiana).
Materials and methods
Second and tertiary-care level hospitals were invited to participate in the PUCRA network. Twenty centers agreed to voluntarily provide information. Selection of participant centers was by convenience. A retrospective observational study was conducted with the information of the antimicrobial resistance patterns of isolated microorganisms from blood cultures during 2016 and 2017, focused on the ESKAPE group pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter spp.). Also, antimicrobial resistance patterns of Escherichia coli and Klebsiella pneumoniae isolates obtained from urine cultures in the same period were registered.
Bacterial isolates were identified by automated microbial identification systems, including MALDI TOF VITEK MS in four hospitals, VITEK 2 in thirteen hospitals (bioMérieux Marcy l’ Etoile, France), BD Phoenix in three (Becton-Dickinson Sparks, MD, USA), MicroScan autoSCAN-4 in two, WalkAway 96 plus in one (Beckman Coulter Brea, California, USA), and Aris Sensititre in one (Thermo-Fisher Scientific Waltham, Massachusetts, USA). Two hospitals reported having more than one identification system. Antimicrobial susceptibility testing was performed by automated systems VITEK 2 in 12 hospitals (bioMérieux), BD Phoenix in three (Becton-Dickinson), MicroScan autoSCAN-4 in one, WalkAway 96 plus in one (Beckman Coulter), and Aris Sensititre in one (Thermo-Fisher Scientific). Kirby-Bauer disk diffusion susceptibility method was used in five hospitals, broth microdilution method in one, and E-test gradient minimal inhibitory concentration in two (bioMérieux). All the participating centers follow the Clinical and Laboratory Standards Institute (CLSI) criteria to report the isolate as susceptible or resistant.4 A database was created in excel to store all data. Each center selected and sent information of the first isolate of a patient. Internal quality controls are performed periodically in all laboratories of the network.
Hospitals reported indicators (number of beds, occupancy rate, and discharges), and were classified according to size: group I: hospitals with 100 to 200 beds, group II: hospitals with 201 to 500 beds and group III: hospitals with more than 500 beds. Group I included one general hospital and eight high specialty hospital (one pediatric); group II included one general (regional) hospital and three high specialty hospital (one pediatric) and group III two general hospitals. General and regional hospitals provide 2nd and 3rd level care.
The pharmacy department (in some cases the administrative department) gave the information of the annual units of medication consumed. Antibiotic consumption (J01 systemic use) was calculated for each hospital and expressed in defined daily dose (DDD)/100 occupied bed-days (OBD), according to the formula: DDD/100 OBD= (consumption/DDD) x (100/OBD). Consumption was transformed into DDD dividing the total grams/DDD, and the OBD was obtained multiplying the number of beds by the occupancy rate and by the number of days in the analyzed period (one year 2017). The methodology employed was the Anatomical Therapeutic Chemical (ATC)/DDD (defined daily dose) system, developed by the Drug Utilization Research Group and the Nordic Council of Medicines, updated by the WHO’s International Working Group.5 Consumption by hospital departments was not recorded.
Statistical analysis
Numeral data was expressed with median, percentages and minimum and maximum values. For antimicrobial consumption data was expressed in median and 95% confidence intervals and presented for each hospital in DDD/100 OBD. Comparison for medians among groups were done with Mann-Whitney U test. A p value less than 0.5 was considered statistically significant.
Results
Information was reported by 20 participant hospitals: 12 highly specialized hospitals (including three pediatric hospitals), seven general hospitals, and one private hospital, which provided data on the 2016 and 2017 antimicrobial susceptibility profiles. The hospitals had a total annual median of 7 185 discharges. Twelve hospitals are located in Mexico City, two in Guadalajara, Jalisco; two in León, Guanajuato; one in Durango, Durango; one in the State of Mexico, one in Monterrey, Nuevo León and one in Acapulco, Guerrero. General hospitals and regional hospitals provide 2nd and 3rd level care.
The hospitals reported processing an annual median of 3 443 blood cultures (minimum 1 085-14 500 maximum) with a median of positivity of 15% (5-25%).
Blood culture isolates
Number of isolates per hospital varied from 28 to 956. A total of 4 382 blood isolates were obtained: Escherichia coli 1 467, Klebsiella pneumoniae 886, Staphylococcus aureus 848, Pseudomonas aeruginosa 586, Acinetobacter baumannii 317 and Enterobacter cloacae 278.
Escherichia coli and Klebsiella pneumoniae antimicrobial resistance were high for most drugs tested (>30%), only for ertapenem, meropenem and amikacin median resistance values were <20%. For Enterobacter cloacae isolates, the median resistance value for ciprofloxacin and cefepime was <20%. For the three microorganisms, median percentage resistance for piperacillin/tazobactam was 23 to 26 (table I).
Table I Median percentage of antimicrobial resistance in 2 631 Enterobacteriaceae isolates obtained from blood cultures during 2016 and 2017 at 20 participant hospitals in Mexico
| Antimicrobials | Escherichia coli N=1467 | Klebsiella pneumoniae N=886 | Enterobacter cloacae N=278 | ||||||
| Number of resistant strains | Median percentage | Minimum and maximum values % | Number of resistant strains | Median percentage | Minimum and maximum values % | Number of resistant strains | Median percentage | Minimum and maximum values % | |
| Ampicillin | 1 276 | 88 | 77-100 | 877 | 100 | 91-100 | |||
| Ampicillin-sulbactam | 1 115 | 76 | 55-82 | 691 | 75 | 62-100 | NA | ||
| Cefuroxime | 908 | 69 | 48-89 | 556 | 65 | 33-100 | |||
| Cefepime | 908 | 69 | 48-89 | 556 | 65 | 33-100 | 150 | 17 | 2.5-24 |
| Ceftazidime | 908 | 69 | 48-89 | 556 | 65 | 33-100 | ND | ||
| Cefotaxime/Ceftriaxone | 908 | 69 | 48-89 | 556 | 65 | 33-100 | 78 | 34.5 | 26-41 |
| Ertapenem | 44 | 0 | 0-6 | 97 | 0 | 0-14 | 17 | 0 | 0-11 |
| Meropenem | 44 | 0 | 0-5 | 132 | 4 | 0-27 | 14 | 3 | 0-17 |
| Piperacillin-tazobactam | 308 | 23 | 7-32 | 230 | 26 | 0-37 | 53 | 23.5 | 7.5-30 |
| Amikacin | 29 | 2 | 0-8 | 89 | 6.5 | 0-8 | 27 | 0 | 0-32 |
| Ciprofloxacin | 953 | 70 | 40-93 | 336 | 41 | 9-63 | 27 | 5.4 | 0-22 |
NA: not applicable. ND: No data available
Pseudomonas aeruginosa was resistant to 4/6 first line antimicrobials, with a median from 22 to 30%, for amikacin and ciprofloxacin median resistance was <20%. A.baumannii isolates had > 20% median resistance to all antimicrobials tested, and even though small size hospitals reported 0% antimicrobial resistance in their isolates (usually less than 20), larger hospitals informed maximum values of antimicrobial resistance of 80 to 100% (table II).
Table II Median percentage of antimicrobial resistance in 903 non-fermenting Gram-negative bacilli isolates from blood cultures during 2016 and 2017 at 20 participant hospitals in Mexico
| Antimicrobial | Pseudomonas aeruginosaN=586 | Acinetobacter baumanniiN=317 | ||||
| Number of resistant strains | Median percentage | Minimum and maximum values % | Number of resistant strains | Median percentage | Minimum and maximum values % | |
| Ampicillin-sulbactam | NA | 206 | 44 | 0-88 | ||
| Cefepime | 167 | 22 | 1-77 | 244 | 68 | 0-100 |
| Ceftazidime | 193 | 24 | 1-48 | ND | ||
| Meropenem | 210 | 30 | 3-100 | 104/153* | 44 | 0-90 |
| Piperacillin-tazobactam | 176 | 22 | 2-63 | 228 | 60 | 0-100 |
| Amikacin | 146 | 15 | 0-82 | 196 | 47 | 12.5-98 |
| Ciprofloxacin | 158 | 18 | 1-82 | 238 | 70.5 | 0-88 |
NA: not applicable. ND: No data available * For meropenem a reduced number of isolates were tested.
Staphylococcus aureus ranked third in frequency of isolation in blood cultures. Of them, a median of 20.5% was oxacillin resistant (0-67%). For ciprofloxacin, clindamycin and erythromycin median resistance was >30% (0-100%), and for the rest of the antimicrobials tested <10%. This microorganism had the largest number of in vitro active drugs, but some hospital reported high resistance to some antimicrobials (>60%) (table III).
Table III Median percentage of antimicrobial resistance in 848 strains of Staphylococcus aureus isolates from blood cultures during 2016 and 2017 at 20 participant hospitals in Mexico
| Antimicrobial | Number of resistant strains | Median percentage | Minimum and maximum values % |
| Oxacillin | 239 | 20.5 | 0-67 |
| Ciprofloxacin | 279 | 33 | 16-100 |
| Clindamycin | 325 | 36 | 0-66 |
| Erythromycin | 348 | 35 | 0-70 |
| Gentamicin | 132 | 9.5 | 0-50 |
| Linezolid | 2 | 0 | 0-1 |
| Rifampicin | 34 | 0 | 0-12 |
| TMP/SMX* | 86 | 4.5 | 0-43 |
| Vancomycin | 3 | 0 | 0-4 |
* Trimethoprim/sulfamethoxazole
Isolates from urine cultures
A total of 12 151 isolates from urine cultures were reported, 90% of them corresponded to E. coli and 10% to Klebsiella pneumoniae. For E.coli median resistance to amikacin, imipenem, meropenem and nitrofurantoin was <10%. Klebsiella pneumoniae isolates also showed low resistance to amikacin and carbapenems, but nitrofurantoin median resistance was 52%. For both enterobacteriacea, median resistance to cephalosporins, ciprofloxacin and trimethoprim/sulfamethoxazole was >40% (table IV).
Table IV Median percentage of antimicrobial resistance in Escherichia coli and Klebsiella pneumoniae isolated from urine cultures during 2016 and 2017 at 20 participant hospitals in Mexico
| Antimicrobial | Escherichia coli N=11 056 | Klebsiella pneumoniaeN=1 095 | ||||
| Number of resistant strains | Median percentage | Minimum and maximum values % | Number of resistant strains | Median percentage | Minimum and maximum values % | |
| Amikacin | 303 | 2.5 | 0-15 | 98 | 4.5 | 0-39 |
| Ampicillin | 8 734 | 81 | 70-91 | 1052 | 100 | 90-100 |
| Cefuroxime | 5 322 | 48 | 33-62 | 624 | 57.5 | 35-91 |
| Cefotaxime/Ceftriaxone | 5 322 | 48 | 33-62 | 624 | 57.5 | 35-91 |
| Ceftazidime | 5 322 | 48 | 33-62 | 624 | 57.5 | 35-91 |
| Cefepime | 5 322 | 48 | 33-62 | 624 | 57.5 | 35-91 |
| Imipenem | 442 | 0.8 | 0-23 | 142 | 9.2 | 0-35 |
| Meropenem | 155 | 0.6 | 0-23 | 120 | 6.5 | 0-40 |
| Ciprofloxacin | 7 105 | 65 | 49-73 | 508 | 49 | 10-77 |
| Nitrofurantoin | 718 | 8.5 | 4-68 | 613 | 52 | 12-76 |
| TMP/SMX* | 6 191 | 57 | 24-74 | 655 | 62.5 | 39-91 |
*Trimethoprim/sulfamethoxazole
Antimicrobial consumption
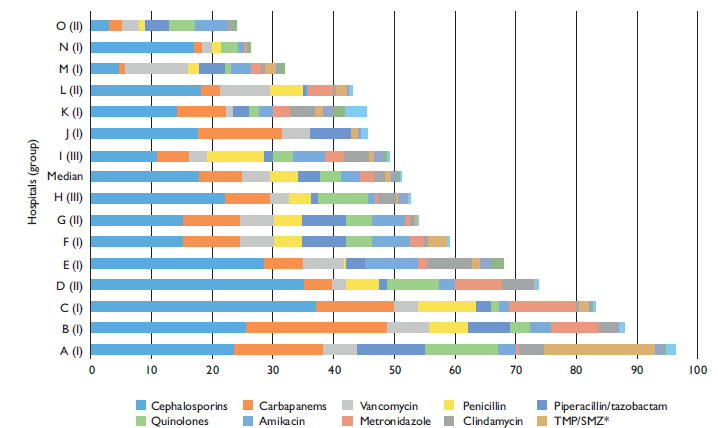
Fifteen hospitals reported annual grams’ consumption of systemic antimicrobials (J01) during 2016-2017. The global median antimicrobial consumption was 57.2/100 OBD, 95% Confidence interval (95%CI) 19.05-85.56. For group I, consumption was 75.56/100 OBD, (95%CI 38.28-85.56); for group II, 47.8/100 OBD (95%CI: 19.05-76.9) and for group III, 47.71/100 OBD (95%CI: 31.62-63.78). Statistically significant difference was found for group I (p=0.002), compared with groups II and III (Mann-Whitney U test).
Antimicrobials with higher consumption were cephalosporins: cephalothin, cefepime, cefotaxime, ceftazidime, and ceftriaxone (ATC codes J01DB03, J01DE01, J01DD01, J01DD02, J01DD04, respectively), with a median of 17.82, 95%CI 13.95-24.45; carbapenems: ertapenem, imipenem and meropenem (ATC codes J01DH03, J01DH51, J01DH02) median 7.08, 95%CI 4.9-11.37, and vancomycin (ATC code J01XA01) median 4.52, 95%CI 3.38-6.28.
Total consumption in DDD/100 OBD for systemic antibiotics is showed for each hospital in figure 1.
Discussion
This report summarizes a recent information of antimicrobial resistance in a network of hospitals in our country, also, the global consumption of antibiotics was calculated for a proportion of them (15/20).
The antimicrobial resistance in Enterobacteriaceae was very high. Escherichia coli, the most frequently isolated pathogen in blood cultures, have high resistance to third and fourth generation cephalosporins, ciprofloxacin and piperacillin/tazobactam leaving the carbapenems as the only treatment option for a bacteriemia/sepsis episode. It is relevant that the amikacin resistance is very low despite its use for so many years, and it could be considered a good alternative in combination with another antibiotics.
The high percentage of resistance to betalactams, cephalosporins, ciprofloxacin, and moderate resistance to piperacillin/tazobactam is evident for K. pneumoniae. Also for this enterobacteria, the carbapenems and amikacin showed the lowest percentage of resistance.
Enterobacter cloacae showed a moderate to low resistance percentage, to carbapenems, ciprofloxacin, amikacin and cefepime, that could be useful drugs, and in second place cefotaxime and piperacillin/tazobactam.
Acinetobacter baumannii isolates show the highest levels of resistance for all antimicrobials, fortunately, its presence seems to be circumscribed to some hospitals in the network. In many countries of the world A. baumannii is one of the most resistant Gram negative bacteria.6 For severe infections, treatment with a few antimicrobials, such as colistin and tigecycline is recommended in combination with other drugs. One limitation of this study was the lack of information on susceptibility for these antibiotics. Another Mexican surveillance network recently published their results of antimicrobial resistance in isolates from a 6-month period including 47 laboratories, they found a high resistance level to all antibiotics tested for Acinetobacter baumannii, but also, information of susceptibility to colistin and tigecycline is lacking.7
When analyzing the resistance in Pseudomonas aeruginosa isolates, there was a great variability, with a wide range of antimicrobial resistance percentages in different hospitals. The higher resistance was observed to carbapenems, with an intermediate median percentage of resistance to first line antimicrobials (piperacillin/tazobactam, cefepime, and cetazidime). The Gram-negative non-fermenting bacilli represent the greatest threat to hospitals, as occurs worldwide. This problem has been favored by the increased consumption of carbapenems.8
For Staphylococcus aureus, the resistance levels were similar to other reports worldwide and the Mexican Network for the Research and Surveillance of Drug Resistance,9,7with good susceptibility to cotrimoxazole and rifampicin, and resistance to oxacillin in around 20%. According to the antibiotic consumption data of our network, vancomycin was the 3rd most prescribed antimicrobial. There is no reason for the use of vancomycin as empirical treatment. Other less expensive and less toxic antibiotics can be used alone or in combination for the treatment of infections due to Staphylococcus aureus.
In urine cultures, an optimal range of nitrofurantoin activity was found for Escherichia coli. The resistance levels to ciprofloxacin, cephalosporins and TMP/SMX were very high, precluding their use as empiric therapy in low urinary tract infections. In our country, according to these results, it is necessary to update the clinical practice guidelines.10,11The use of nitrofurantoin in cases of acute uncomplicated urinary tract infections should be promoted and reserve other active antimicrobials for pyelonephritis and complicated infections. In our population there is an excessive use of quinolones in the management of low and high urinary tract infection, which should be avoided. There are other antimicrobials, as fosfomycin, that have been recommended for the treatment of acute lower urinary tract infection. A susceptibility review is necessary.
Simultaneously, as is shown, the level of antibiotic consumption is very high in most of the participating hospitals, with the exception of two highly specialized hospitals (cardiology), where only one patient in every five admissions receive antibiotics. In contrast, in other eight institutions more than 50% of the patients receive at least one antibiotic (figure 1).
Methods to register antibiotic consumption vary considerably, as Bittermann and colleagues found in a recent systematic review of 80 studies concluding on the need to standardize the reporting methodology.12 We use the Anatomical Therapeutic Chemical (ATC)/DDD system. In this report, the results are shown as baseline information, which may be used in the future to improve the registration, discriminate among hospital areas and type of hospital, and compare the results with other national and international hospitals. Several studies have been carried out to associate or relate the consumption of antibiotics and risk of increase in antimicrobial resistance. Klein and colleagues tracked antibiotic consumption patterns in 76 countries, between 2000 and 2015, and found that DDD increased 65% (21.1-34.8 billion DDDs), and also antibiotic consumption rate increased 39% (11.3-15.7 DDDs per 1 000 inhabitants per day). The increase was rapid for the last available treatments for multidrug-resistant isolates (oxazolidinones, carbapenems, glycylcyclines, and polimyxins), and even though consumption was superior in high income countries, low income countries showed increased consumption in other antimicrobials (cephalosporins, quinolones, macrolides), as well as the costlier last resource antibiotics.13
Resistance in Gram-negative bacilli is higher than in similar reports from Mexico a few years ago,14 and similar to the recent study from the Mexican Network for the Research and Surveillance of Drug Resistance.7 The limited therapeutic options available lead to an increased and continuous use of carbapenems, with the consequent antibiotic consumption and selection of a new threat: carbapenem resistant Enterobacteriaceae and Gram-negative, non-fermenting bacilli. In a global point-prevalence study including adult hospitals in 53 studies the top three antibiotics prescribed worldwide were penicillins with β-lactamase inhibitors, third-generation cephalosporins, and fluoroquinolones. Carbapenems were most frequently prescribed in Latin America and west and central Asia. The reason for prescribing broad spectrum antimicrobials was the prevalence of extended-beta lactamase producing isolates, but not all prescriptions were endorsed by a clinical practice guideline.15
We recognize that this study has several limitations, some of which are:
1) Participation of hospitals was voluntary, so this is not a representative sample of our country. However, the number of participating states offers a wide geographical distribution.
2) There is a variability in the size of the participating hospitals and the characteristics of the underlying diseases of the patients attended by each center.
3) Bacterial identification systems and susceptibility methods are not identical in all hospitals, however, virtually all used automated systems and internal quality controls are carried out periodically.
4) The information on annual antibiotic consumption offers at this moment raw descriptive data, which allows to know the variability in type and quantities of antibiotics used in the participating institutions.
5) In this report, the bacterial isolates of health-care associated infections could not be presented and analyzed separately.
The present report is not a representative sample from all the hospitals in Mexico, but gave us a sound perspective on the severity of antimicrobial resistance and the trends in antibiotic consumption. We hope this information will be useful as a baseline to plan and consolidate the interventions.











 nueva página del texto (beta)
nueva página del texto (beta)