Introduction
Worldwide, hearing and visual impairments are becoming an increasing burden of disability for public health systems due to the growth and aging of populations. Both are non-lethal impairments that have negative effects on quality of life and cognitive, psychosocial, and functional health; and they increase the risk of mortality as well.1,2,3,4Hearing loss has been associated with several chronic diseases, such as diabetes and hypertension, and it is caused by increased exposure to noisy environments, longer life expectancy, and ear infections, among other risk factors.5,6Visual impairment is also associated with aging, but it may also be caused by some infections, nutritional deficiencies, metabolic causes, among other factors.7,8However, these impairments are preventable, avoidable, or treatable with effective medical or surgical interventions that can reduce the severity and magnitude of the disability.
According to data from the World Health Organization (WHO), by 2012, 328.5 (15%) million people 15 years and older were affected by hearing loss worldwide, of whom 164.5 million (50%) were 65 years or older. Prevalence is higher in low- and middle-income (48%) than in high-income countries (18%), particularly in the Latin America and Caribbean region, where it reaches 38%.9,10
As for visual impairment, in 2015, 253 million people worldwide had visual impairment (3.4%); of them, 217 million (2.9%) showed moderate or severe visual loss and 36 million (0.5%) had blindness. The highest proportion of visual impairment and blindness occurred in people older than 50 years (80%) living in low- and middle-income countries (89%). In Latin America and the Caribbean, 14.8 million people had visual impairment (2.4%); 2.3 million (0.4%) corresponded to blindness and 12.5 million (2%) to moderate or severe visual loss.8,11
On the other hand, the presence of hearing loss with concurrent visual impairment is frequent in adult population; the reported prevalence of both impairments combined varies between 3.4 and 7%.4,12,13Because of the impact of both hearing and visual impairment in the quality of life of patients, the assessment of the risk profile of patients with both disabilities could help to implement suitable strategies for prevention of these conditions.
In this study, we aimed to determine the prevalence of self-reported hearing loss alone and combined with visual impairment and the associated risk factors among adults aged 50 years and older from the state of Tlaxcala in East-Central Mexico.
Materials and methods
Study population
A population-based cross-sectional study was conducted between July and October 2013 in Tlaxcala, in Central Mexico, to determine the prevalence of hearing loss and visual impairment among persons 50 years of age and older. A multistage cluster random sampling design was used with 37 clusters selected from 38 municipalities. Of 2 163 individuals potentially eligible, only 1 617 (75%) agreed to participate in the study. Information about hearing loss was available for 1 511 individuals (93.4%). The assessments were performed at the participant’s home by trained and standardized interviewers who administered questionnaires on general health and hearing impairment and measured visual acuity. The study was performed in accordance with the guidelines of the Declaration of Helsinki14and approved by the Institutional Review Boards of Research, Ethics and Biosecurity of the Conde de Valenciana Institute of Ophthalmology. All participants signed an informed consent form for the interview.
Sociodemographic and clinical variables
Sociodemographic variables included age, sex, literacy (yes/no), schooling (none/elementary or greater), area of residence (rural/urban), level of marginalization (very low/low/medium) as defined by Mexico’s National Population Council (Conapo),15and social security affiliation (yes/no). Clinical variables included self-report on general health (good/regular/poor), diabetes (yes/no), and hypertension (yes/no). Diabetes was defined as fasting serum glucose >7.8 mmol/l (126 mg/dl) or previous medical diagnosis of diabetes. Hypertension was defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg, or previous medical diagnosis of hypertension. Chronic comorbidities were defined as the presence of diabetes or hypertension.
Hearing loss assessment
Hearing loss was measured using the validated Spanish Hearing Impairment Inventory for the Elderly (SHIIE), which consists of 10 items and is designed to identify non-institutionalized individuals who should be referred to an audiological assessment.16The questionnaire has an internal consistency of 0.956 and a sensitivity and specificity of 80 and 58%, respectively.17Response options for the SHIIE validated in Spanish are “Yes” (scoring 2 points), “Sometimes” (1 point), and “No” (0 points) within a 20-point range. A score <10 indicates normal hearing and a score ≥10 suggests hearing loss. In individuals with a total score ≥10, and additional question (“Can you understand when someone is speaking to you on the telephone?”) was used to determine the degree of hearing loss. A “Yes” answer indicated mild hearing loss; “Sometimes”, moderate hearing loss; and “No” severe hearing loss.16,18
Visual acuity measurement
Visual acuity was evaluated using a tumbling E chart with and without pinhole correction. Visual acuity in the better eye was classified as follows: blindness (visual acuity worse than 20/400), severe visual disability (worse than 20/200 but better than or equal to 20/400), moderate visual impairment (worse than 20/60 but better than or equal to 20/200), and normal vision (better than or equal to 20/60).19
Data analysis
Hearing loss was classified into the following three categories: normal hearing, mild/moderate hearing loss, and severe hearing loss. Comparisons of different risk factors according to level of hearing loss were done using Pearson Chi2test for categorical variables and analysis of variance (Anova) test for continuous variables. Prevalence with 95% confidence interval (95%CI) was estimated for mild/moderate and severe hearing loss according to age categories and visual acuity (normal, moderate visual impairment, and severe visual impairment/blindness). The risk factors associated with any degree of hearing loss alone or combined with visual impairment were evaluated by logistic and multinomial regression analyses, respectively. The diagnosis of the models was made using the Hosmer-Lemeshow Goodness-of-Fit test and with the analysis of outliers and influential points. All analyses were performed with Stata/MP 15.1 (Stata Corporation, College Station, TX, USA).
Results
Description of the study population
The study included 1 511 persons (611 men [40%] and 900 women [60%]; mean age 66.1 years; s.d. 10.4 years). Hearing status was normal in 1 030 individuals (68.2%), whereas 481 (31.8%) showed some degree of hearing impairment (mild 129 [26.8%], moderate 134 [27.9%], and severe 218 [45.3%]). Hearing loss alone was detected in 415 (86.3%) persons, and combined hearing and visual impairment was observed in 66 (13.7%) individuals. Comparison between persons with normal hearing and those with mild/moderate and severe hearing loss showed that the affected individuals were older (63.7, 64.5, and 68.1%, respectively), self-reported poorer health status (4.2, 6.5, and 11%, respectively), had hypertension (46.1, 50.6, and 56.4%, respectively), and had more severe visual impairment (3.0, 3.8, and 10.6% respectively) and blindness (2.6, 4.6, and 9.6% respectively). Significant differences as regards area of residence, marginalization level, social security affiliation, and chronic comorbidities were also noted (table I).
Table I omparison of demographic and clinical characteristics by hearing loss categories among adults 50 years and older from Tlaxcala, Mexico. July-October, 2013
| Variable | Normal hearing* | Mild/moderate hearing loss* | Severe hearing loss* | P value | ||||
| N=1 030, n (%) | N=263, n (%) | N=218, n (%) | ||||||
| Age (yrs.), mean (s.d.) | 63.7 (9.8) | 64.5 (10.3) | 68.1 (12.3) | <0.001 | ||||
| Sex | ||||||||
| Women | 606 (58.8) | 162 (61.6) | 132 (60.6) | 0.682 | ||||
| Men | 424 (41.2) | 101 (38.4) | 86 (39.4) | |||||
| Literacy | ||||||||
| Yes | 889 (86.3) | 238 (90.5) | 188 (86.2) | 0.184 | ||||
| No | 141 (13.7) | 25 (9.5) | 30 (13.8) | |||||
| Schooling | ||||||||
| None | 228 (22.1) | 57 (21.7) | 37 (17.0) | 0.236 | ||||
| Elementary or higher | 802 (77.9) | 206 (78.3) | 181 (83.0) | |||||
| Area of residence | ||||||||
| Urban | 793 (77.0) | 221 (84.0) | 163 (74.8) | 0.024 | ||||
| Rural | 237 (23.0) | 42 (16.0) | 55 (25.2) | |||||
| Marginalization level | ||||||||
| Very low/low | 887 (86.1) | 246 (93.5) | 186 (85.3) | 0.004 | ||||
| Medium | 143 (13.9) | 17 (6.5) | 32 (14.7) | |||||
| Social security affiliation | ||||||||
| Yes | 318 (30.9) | 105 (39.9) | 82 (37.6) | 0.008 | ||||
| No | 712 (69.1) | 158 (60.1) | 136 (62.4) | |||||
| Self-reported health status | ||||||||
| Good | 575 (55.8) | 107 (40.7) | 87 (39.9) | <0.001 | ||||
| Normal | 412 (40.0) | 139 (52.8) | 107 (49.1) | |||||
| Poor | 43 (4.2) | 17 (6.5) | 24 (11.0) | |||||
| Diabetes | ||||||||
| Yes | 330 (32.0) | 92 (35.0) | 79 (36.2) | 0.385 | ||||
| No | 700 (68.0) | 171 (65.0) | 139 (63.8) | |||||
| Hypertension | ||||||||
| Yes | 475 (46.1) | 133 (50.6) | 123 (56.4) | 0.016 | ||||
| No | 555 (53.9) | 130 (49.4) | 95 (43.6) | |||||
| Hypertension | ||||||||
| Yes | 475 (46.1) | 133 (50.6) | 123 (56.4) | 0.016 | ||||
| No | 555 (53.9) | 130 (49.4) | 95 (43.6) | |||||
| Chronic comorbidities‡ | ||||||||
| Yes | 615 (60.7) | 172 (66.7) | 148 (68.5) | 0.037 | ||||
| No | 398 (39.3) | 86 (33.3) | 68 (31.5) | |||||
| Visual acuity in the better eye§ | ||||||||
| Normal | 972 (94.4) | 241 (91.6) | 174 (79.8) | <0.001 | ||||
| Visual impairment | 58 (5.6) | 22 (8.4) | 44 (20.2) | |||||
*Hearing ability was defined as follows: normal hearing, score <10; mild hearing loss, score ≥10 with no difficulty to understand someone speaking on the telephone; moderate hearing loss, score ≥10 with difficulty sometimes to understand someone speaking on telephone; and severe hearing loss, score ≥10 with difficulty always to understand someone speaking on telephone.
‡Included hypertension and diabetes
§Visual acuity in the better eye was classified as follows: visual impairment, worse than 20/60, and normal vision, better than or equal to 20/60.
Hearing loss and visual impairment
Of a total of 481 (31.8%) persons with hearing loss, 263 (54.7%) had mild/moderate impairment and 218 (45.3%) had severe hearing loss. Of the 415 (86%) individuals with hearing loss alone, 241 (58.1%) had mild/moderate and 174 (41.9%) had severe hearing loss, and of the 66 (13.7%) persons with combined hearing and visual impairment, 22 (33.3%) had mild/moderate hearing impairment and 44 (66.7%) had severe hearing loss. Combined hearing and visual impairment increased with age as follows: 1.6% for those younger than 60 years, 2.8% for those 60 to 69 years, and 9.9% for those 70 years and older.
Prevalence of severe hearing loss also showed a significant trend by age, ranging between 10.7% (95%CI 8.4-13.4) in persons 50 to 59 years and 20.8% (95%CI 17.2-24.9) in those 70 years and older (p trend<0.001) (figure 1). Additionally, an increment in the prevalence of severe hearing loss associated with visual acuity was observed as follows: 12.6% (95%CI 10.9-14.4) in individuals with normal vision, 35% (95%CI 24.0-47.9) in those with moderate visual impairment, and 36% (95%CI 25.1-48.4) in those with severe visual impairment/blindness (p trend<0.001). In contrast, no significant trend in the prevalence of mild/moderate hearing loss by age or visual acuity was observed (figure 2).
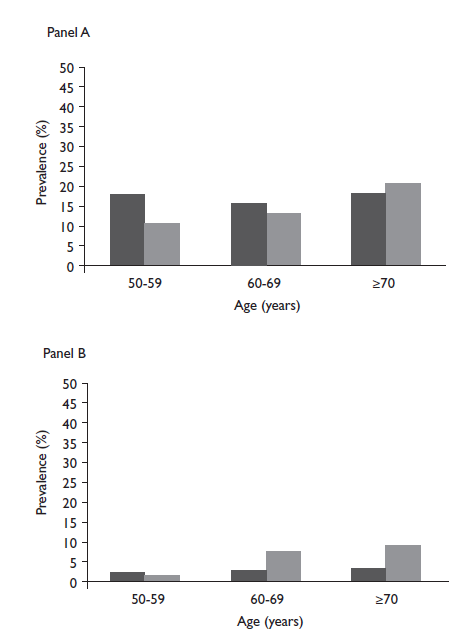
Panel A. For prevalence by age of severe hearing loss, p trend <0.001; and of mild/moderate hearing loss, p trend=0.391. Panel B. For prevalence by age of severe visual impairment//blindness,ptrend<0001; and of mild/moderate visual impairment,p trend<0001.
Figure 1 Prevalence of mild/moderate (black bars) and severe (grey bars) hearing loss (panel A), and mild/moderate (black bars) visual impairment and severe visual impairment/blindness (grey bars) (panel B) by age among adults 50 years and older from Tlaxcala, Mexico. July-October, 2013
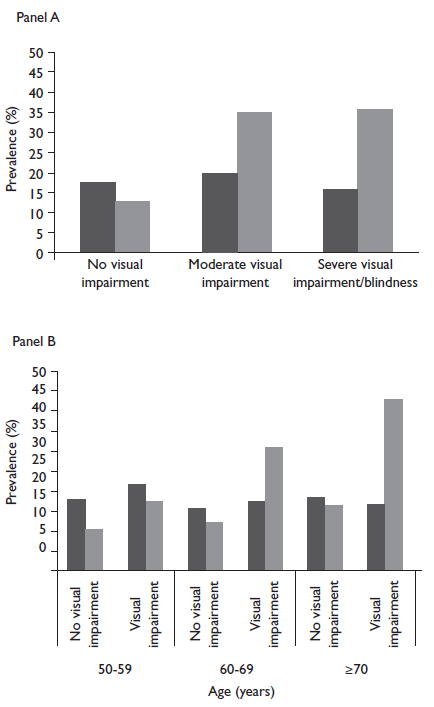
Panel A. For prevalence by visual acuity of severe hearing loss,ptrend <0.001; and of mild/moderate hearing loss,ptrend=0.185. Panel B. For prevalence by age of severe hearing loss with normal vision,ptrend=0.007, and with visual impairment,ptrend=0.022; for prevalence by age of mild/moderate hearing loss with normal vision,p trend=0.555, and with visual impairment, p trend=0.773.
Figure 2 Prevalence of mild/moderate (black bars) and severe (grey bars) hearing loss by visual impairment (panel A), and by visual impairment and age (panel B) among adults 50 years and older from Tlaxcala, Mexico. July-October, 2013
Risk factors associated with hearing loss
The multiple logistic regression model included age, literacy, marginalization level, self-reported health status, chronic comorbidities, and visual impairment. The probability of hearing loss increased with age (per two years, OR=1.04 [95%CI 1.02-1.06]; p<0.001) and was higher in illiterate persons (OR=1.51 [95%CI 1.05-2.15];p=0.024), those who self-reported poor health status (OR=2.04 [95%CI 1.29-3.22];p=0.002), and those with visual impairment (OR=2.22 [95%CI 1.50-3.29]; p<0.001). In the multinomial logistic regression model, the associated risk factors for hearing loss alone were age, literacy, low/very low level of marginalization, and self-reported poor health status. As for hearing loss combined with visual impairment, the associated risk factors were age, self-reported poor health status, and chronic comorbidities, such as diabetes or hypertension (table II).
Table II Risk factors associated with hearing loss alone and combined with visual impairment among adults 50 years and older from Tlaxcala, Mexico. July-october, 2013
| Variables | Hearing loss independent of visual impairment* | Hearing loss alone‡ | Hearing loss combined with visual impairment§ | |||||||||
| Odds ratio (95%CI) | p value | Odds ratio (95%CI) | p value | Odds ratio (95%CI) | p value | |||||||
| Age (per two years) | 1.04 (1.02-1.06) | <0.001 | 1.03 (1.01-1.05) | 0.012 | 1.18 (1.13-1.24) | <0.001 | ||||||
| Literacy# | 1.51 (1.05-2.15) | 0.024 | 1.61 (1.09-2.37) | 0.016 | 0.99 (0.51-1.90) | 0.969 | ||||||
| Low/very low marginalization level# | 1.46 (1.02-2.09) | 0.036 | 1.54 (1.05-2.26) | 0.026 | 0.87 (0.42-1.80) | 0.705 | ||||||
| Self-reported poor health status# | 2.04 (1.29-3.22) | 0.002 | 1.90 (1.17-3.09) | 0.009 | 3.69 (1.66-8.20) | 0.001 | ||||||
| Chronic comorbidities# | 1.20 (0.94-1.51) | 0.140 | 1.13 (0.88-1.44) | 0.332 | 3.64 (1.69-7.81) | 0.001 | ||||||
| Visual impairment# | 2.22 (1.50-3.29) | <0.001 | – | – | – | – | ||||||
*Multiple logistic regression analysis was performed
‡Multinomial logistic regression analysis was done
§Chronic comorbidities included hypertension and diabetes.
#Variable categories: literacy, yes/no (reference); marginalization level, low and very low/medium (reference); self-reported health status, good and normal (reference)/poor; chronic comorbidities, yes/no (reference); visual impairment, yes/no (reference)
Discussion
Sensory function in older adults plays a critical role in their general well-being. Coping with visual and hearing decline represents a great source of stress for older people and may significantly affect their health by association with an array of geriatric problems including falls, injuries, depression, and anxiety.20,21These concerns hinder the capacity of older people to carry out daily activities that relate to personal care and social interaction.
Our study shows that the prevalence of any degree of hearing loss increases with age (10.7% in persons 50-59 years to 20.8% in those 70 years and older) and this increment is more remarkable for severe hearing loss. Several studies have shown that older adults can develop age-related partial or total sensorineural hearing loss, which is neither preventable nor reversible.18In the 2012 National Health and Nutrition Survey in Mexico, only 9.5% of people 60 years and older self-reported hearing loss, with an increase in those 80 years and over (25.7%).22Another study using the Hearing Handicap Inventory for the Elderly-Screening version (HHIE-S) questionnaire reported a prevalence of hearing loss in the age groups 70-79 and 80-92 years of 20.6 and 33.2%, respectively.18In the United States, the National Health and Nutrition Examination Survey (NHANES) study indicated that 30% of adults 60 years and older self-reported hearing loss,23 which increased to 50% in the 80 year and older group.18
Both visual impairment and hearing loss are closely associated with aging and their concurrence has been reported previously.16 Aging of the population is a worldwide demographic process that brings along the potential increase of these impairments together with other comorbidities associated with the elderly population. In our study, the prevalence of hearing loss was significantly higher in individuals with moderate visual impairment (55%) or severe visual impairment/blindness (51.6%) than in those with no visual impairment (29.9%). The prevalence of hearing loss alone and combined with any degree of visual impairment was 27.5 and 4.4%, respectively.
In a multiethnic study, Caban and colleagues reported a prevalence of hearing impairment alone of 27.6 and 36.5% among people ages 65-79 years and 80 years and older, respectively, whereas the prevalence for hearing loss combined with visual impairment was 7.3 and 16.6% for the same age groups, respectively. As for Hispanic people, the prevalence was lower compared with that of non-Hispanics, although Mexican-Americans had the highest prevalence among Hispanics.13Jee and colleagues, in a small study that included individuals 65 years old and over, found a combined prevalence of hearing loss and visual disability of 22.5%.24Likewise, Schneck and colleagues reported that low vision was associated with increased risk of hearing loss in older adults.25
Our study has documented large differences in the prevalence of hearing loss alone or combined with visual impairment in relation to poor health, literacy, and low/very low marginalization level. These variables concur almost universally.26The 2016 Global Burden of Disease Study (GBD) revealed that the state of Tlaxcala and Mexico had higher age-standardized prevalence rates for hearing and visual impairments than the prevalence rates of high income countries, such as United States, Australia, Japan, and Germany, but lower than the prevalence rates of Brazil, Peru, India or the Sub-Saharan countries. The age-standardized prevalence of hearing loss is higher in Bangladesh with 28 178.4 per 100 000 (UI 27 139.1-29 247.1), followed by Pakistan, India, and Sub-Saharan Africa compared with the prevalence rates of Europe, Southeast Asia, and the Americas. However, the prevalence rate in Mexico in 2016 was 19 376.5 per 100 000 (UI 18 593-20 203), which was significantly higher than that reported for Chile, Argentina, United States, and Canada.27
Also, the 2016 GBD study reported the highest age-standardized prevalence rates of blindness and visual impairment in the Sub-Saharan Africa region, particularly in Central African Republic (31 804.4 [UI 30 722.1-32 924.4]) and the Democratic Republic of Congo (31 740 [UI 30 666.8-32 916.2]). Mexico showed an intermediate prevalence rate of 14 762 (UI 14 202.7-15 318.7) in the Americas.27
Our study did not explore the impact of hearing and visual impairment on quality of life or performance of daily activities. Nevertheless, several studies suggest that the combination of hearing loss and visual impairment increases the risk of reduced function in daily life instrumental activities and produces more depression compared with having either condition.28,29,30Older adults with concomitant best-corrected visual impairment and mild hearing loss at baseline had a 2-fold increased risk of experiencing two or more falls five years later,31and dual sensory impairment is associated with lower health status and increased risk of mortality.24,25In contrast, some reports suggest that the main impact is caused by visual impairment, while hearing impairment alone does not further reduce functioning.12,25As for the burden of both hearing loss and visual impairment, from 1990 to 2010 the years lived with disability significantly increased 29.1 and 53.4%, respectively, and from 2006 to 2016, the increment was of 18.8 (UI 17-20.4) and 20.4% (UI 19.1-22), respectively. This has undoubtedly a negative impact on quality of life and entails an increment of costs for public health systems.26,27,32
A limitation of our study was the self-report nature of hearing loss measurement. In audiometric studies, prevalence ranges between 13.3 and 68%,12,13,20,23,28,33,34,35,36whereas in studies using self-report questionnaires prevalence goes from 11.6 to 48.1%.5,20,22,37However, some self-report questionnaires, including the Spanish Hearing Impairment Inventory for the Elderly, have an acceptable accuracy in comparison with pure-tone audiometry in elderly population.16,18The variation on the precision depends on factors such as the questionnaire used and the definition of hearing loss by audiometry (i.e. ear used, best or worst ear, frequency in kHz [kHertz], and threshold level [dB hearing level]). The sensitivity and specificity of some questionnaires is about 80 and 60%, respectively, in comparison with audiometry, and both increase with age.18
In summary, the strong association between hearing loss and visual impairment in older people put them at greater risk of dependency to family and community support. Even though a proportion of these impairments develop as part of the aging process, many of them are avoidable, preventable or treatable with medical or surgical interventions. Both hearing loss and visual impairment affect people’s daily life activities and are tied to social isolation, depression, cognitive dysfunction, and dementia. Therefore, assessing the magnitude of the problem becomes mandatory to implement early interventions that address opportunely this mounting public health concern.











 text new page (beta)
text new page (beta)


