The proportion of people 60 years of age and older is growing faster than other age groups in most countries. Clinical preventive services ([CPS] colorectal, breast, and cervical cancer screenings, influenza and pneumococcal immunizations) reduce rates of premature death and disability in older adults and support healthy aging. Between 30-50% of premature deaths due to cancer are preventable with screening, early diagnosis, and treatment.1 One highly effective CPS with a low use rate is colorectal cancer screening.2
Colorectal cancer is the fourth most common cancer in the Americas, with more than 240 000 new cases and 112 000 deaths occurring each year. By 2030 colorectal cancer deaths are expected to increase by 68%.3,4,5 Screening, such as high-sensitivity fecal occult blood testing (FOBT), fecal immunochemical test (FIT), sigmoidoscopy, or colonoscopy can help detect colorectal cancer at early, treatable stages. Although guidelines vary by country, screening is generally recommended in an average risk population to start at age 50 and continue at regular intervals until age 75.5
In the United States, the use of CPS, including colorectal cancer screening, is below the national health promotion goals set out in Healthy People 2020, especially for ethno-racial minorities. Data from South Los Angeles show that 42% of adults ages 50 years and older had not met colon cancer screening guidelines, 56% had not had a flu vaccine in the past year, and 17% of women ages 50-74 were not up-to-date with breast cancer screening.6 While many interventions to increase CPS use focus on changing practices at primary care sites, such as community health centers (CHC), overcoming the complex barriers to CPS use also benefit from building on community strengths such as social networks, religious and community institutions, and traditional knowledge.7
The goal of the Healthy Aging Partnerships in Prevention Initiative (HAPPI) is to increase the use of a core set of “high value” CPS, including colorectal cancer screening among African American and Latino adults ages 50 years and older who live in South Los Angeles, an underserved low-income area of Los Angeles County, California, USA.
Building a regional collaboration to advance preventive health
HAPPI uses an evidence-based collaboration model, Sickness Prevention Achieved through Regional Collaboration (SPARC),8to mobilize, foster linkages, and leverage existing networks of community-based health, service, non-governmental organizations (NGOs), and government agencies to promote the use of CPS among ethno-racial minority elders. Our approach builds on earlier work, which identified 20 evidence-based community-based interventions that targeted two or more CPS for elders and used a range of educational, motivational, behavioral and psychosocial strategies in diverse community settings (e.g., churches, community centers, etc.).9
Multi-sectoral collaborations increase awareness and use of CPS in underserved communities by building on existing resources and implementing community-wide strategies that are responsive to the local environment. HAPPI’s collaboration includes the Los Angeles County Department of Public Health, Los Angeles City and County Departments of Aging, Southside Coalition of Community Health Centers (eight CHCs with a network of over 35 community- and school-based primary health care clinics), local community-based organizations, and a multidisciplinary group of UCLA investigators.
HAPPI undertook three activities: 1) CHC capacity assessment, 2) CHC and NGO capacity building, and 3) a small grants program that provided seed funding and technical assistance to support eight NGOs in efforts to adapt, implement, evaluate, and maintain culturally-tailored CPS outreach programs. Taken together, these activities fostered ongoing and sustainable community-based efforts to increase CPS use.
The following describes: 1) the formation and expansion of a regional collaboration to increase the use of CPS among the 50+ population in an underserved community; 2) the identification of facilitators and barriers to increasing CPS use, especially colorectal cancer screening; and 3) the success of trainings conducted with CHC providers and with “HAPPI ambassadors” representing 32 NGOs.
Materials and methods
CHC capacity assessment
We conducted a capacity assessment for CPS delivery with five CHCs by establishing baseline CPS utilization rates and identifying barriers and facilitators to increasing CPS use through key informant interviews with CHC personnel. Informed consent was obtained from all study participants. Data collection activities were approved by the UCLA Institutional Review Board, IRB#15-000368.
Establishing baseline rates of CPS utilization
We obtained de-identified 2014 data representing patients age 50+ from five CHCs, including: 1) demographics; 2) receipt of six “high-value” CPS (influenza and pneumococcal vaccinations, cholesterol screening, colorectal, breast and cervical cancer screenings) and 3) insurance type and status. We used the 2014 U.S. Preventive Services Task Force A and B guidelines10,11 as benchmarks to determine the proportion of patients “up-to-date” on the selected CPS. We used SPSS version 23.0 for Windows for analysis (SPSS, Inc., Chicago, IL).
Key informant interviews with CHC personnel
To learn about barriers and facilitators to CPS delivery and use, we conducted 34 in-person key informant interviews with CHC personnel (healthcare providers, chief executive officers, chief medical officers, chief financial officers, quality improvement directors, referral coordinators, and community outreach specialists) from five CHCs. We inquired about organizational context; current practices related to serving older adults, including marketing and outreach efforts; how CPS were monitored and evaluated; and strategies used for engagement with community partners and collaborators.
Interviews were audiotaped and independently summarized by two research members. A matrix was developed to organize the data across CHCs and identify emerging themes (e.g., CHC culture, CPS delivery, CPS referrals, and geriatric training) by CPS at individual, organizational, and system levels.
CHC capacity building
In-service training of CHCs
We developed and delivered training for professionals at the CHCs to promote CPS delivery. The curriculum was informed by a multidisciplinary competency framework developed by the Partnership for Health and Aging12 and by findings from the CHC capacity assessment.
The training was directed at system-level and practice-based changes to increase utilization of CPS and included seven competency domains (table I).
Table 1 Healthy Aging Partnerships in Prevention Initiative. Curriculum domains in the inservice training of community health centers (CHC) professionals. October 2015-June 2016, South Los Angeles, California, USA
| Competency Domains | Description | |
| 1 | Overview of older adult demographics and health profile | |
| 2 | Adults 50+ CPS recommendations | |
| 3 | Adults 50+ CPS receipt, barriers and facilitators | |
| 4 | Evidence- and community-based CPS programs for adults 50+ | |
| 5 | Best practices in CHC services and systems to support CPS delivery to adults 50+ | |
| 6 | Older adult continuum of care | |
| 7 | Older adult community-based support services | |
The training format included lectures and group discussions about modifications to CHC practices and systems needed to align with current standards of care for older adults, and possible roles for NGO-CHC partnerships in boosting CPS utilization. Each group discussion used a worksheet as a basis for developing an “action plan” that could be implemented given the CHC’s capacity and resources (table II).
Table II Healthy Aging Partnerships in Prevention Initiative (HAPPI). Capacity building training activities delivered to community health centers (CHC) and non-governmental organizations (NGO). October 2015-June 2016, South Los Angeles, California, USA
| CHC capacity building | NGO capacity building | |||||
| community clinic in-service training | HAPPI Ambassador’s training | |||||
| October 2015-June 2016 | April 2016-May 2016 | |||||
| Agenda items | Type of instruction | Agenda items | Type of instruction | |||
| Day 1 | Day 1 | Activity #1: Group discussion: healthy | ||||
| Introduction to project and clinic role | Didactic | Welcome and participant introductions | aging in my community | |||
| Overview of older adult demographics and health | Didactic | HAPPI project overview | Didactic | |||
| Adults 50+ clinical preventive services (CPS) recommendations, system-level perspectives | Didactic | Healthy aging overview | Didactic | |||
| Adults 50+ CPS receipt, barriers and facilitators | Participant discussion of perceptions of clinic barriers and facilitators | Clinical preventive services | Didactic | |||
| Action Plan Development:* Best practices in clinic services and systems to support CPS delivery to adults 50+ | Interactive discussion | Clinic and Community CPS Action Plan | Activity #2: Small group work | |||
| Day 2 | ||||||
| Overview of community training and small grant funding opportunities through the HAPPI Project | Didactic | Community resource panel | Interactive | |||
| Review CHC’s Training Session Day 1 | Didactic | Community-Clinic CPS Education and Promotion Action Plan§ | Activity #3: Small group work: | |||
| Opportunities to increase CPS use by adults 50+ through collaborations with non-governmental organizations | Didactic | CPS Community Education and Promotion | Didactic | |||
| Role of non-governmental organizations in promoting CPS | Didactic | Homework: Planning Assignment≠ | ||||
| Clinic-community linkages: reaching people where they are | Didactic | Day 2 Review | Participants provide overview of their workshop plan and discuss barriers and solutions to implementing their workshop. | |||
| Asset map tool for identifying organizations in your area (e.g., multi-purpose senior centers as clinic partners) | Didactic | Beyond the training: Evidence based interventions to sustain CPS best practices | Didactic | |||
| Evidence-based programs that promote CPS use by adults 50+ in the community | Didactic | EBI “Fit” activity | Activity #1: Working in small groups, identify an EBI model to implement in your community | |||
| Older adult community support services (e.g., specific resources available to clinics including referrals to senior services, dept of aging resources) | Didactic | Workshop presentations | Participants deliver 5-minute presentations for planned workshop audiences | |||
| Community Engagement Action Plan: ‡ Group discussion of “next steps” to connect clinics with community services to promote CPS | Interactive - Small groups report back to larger group | Next steps | Submitting your HAPPI small grant application | |||
Clinic training
*Action Plan Development: Participant discussion of systems improvement opportunities based on specific clinic data and selected CPS focus for improvement (decided by leadership in advance). To document plans, please complete the Action Plan Worksheet Part 1.
‡Community Engagement Action Plan: Participants were asked to think about Day 1 and about community resources that they would use to support clinic strategies for implementing CPS focus for the community. The worksheet provided focused on how community resources could support a CPS focus. Lastly, they were asked what they would add to the original clinic plan that they worked on Day 1 training.
Community training
§Community-Clinic CPS Education and Promotion Action Plan: Panelists join small groups to plan activity for CPS education and promotion.
≠ Planning Assignment: Participants were asked to (1) develop community workshop plan based on an assessment of their intended audience, i.e. co-workers, volunteers, Board of Directors, community partners, residents, etc., (2) complete Audience Assessment and Workshop Planning Worksheet with their organization and partners. They were provided a resource workbook and instructed to see the “Workshop Planning” tab in workbook. (3) prepare a 5-minute presentation on Healthy Aging and clinical preventive services for a specific audience that they will present on Day 2, which was instructed to include: a brief description of the intended audience for your presentation, a definition of healthy aging and CPS guidelines, focus on CPS and specific population relevant to their audience, and discuss why the topic is important to their organization and aging adults they serve.
CPS: clinical preventive services.
Pre-and post-training assessment
To tailor the training, investigators met with CHC leadership to discuss capacity assessment findings and allow CHC leadership to select specific CPS for inclusion. Most CHCs selected colorectal screening as it had the lowest utilization rate and their existing protocols needed improvement. This assessment also revealed limited staff availability to attend trainings, leading us to condense a two-day training curriculum into a three-hour session. As a result, cultural sensitivity training for providers and health care staff, although important, was integrated into existing modules. The training engaged 6-30 staff at each of the five CHCs.
To foster adoption of clinical improvement strategies formulated during the training, investigators met with CHC leadership after the trainings to discuss training evaluation results and offer technical assistance. Most CHCs were at the contemplation stage of adoption of how to apply action steps when the post-training meeting was held.13
NGO capacity building
HAPPI Community Council
Building community capacity to promote and increase CPS utilization required broad partnerships. Over 40 NGOs serving priority populations in the target area were invited to form a HAPPI Community Council. Thirty-four NGOs representing faith-based, community services, housing, worksite/labor, social justice, and volunteer organizations participated in quarterly meetings. The Community Council provided input on the HAPPI community training and small grants program and helped recruit organizations to participate in these activities.
HAPPI Ambassador training of NGOs
Community training goals included: 1) using a train-the-trainer model to develop knowledgeable and skilled communicators -HAPPI Ambassadors- to diffuse CPS knowledge and motivation to community members through local workshops; 2) fostering partnerships with CPS providers and NGOs to improve access to and use of CPS; and 3) sustaining CPS practices.
The HAPPI Ambassador curriculum applied a train-the-trainer model successfully used in previous community capacity building programs14 which draws on NGO’s knowledge of their communities to adapt CPS topics to workshops or other educational sessions they conduct. The curriculum also engaged CHCs that completed the HAPPI in-service training as experts and co-learners to foster sustainable relationships. The design included breakout groups where CHC representatives discussed strategies to advance knowledge and use of CPS with NGO representatives (table II). We conducted the training in English and provided educational materials for community residents in English and Spanish. Participants who completed the training and conducted a community workshop received a 250 dollars stipend and their organizations became eligible to apply for a HAPPI Community Small Grant.
Community small grants program
Eight small grants of 10 000 to 20 000 dollars were awarded through a request for proposal process to organizations employing graduates of the HAPPI Ambassador training. The awards supported culturally-tailored pilot projects that promoted CPS use in partnership with CHCs that had also completed the HAPPI training. The pilot projects applied multiple approaches to increase CPS engagement, delivery, and/or follow-up. While grant funding supported outreach, education, promotion, and referral to at least one CPS, applicants were encouraged to develop projects that combined at least two CPS and to build on the evidence-based models discussed earlier.9
Results
HAPPI increased knowledge of local environments and community resources, and facilitated efforts to increase CPS use by adults 50 years and older in South Los Angeles. The findings highlight the untapped potential to build on existing CHC and NGO capacity and forge CHC-community linkages that promote the health of the aging community through increased use of prevention services.
Community Health Center (CHC) capacity
Baseline CPS utilization rates
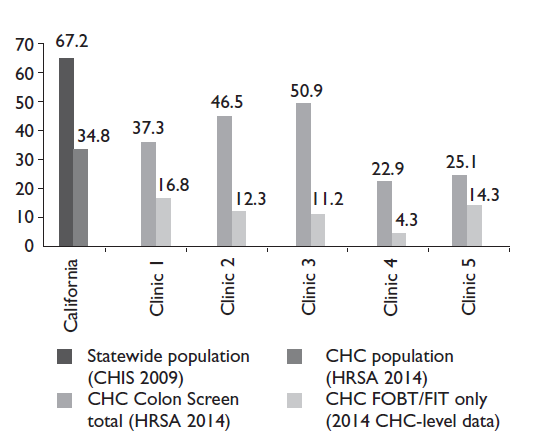
Baseline data gathered from five CHCs in the Southside Coalition on CPS use by individuals 50 years and over documents their 2014 use of the six high-value CPS. According to the California Health Interview Survey, about two-thirds of 50+ Californians reported being adherent with guidelines for any type of colorectal cancer screening6 as compared with only about one-third of people receiving care in one of California’s CHCs (figure 1). During the same period, guideline-compliant colorectal cancer screening rates reported to the federal government across the CHCs participating in HAPPI ranged from 22.9 to 50.9%.15 However, data gathered directly from CHC medical records indicate even lower rates, ranging from 4.3 to 16.8%. CHC key informants suggested possible underreporting due to a lack of reliable documentation and variation in the coding used to extract the CHC data.
CHC key informant interviews
The objective of the CHC assessment was to understand CHCs role in increasing CPS use among the 50+ population. Through key informant (KI) interviews we identified three inter-related barriers to CHCs delivery of CPS to aging adults: 1) CHCs have a history of serving younger populations and are often not prepared for an influx of new, older patients, 2) despite their experience in providing well-child care, their adult services focus on acute care with a reactive versus prevention-oriented paradigm; and, 3) they work in “silos”, independent of surrounding NGOs.
While CHCs serve people of all ages, they have not historically focused on older adults. However, several KIs recognize that older adults are a growing proportion of their service population and acknowledge that serving this “new” group requires organizational culture change. Some attributed the patient shift to the 2010 Affordable Care Act’s (ACA) expansion of health insurance coverage (table III). Interestingly, this created a new environment of competition among CHCs, as previously uninsured patients started using the clinics significantly more once they became insured. The CHCs scaled up to meet the pent-up demand of newly insured patients, including many 50-64 year old’s, who now had more choices. To retain as well as grow their patient population, KI administrators suggested that aging adults represent an “emerging market.”
CHCs serve low-income, high-need communities, and historically funding was for treating episodic health problems rather than disease prevention among adults. Many KIs acknowledged an untapped opportunity to expand the delivery of CPS services to aging adults to prevent disease, disability, and premature death by educating patients and providers.
Table III Healthy Aging Partnerships in Prevention Initiative (HAPPI) study, summary of facilitators and barriers to the use of clinical preventive services (CPS) as identified by community health center (CHC). Key Informants (n=34). South Los Angeles, California, USA, 2014-2015
| Facilitators to CPS in general | Barriers to CPS in general | |
| Community Health Center (CHC) culture | ||
| CHCs provide CPS – this is what they do. CHCs have an opportunity to expand CPS delivery and service to emerging aging/older adult population. | CHCs traditionally served a predominantly younger population – i.e., children, young families, women of reproductive age. Therefore, there has been little push or focus on addressing the specific needs of older adults. | |
| Delivery of CPS | ||
| CHCs periodically engage in special concerted efforts/campaigns to increase specific CPS, especially in response to state or national quality improvement goals. | CHCs have tended to take a more acute (less preventive) approach to the delivery of health care. | |
| Impact of policy changes* | ||
| An increased number of patients have acquired health insurance which, in turn, has created a climate of competition for patients. The passage of health care reform created an opportunity to respond to the pent-up demand for care, for more patients to receive preventive services and referrals to specialists on a more regular basis. | CHCs are experiencing capacity concerns related to workforce turnover: Some clinics are having trouble retaining primary care providers due to the capacity of competing institutions to increase clinician payment and incentives. Also, the scope of change for CHCs in recent years has been dramatic (e.g., Medi-Cal expansion, Medi-Cal managed care, Patient-centered medical home certification). These changes have resulted in competing priorities and have placed many clinics in a reactive rather than proactive mode. | |
| Geriatric training | ||
| CHCs support and advocate for continuing provider education (e.g., clinicians get time off to attend CME courses). However, it is rare for CHCs to have geriatric providers on staff, or training opportunities in geriatrics. | CHCs are experiencing a workforce shortage. Physicians need specialized geriatric training. However, an insufficient number of primary care providers are coming through the pipeline, let alone those with geriatric training. | |
| Facilitators to colorectal cancer screening | Barriers to colorectal cancer screening | |
| Testing | ||
| Yearly testing (e.g., FIT/FOBT) available through the clinic. | Differential testing based on patient’s insurance status (e.g. patients with private insurance able to use colonoscopies as a screening procedure, but public insurance holders only able to use colonoscopies for diagnostic purposes). | |
| Referrals | ||
| Privately insured patients easily receive referrals for more intensive screenings (e.g., sigmoidoscopies, colonoscopies). | Follow-up completion reports and/or results are not easily returned to the CHC that refers patient for a colonoscopy. | |
*Medi-Cal expansion, Medi-Cal managed care, Patient-centered medical home certification, Affordable Care Act (ACA)
Finally, funding mechanisms have incentivized CHCs to operate independent of NGOs and other community resources that provide services and supports to an aging population. When they do partner with NGOs, these partnerships typically rely on special project funding. Efforts to increase the use of specific CPS are typically tied to specific quality improvement goals and are both resource and time-limited.
CHC key informant perspectives on colorectal cancer screening
Colorectal cancer screening is one of the most complicated CPS for CHCs, especially when referring out for additional diagnostic and treatment visits. KIs identified obstacles for patients including mobility, transportation, paperwork, low health literacy, and language barriers for monolingual Spanish speakers. Patients given FOBT/FIT cards often did not return them, and when the FOBT/FIT was positive there were long wait times at the county’s public hospitals for screening and treatment colonoscopies. Once completed, there were challenges to getting results back to the CHCs due to legal regulations intended to protect patient privacy. Facilitators for increasing colorectal cancer screening and other CPS included the capacity of CHCs to conduct the low-cost first screening test (FIT) on-site and the commitment of practitioners who were highly motivated to improve patient health.
Building capacity of CHCs and NGOs
In-service training of CHCs
A total of 164 CHC staff took the training. Those obtaining Los Angeles County CME credit completed the post-training evaluation survey, giving the course a 2.8 average on a three point scale (three-point scale: 3=fully met, 2=somewhat, 1=did not meet) for meeting course objectives. In open-ended questions asked only of physicians, most reported they intended to make practice modifications, such as working with clinic staff to implement system-level changes (e.g., readily available FIT kits; patient coordination for return of specimen; developing EMR documentation process noting supplies were given; develop patients reminder system to return completed test kits). CHCs later reported they planned to collect and analyze data for quality improvement and clinic-wide dissemination. Anticipated barriers included: money, time, habits, and routines. They identified additional staffing needs and the potential to involve multiple staff like medical assistants to educate patients about colorectal screening.
Through follow-up meetings with CHC leadership we learned that the trainings had increased CHCs intent to modify clinical practices and improve CPS service delivery. Two of the five CHCs that focused on colorectal cancer screening reported implementing changes shortly after the training concluded. One CHC revised their FIT colorectal screening kit protocol immediately following the training. Another adapted the Flu-FIT Program, a research tested intervention16 that increases patient access to colorectal cancer screening by offering them home tests at the time of their annual flu shots.17 This CHC added a Flu-FIT education intervention during patient visits for flu shots. Project staff continues to monitor the results of modifications made by participating CHCs.
HAPPI Ambassador training of NGOs
A separate set of trainings were conducted with NGO staff; their satisfaction scores with the HAPPI Ambassador’s train-the-trainer course averaged 4.5/5. Of the 28 out of 32 (88%) who submitted follow-up workshop training plans, 26 workshops were ultimately completed. HAPPI Ambassador’s reached a total of 385 Latino and African American adults with healthy aging and CPS information through community workshops, fulfilling a key objective of the Ambassador role in the project (table IV).
Table IV HAPPI Ambassador Train-the-Trainer (TTT ) workshops. Number of HAPPI Ambassador Trainers who completed TTT workshops and proceeded to independently replicate TTT workshop in their respective organizations (n=32). HAPPI Study, 2016, South Los Angeles, California, USA
| Number of Train-the-Trainer participants | HAPPI Ambassadors who conducted workshops | Workshop participants (end users receiving CPS education) | ||||||
| (n) | (n) | (%) | (n) | |||||
| April 2016 workshop | 13 | 10 | 77 | 153 | ||||
| May 2016 workshop | 19 | 16 | 84 | 232 | ||||
| Total | 32 | 26 | 81 | 385 | ||||
HAPPI small grantees
HAPPI received 20 applications; eight grants were made including five for colorectal screening bundled with another CPS, e.g., combining with cholesterol. Six grantees partnered with participating CHCs, and two well-designed projects without CHC partners received smaller awards.
Conclusion
The World Health Organization (WHO) defines “people-centered care” as care focused and organized around the health needs and expectations of people and communities, rather than on specific diseases. People-centered care encompasses not only individual clinical encounters but also attention to the health of people in their communities and their crucial role in shaping the delivery of health services.18 HAPPI is an ambitious effort to connect CHCs in the underserved area of South Los Angeles with other organizations in the communities they serve to increase delivery of CPS to minority elders. HAPPI aimed to increase the rate of CPS delivery within CHCs and stimulate a deliberate approach to the care of older adults, while simultaneously training and empowering NGOs to increase demand for CPS through person-to-person interactions with community residents, essentially promoting people-centered care.
While HAPPI’s evaluation is ongoing, preliminary findings indicate: 1) a general receptiveness of CHCs to include aging adults as a target population and to improve systems to better provide selected CPS and 2) our method of fostering clinical-community partnerships can be a potentially generalizable approach for other localities throughout the Americas that are facing growing aging populations.
Historically, CHCs both in the United States and in Latin America were established to meet the medical needs of low-income communities, with their growth driven primarily from providing direct medical services to mothers and children. CHCs in our project showed a receptiveness to addressing the “emerging patient population” of aging adults and developing new strategies to improve colorectal cancer screening. The Southside Coalition of Community Health Centers have patient populations between 3.2-5.2% older adults, which is half or less their proportion of the total population; the 50-64 years old group is an additional 16% of community residents.19,20,21,22,23 Similarly, the almost three dozen NGO representatives joining HAPPI efforts and completing a newly designed train-the-trainer curriculum came from many organizations that had not previously conducted programs targeting older adults and/or health promotion. Few had sustained relationships with CHCs.
HAPPIs preliminary results suggest clinics can develop aging-relevant preventive services, which should be applicable in Latin America health care systems facing similar demographic shifts. Although Latin American healthcare systems are qualitatively different from the US, the CHC target population is the poor and underserved and most Latin American countries similarly rely on publically-funded primary care centers to serve low-income and hard to reach populations. CHCs in both the United States and in Latin America are facing the challenge of growing older adult patient populations being served by primary care clinics designed for young families. Raising awareness, redesigning protocols, and connecting clinics with activated community organizations are steps that can improve CPS, and all primary care, for aging adults throughout the Americas.
Next steps in this work include evaluating the impact the HAPPI project had on increasing actual delivery of CPS, creating and sustaining improved CHC workflows for CPS delivery, and maintaining CHC-NGO partnerships working to deliver preventive care for the wider community of older adults.
The United States spends 95% of healthcare dollars in direct medical services, while only 5% on prevention.24 For HAPPI and similar efforts to succeed in promoting prevention at the community level, an equitable distribution of healthcare funding is needed, increasingly directed to successful partnerships between community organizations and direct service providers. Such a committed effort would bring us closer to achieving the WHO goal of accomplishing people-centered care on a broader scale











 nueva página del texto (beta)
nueva página del texto (beta)