Introduction
Lung cancer has been consistently the leading cause of cancer incidence and mortality worldwide over several decades. In 2018, there were over two million new lung cancer cases and 1.7 million deaths, representing 14% of the total number of new cancer cases estimated globally, and 20% of the cancer deaths.1 More than half of the global burden of incidence and mortality occurs in low and middle income countries (LMIC). Prognosis following a lung cancer diagnosis remains poor; even in high-resource settings, with five-year relative survival ranging from 32.9% in Japan to 13.3% in the United Kingdom over the diagnostic period 2010-2014.2
The most important cause of lung cancer is tobacco smoking, with tobacco classified as carcinogenic in humans (Group 1A).3 The geographic pattern worldwide thus depends on the past tobacco smoking histories of the underlying populations, given an average latency period of more than two decades.4 The establishment of the World Health Organization Framework Convention on Tobacco Control (FCTC) and the implementation of its policy package (MPOWER) has contributed to a reduction in smoking prevalence and subsequently in rates of lung cancer and of many other tobacco-related diseases in many countries; nevertheless, with an estimated global population of 1.1 billion people (aged≥15 years) smoking tobacco in 2016, strengthening the implementation of the FCTC in all countries remains a key contributory action to the goal of reducing smoking prevalence by about a third by 2025.5
Comparable incidence statistics at the global level are important metrics for evaluating the lung cancer burden in different populations, revealing distinct patterns that may lead to more targeted tobacco control interventions. We provide here an exposition of the most recent lung cancer incidence and mortality patterns using national estimates for 2018 according to world region from Globocan, as well as observed lung cancer incidence trends using the recorded data in Cancer Incidence in Five Continents (CI5). To aid interpretation, we further examine recent smoking prevalence figures in selected countries.
Materials and methods
Data sources and population
Estimates of lung cancer incidence for 185 countries in the year 2018 were extracted from Globocan database. The methods of national estimation rely upon the most reliable sources of cancer incidence and mortality data of high quality available at national or subnational level. Although population-based cancer registries (PBCR) may be national in terms of coverage, they often cover subnational areas; a detailed account of the methods is provided by Ferlay and colleagues elsewhere.6
We extracted recorded incidence and population data as reported in the latest volume of Cancer Incidence in Five Continents (CI5, Volume XI),7 a compendium of high quality data from PBCR worldwide, for 343 cancer registries in 62 countries worldwide, predominantly for the years of diagnosis 2008-2012. We assumed aggregation of one or more subnational PBCR were nationally representative.* We present the observed lung cancer incidence rates according to a four-tier Human Development Index (HDI) based on the predefined cut-points: low (HDI <0.5); medium (0.5≤HDI<0.8); high (0.8≤HDI<0.9); very high (HDI≥0.9).8
We examined temporal patterns of lung cancer in countries using the longstanding high quality cancer registries that were included in successive volumes of CI5, covering the period from 1980 to 2012.9 To ensure comparability in the incidence between registry populations, morphological groups of the International Classification of Diseases for Oncology (ICD-O, 2000) corresponding to lung, trachea and bronchus cancers (ICD10 C33-34) were selected.
Age-standardized tobacco smoking prevalence among persons aged 15 years and older was extracted from the WHO Global Health Observatory,10 representing the percentage of the population aged 15 years and over who currently use any tobacco product (including smokeless tobacco) on a daily or non-daily basis. More details about the methods to estimate the tobacco prevalence can be obtained in the corresponding WHO global report.11
Statistical analyses
Lung cancer incidence rates per 100 000 person-years were estimated by country, sex and according to four-level HDI. Age-standardized incidence rates (ASR) were adjusted using the world standard population.12 The ASR for the year 2018 and the age-standardized tobacco smoking prevalence among persons 15 years and older (%) in 2015 were plotted using global maps. Time trends of incidence rates are presented for 33 countries by year and sex. Analyses were undertaken using the statistical package R version 3.3.3.
Results
Estimated incidence, mortality and cumulative risk 2018
Table I shows the estimated number of lung cancer cases in 2018 alongside the age-standardized rates (per 100 000) and cumulative risk of incidence and mortality, by world region and sex. Incidence rates varied ten-fold across regions, ranging from 3.4 in Eastern Africa to 49.3 in Eastern Europe. Marked variations were also seen between countries and sub-regions within continents, particularly in Africa (up to a six-fold variation), the Americas and Asia. Among females, rates were consistently lower than those observed in males, ranging from 1.2 in Western Africa to 30.7 in North America. The highest M:F ratios of around 5.0 were seen in Northern Africa and Western Asia, while the lowest M:F ratio of 1.2 were observed in Australia and New Zealand. The mortality rates and the corresponding M:F ratios showed a similar pattern as described for incidence.
Table I Estimated number of lung cancer cases, age-standardized (per 100 000 inhabitants) incidence and mortality rates (ASR) and cumulative risk, worldwide, in males and females, 2018
| Incidence | Mortality | |||||||||||||||||||||||||||
| Male | Female | M:F | Male | Female | M:F | |||||||||||||||||||||||
| Cases | ASR | Cumulative risk | Cases | ASR | Cumulative risk | Cases | ASR | Cumulative risk | Cases | ASR | Cumulative risk | |||||||||||||||||
| World | 1 368 524 | 31.5 | 3.8 | 725 352 | 14.6 | 1.77 | 2.1 | 1 184 947 | 27.1 | 3.19 | 576 060 | 11.2 | 1.32 | 2.4 | ||||||||||||||
| Africa | ||||||||||||||||||||||||||||
| Eastern Africa | 3 296 | 3.4 | 0.4 | 2 595 | 2.2 | 0.2 | 1.5 | 3 230 | 3.4 | 0.4 | 2 503 | 2.2 | 0.26 | 1.5 | ||||||||||||||
| Middle Africa | 1 285 | 3.8 | 0.4 | 975 | 2.3 | 0.2 | 1.7 | 1 240 | 3.6 | 0.4 | 911 | 2.2 | 0.26 | 1.6 | ||||||||||||||
| Northern Africa | 16 008 | 16.9 | 2.1 | 3 529 | 3.4 | 0.4 | 5.0 | 15 655 | 16.6 | 2.02 | 3 183 | 3.1 | 0.36 | 5.4 | ||||||||||||||
| Southern Africa | 5 634 | 26.0 | 3.0 | 2 782 | 8.9 | 1.0 | 2.9 | 5 348 | 25.0 | 2.92 | 2 597 | 8.3 | 0.96 | 3.0 | ||||||||||||||
| Western Africa | 2 087 | 2.4 | 0.2 | 1 162 | 1.2 | 0.1 | 2.0 | 2 058 | 2.4 | 0.26 | 1 023 | 1.1 | 0.12 | 2.2 | ||||||||||||||
| America and Caribbean | ||||||||||||||||||||||||||||
| Caribbean | 6 540 | 23.5 | 2.8 | 4 466 | 14.2 | 1.7 | 1.7 | 5 866 | 20.8 | 2.49 | 3 609 | 11.2 | 1.36 | 1.9 | ||||||||||||||
| Central America | 5 962 | 7.2 | 0.8 | 4 300 | 4.5 | 0.5 | 1.6 | 5 368 | 6.4 | 0.74 | 3 619 | 3.7 | 0.43 | 1.7 | ||||||||||||||
| South America | 39 255 | 16.8 | 1.9 | 29 249 | 10.2 | 1.2 | 1.6 | 36 824 | 15.7 | 1.86 | 26 098 | 9.0 | 1.08 | 1.7 | ||||||||||||||
| Northern America | 133 950 | 39.1 | 4.7 | 118 796 | 30.7 | 3.8 | 1.3 | 91 957 | 25.8 | 3.02 | 81 321 | 19.4 | 2.29 | 1.3 | ||||||||||||||
| Asia | ||||||||||||||||||||||||||||
| Eastern Asia | 633 284 | 47.2 | 5.6 | 316 731 | 21.9 | 2.6 | 2.2 | 557 985 | 41.1 | 4.74 | 257 650 | 17.1 | 1.99 | 2.4 | ||||||||||||||
| South-Eastern Asia | 78 453 | 26.3 | 3.0 | 34 729 | 9.6 | 1.1 | 2.7 | 70 504 | 23.8 | 2.82 | 30 227 | 8.4 | 0.98 | 2.8 | ||||||||||||||
| South Central Asia | 80 415 | 9.4 | 1.1 | 30 627 | 3.4 | 0.4 | 2.8 | 74 991 | 8.8 | 1.06 | 28 871 | 3.2 | 0.38 | 2.7 | ||||||||||||||
| Western Asia | 41 309 | 38.8 | 4.7 | 9 481 | 7.8 | 0.9 | 5.0 | 39 773 | 37.6 | 4.64 | 8 861 | 7.3 | 0.85 | 5.2 | ||||||||||||||
| Europe | ||||||||||||||||||||||||||||
| Eastern Europe | 109 928 | 49.3 | 6.2 | 39 155 | 11.9 | 1.5 | 4.1 | 99 266 | 44.2 | 5.67 | 32 093 | 9.4 | 1.2 | 4.7 | ||||||||||||||
| Northern Europe | 39 265 | 34.0 | 4.0 | 35 106 | 26.9 | 3.3 | 1.3 | 30 144 | 25.1 | 2.88 | 25 571 | 18.1 | 2.18 | 1.4 | ||||||||||||||
| Southern Europe | 72 411 | 43.1 | 5.3 | 28 518 | 15.7 | 1.9 | 2.7 | 63 933 | 36.1 | 4.36 | 22 700 | 11.5 | 1.39 | 3.1 | ||||||||||||||
| Western Europe | 90 239 | 43.3 | 5.3 | 55 417 | 25.7 | 3.2 | 1.7 | 74 003 | 33.5 | 4.04 | 40 233 | 17.0 | 2.11 | 2.0 | ||||||||||||||
| Oceania | ||||||||||||||||||||||||||||
| Australia/New Zealand | 8 345 | 28.4 | 3.2 | 7 239 | 24.0 | 2.96 | 1.2 | 6 026 | 20.0 | 2.3 | 4 547 | 14.3 | 1.73 | 1.4 | ||||||||||||||
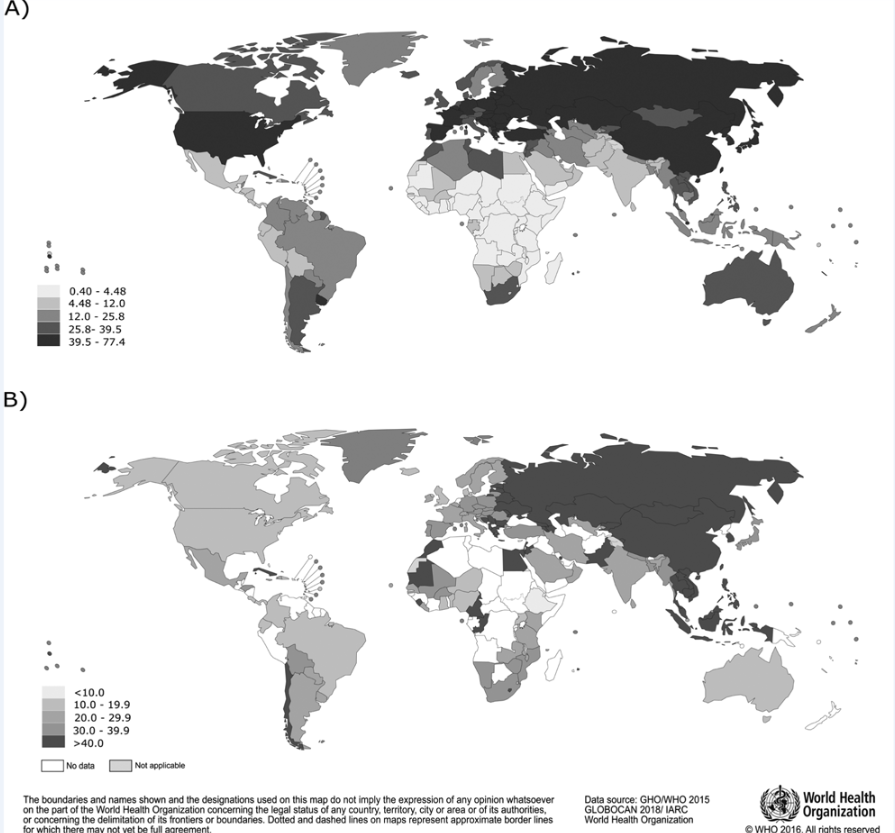
Figures 1 A and 2A depict the national lung cancer incidence variations in males and females, respectively. The highest incidence rates were observed in Northern and Western European countries, in both sexes, while incidence rates were low in African countries. In the Americas, elevated incidence rates were observed in Uruguay and Cuba.
Tobacco prevalence in 2015
Figures 1B and 2B show the observed variations in national (age-standardized) smoking prevalence (%) among persons 15 years and older in 2015, for males and females, respectively. The global mean tobacco smoking prevalence in 2015 was 34% in males and 10.9% in females (data not shown). Among males a higher prevalence was observed in Western Europe (mean prevalence of 42.1%) and Asia (41.7%), while for females, the prevalence tended to be lower but was elevated in Western Europe (24.9%), Southern Europe (24.2%) and Northern Europe (20.4%). In Central and South America, smoking prevalence was low relative to the global average, with prevalence proportions of 24.9% among males and 10.9% in females, respectively; Cuba and Chile had the highest prevalence in the region, of 52.7 and 40.0%, respectively (data not shown).
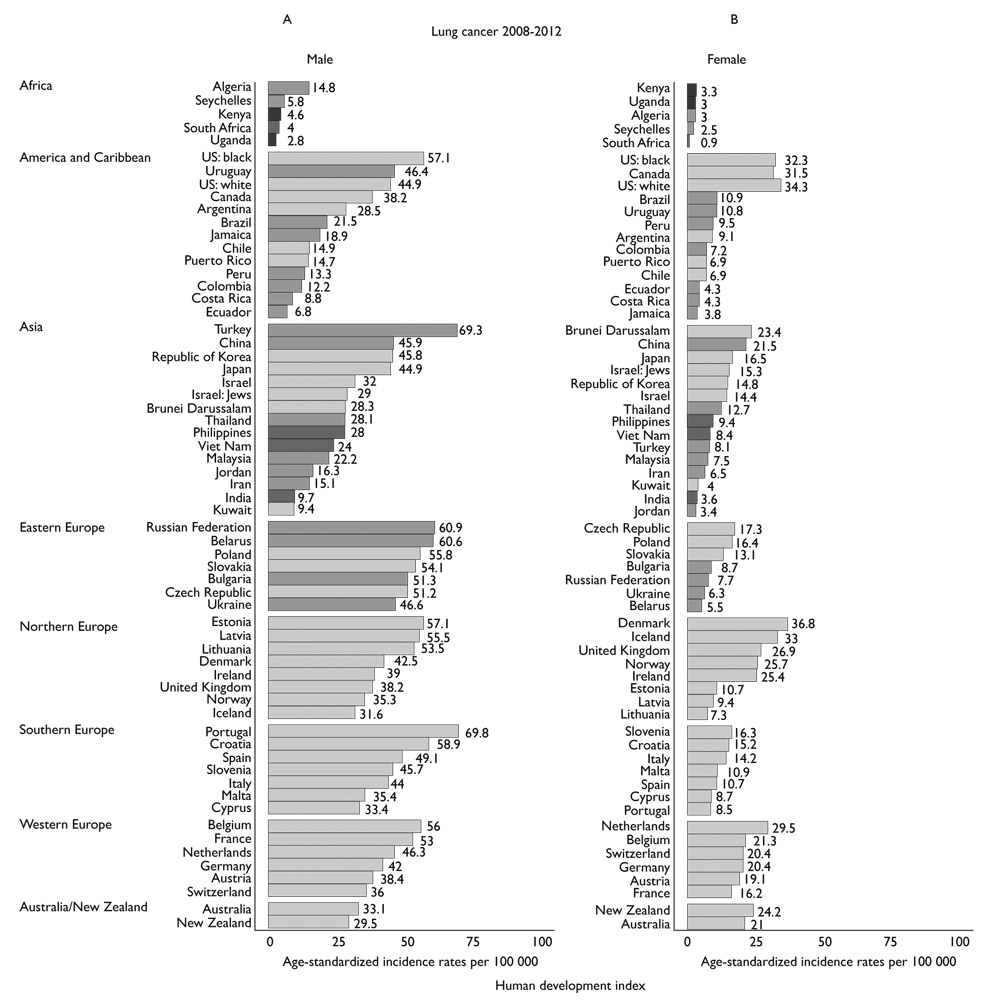
Observed incidence circa 2008-2012
Lung cancer ASR circa 2008-2012 are presented by sex and region in figure 3. Overall, they varied markedly: among males, the highest incidence rates were observed in Portugal (ASR of 69.8), Turkey (69.3) and among US blacks (57.1), while in females, rates were highest in Denmark (36.8), and the Netherlands (29.5). The rates in Eastern European countries tended to be less variable in men, ranging from 46.6 in Ukraine to 60.9 in the Russian Federation. In Asia, male incidence rates were quite similar in China, Republic of Korea and Japan (ASR of 45.9, 45.8 and 44.9, respectively), while in the Americas and the Caribbean, elevated incidence rates among males were found in Uruguay (46.4) and the US (46.3). Generally, higher incidence rates were observed in countries classified as very high-income countries.
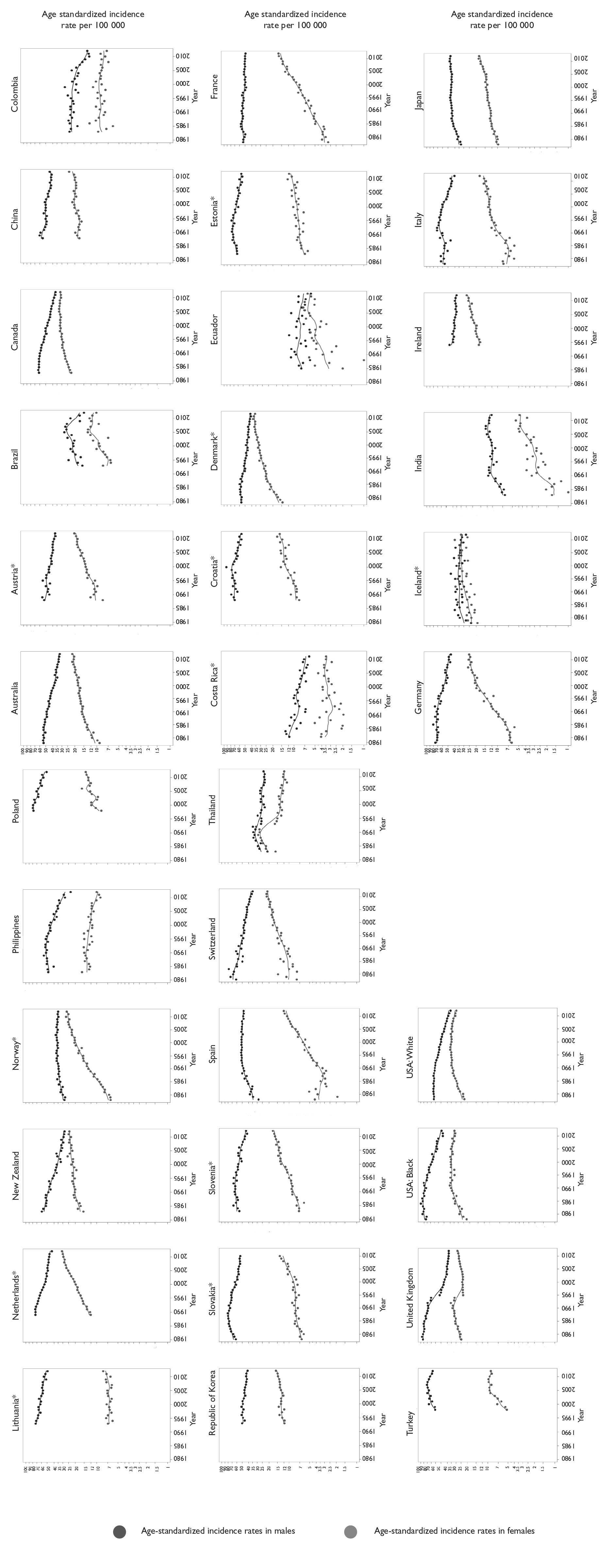
Temporal patterns 1980-2012
The trends in lung cancer incidence rates in selected countries 1980-2012 are plotted in figure 4. The majority of the countries exhibited stable or decreasing incidence rates among males, but increasing rates among females. In South America and the Caribbean, incidence rates increased among females in Ecuador and Brazil, while in Colombia and Costa Rica, rates were stable or in recent decline. North America and Oceania conveyed similar patterns, with decreasing rates in males and female rates either increasing or stabilizing. In Asia, incidence rates in Thailand and Philippines decreased over the study period in both males and females; while, in contrast, rising rates were seen in Japan, Republic of Korea and India in women. Among most Western European countries (Austria, Denmark, France, Germany, Switzerland and Netherlands), incidence rates among males were either flat or in decline, although female rates were increasing. A not dissimilar pattern was observed in Eastern Europe, particularly in Poland and Slovakia, and in Northern Europe, including Denmark.
Discussion
We present here the most recent estimates of lung cancer incidence and mortality worldwide, in 185 countries alongside recorded incidence data in 62 countries coupled with recent figures on tobacco smoking prevalence (%) among males and females 15 years and older. Overall, with two new million cases each year, lung cancer still represents the most important cancer worldwide, with an elevated incidence and mortality burden among males, relative to females. We observed significant variations in rates between and within regions worldwide, with Europe, Asia and North America observed to have the highest incidence rates worldwide, and sub-Saharan Africa, the lowest. Where temporal data were available, the lung cancer incidence trends varied considerably in their direction and magnitude; the most common pattern found among men was stable or decreasing trends, while increasing trends were predominant among women.
Current geographic patterns in lung cancer incidence mainly reflect recent and past exposure to tobacco. Tobacco smoking (both active and passive) is the main risk factor for lung cancer. The tobacco epidemic began among men at the beginning of the 19th century in several high income countries, and developed in women one or more decades later.13 In our results, geographic variation in lung cancer between and within regions appears to correlate with current tobacco prevalence. Although recent incidence rates reflect the duration and intensity of tobacco smoking more accurately than 20 years ago.
Overall the current prevalence of tobacco use in the Americas is lower relative to Europe. In South America, the higher lung cancer incidence rates observed in Uruguay and Argentina, are consistent with the higher tobacco prevalence in both countries, as reported previously.14,15 In the US, the declining rates in both sexes, first observed in males in the 1990s and in females in the 2000s is driven by the decreasing tobacco prevalence reported by Thun and colleagues,13 with an approximate 20 year lag between the peaks of smoking prevalence and lung cancer mortality rates. In Central and South America, the tobacco epidemic was initiated years later; Costa Rica and Colombia have seen decreasing incidence rates by 2000 and 1990 respectively, while rates in Ecuador have stabilized in men.
The burden of lung cancer in Asia is of particular concern. In many Asian countries, the prevalence of tobacco is high (at least relative to the US), although some declines in incidence rates have been observed from the mid-1980s in China (Harbin, Jiashan, Shangai, and Zhongshan), and the Philippines. Our results indicate a 10-fold difference between Asian countries, with the highest incidence observed in Turkey, China, the Republic of Korea and Japan. Although the prevalence of tobacco use among women in China and Republic of Korea tends to be considerably lower than in the US (less than 5% in 2015 in China and Republic of Korea versus 15% in the US), recent incidence rates were higher in Asia than in several European countries. This fact may be related to higher levels of indoor and outdoor pollution, an important risk factor for lung cancer in non-smokers.16 In Japan, we observed a plateau in incidence rates at the end of the 1980s, with a stabilization and slight decline by the early-1990s. As Japanese males started their smoking careers later than Northern American males,17 lung cancer incidence rates are presently lower, despite a higher prevalence of tobacco smoking. A declining prevalence of tobacco has been observed in the Japanese population in the 2000s (data not shown), with a slight increase in rates observed in females and a plateau in males.
The lung cancer epidemic has had an enormous impact on public health in European countries.18 As an example, the incidence rates in Portugal are the highest of the continent in men and 10-fold higher than in women, with further increases expected in women. Elsewhere the grounds for optimism, given declining incidence rates among men in Italy, United Kingdom, Denmark and Netherland, are countered in most European countries by the more recent tobacco epidemic in women, that is contributing to the rising incidence in this group, in both younger and older generations.18 Assessing these in the context of recent tobacco trends, the prevalence of current smoking in France for example, historically high in men, has declined progressively up until 2000 and remained relatively stable thereafter, while in women it has uniformly increased over the same period.19 Somewhat more encouraging are the declines in tobacco prevalence observed in women reported in several countries, suggesting that lung cancer rates will reach a plateau in future years and decline thereafter. Reliable tobacco prevalence data using comparable surveys is needed to assess this, and over the last decade substantial progress has been made in implementing the FCTC at the national level to enable best-practice policies that are adopted to protect millions of lives.
Robust national tobacco control policies are critical in curbing the global tobacco epidemic. In 2013, the WHO Global Action Plan for the prevention and control of noncommunicable diseases (NCDs) 2013-2020 called for governments to reduce the current burden of tobacco by about one-third by 2025, posing challenges to the assessment of long-term prevalence and implementation of MPOWER measures. MPOWER measures were established in 2008 to ensure cost-effective interventions that can lead to marked reductions in tobacco use.20 In addition, monitoring tobacco use and prevention policies using standard methodology are being made possible through global surveys, including the Global Adult Tobacco Survey (GATS) and the Global Youth Tobacco Survey (GYTS). These have shown the inverse relationship between tobacco price and prevalence;21 raising taxes on tobacco is one of the most effective policies to reduce tobacco consumption.22 Increasing the price of tobacco through tax hikes discourage the young to commence smoking and supports the cessation in smokers; there is no safe level of tobacco consumption and the promotion of a smoke-free environment is an effective way to protect people, in particular from exposure to second-hand smoke.
The interpretation of the global pattern of lung cancer requires considerable caution, given its broad and complex relation with past tobacco consumption. It is also important to note that incidence data are derived from subnational cancer registries in some countries and they may not completely represent the national scale and profile. In addition, Thailand and United Kingdom present an artefact in rates around the 1990s, probable driven by changes in coding practices during the period.
In summary, this study has sought to report the most recent global figures on lung cancer based on high quality population-based cancer registries and tobacco prevalence data at the global, regional and national levels. We highlight the marked disparities in incidence between and within regions; the higher lung cancer incidence rates in parts of South America and Asia are important markers of the current tobacco epidemic and warrant further study to better understand the role of tobacco control prevention. Efforts should be made to improve the quality and the availability of tobacco prevalence information over time to permit more informative research based on international comparable statistics. The continuing rise in lung cancer among women in many countries further reinforces the need for the targeted implementation of smoking cessation policies to curb the tobacco epidemic and save millions of lives.











 nueva página del texto (beta)
nueva página del texto (beta)