Introduction
Worldwide, human papillomavirus (HPV) is the most frequent sexually transmitted infection, and genital warts (GW) are caused by infection with low oncogenic types HPV6 or HPV11.1,2,3 In some countries, GW are considered an important health issue,4,5,6,7,8,9,10,11 although data are scarce in regions such as Latin America and the Caribbean.3,12,13 Efforts have been made to document the burden of GW in Mexico but certain factors, such as patterns of infection, type of medical specialists who treat GW, impact on the population, and the financial burden, remain unknown.
GW are not consistently reported for several reasons that include stigma related to the disease and delayed diagnosis due to hesitation in seeking medical care. Additionally, GW include a wide spectrum of lesions, some of which may be undiagnosed. Global comparisons of the burden of GW are also difficult because different countries present their GW data using varying methodologies including age range at diagnosis. This has led to a wide variability in reporting the incidence of GW globally. The United Kingdom has one of the most comprehensive reporting practices due to their systematic registration of sexually transmitted diseases since 1971.14,15,16
A systematic review of the incidence of GW based on 13 studies from North and South America, Europe and Australia, includes information obtained from administrative databases, medical chart reviews, prospectively collected specialist reports, and genital examination of patients. The overall median incidence reported was 1.57 per 1 000 person-years and a prevalence ranging from 0.15 to 0.18%.17
HPV vaccine efficacy trials, which included 16-24 year old women from Mexico, Colombia, Costa Rica and Guatemala, reported a GW incidence of 8 per 1 000 person-years and a prevalence of 1.9% in the placebo arm, along with a 3.6% prevalence of HPV6 and a prevalence of 0.8% of HPV11 at enrollment.18 The HPV in Men (HIM) study, which included 18-70 year old men in Mexico, the United States, and Brazil reported an HPV incidence rate of 2.35 per 1 000 persons-years.19
Unlike GW incidence data, information about GW treatment is more standardized globally, with treatments generally classified into self-applied therapies (podophyllin, imiquimod) and clinic-based therapies (cryotherapy, trichloroacetic acid and surgical excision).20 In Australia, for example, imiquimod and podophyllin are prescribed at nearly-similar rates, and approximately 26% of medical consults are with women vs 22% with men. This same study reports that ablative treatments are significantly more common among men than in women (60 vs. 37%, respectively).21 GW are often resistant to treatment and present a high recurrence rate, which may result in the need for several consultations and different procedures to treat a single patient.
Multiple clinical visits and procedures to treat GW generate direct and indirect medical costs and indirect costs due to loss of productivity of the patient. Several studies have described the costs accrued during a GW episode, from the time of occurrence to the end of treatment.22,23 A systematic review conducted by Raymakers and colleagues reports a wide variation in treatment costs ranging from $167 USD in England to $ 1 196 USD in Spain.22,23
The development of the quadrivalent HPV vaccine and the more recent nonavalent HPV vaccine, which both target HPV genotypes 6 and 11, have generated relevant research regarding HPV and GW. However, the burden of GW remains understudied in many countries, including Mexico. Additionally, only a few studies with small sample sizes have evaluated the impact of GW on quality of life (QoL). The broad heterogeneity of the instruments used to evaluate QoL make it difficult to determine the true psychological burden of GW.24
There have been numerous HPV-related epidemiological studies in Mexico, but research regarding the burden of and types of treatments for GW is scarce. Although GW are not life-threatening, they are relatively common, have a significant impact on QoL, and result in an intensive use of health services. Thus, the burden of GW needs to be better characterized. The aim of this study was to estimate the burden of GW in Mexico by surveying specialists who regularly treat GW, and assessing the QoL of patients with GW.
Materials and methods
We examined national data reported by health care professionals who care for patients with GW to estimate the health care burden of GW in Mexico. A provider-based survey was used to assess the number of GW cases observed at various colposcopy, urology, and dermatology services from November 2011 to April 2013. We also obtained information regarding the treatment practices among specialists who offer medical care for GW on a regular basis. First, we contacted the presidents of the medical associations of colposcopy, urology and dermatology services in Mexico, to obtain the necessary permissions to conduct this study. We also promoted our study during special presentations at the health care professionals’ monthly meetings. Based on the Medical Societies and Colleges in Mexico, there are an estimated 3 300 colposcopists, urologists, and dermatologists, of which 417 participated in our study. Our recruitment strategy and study design are presented in figure 1.
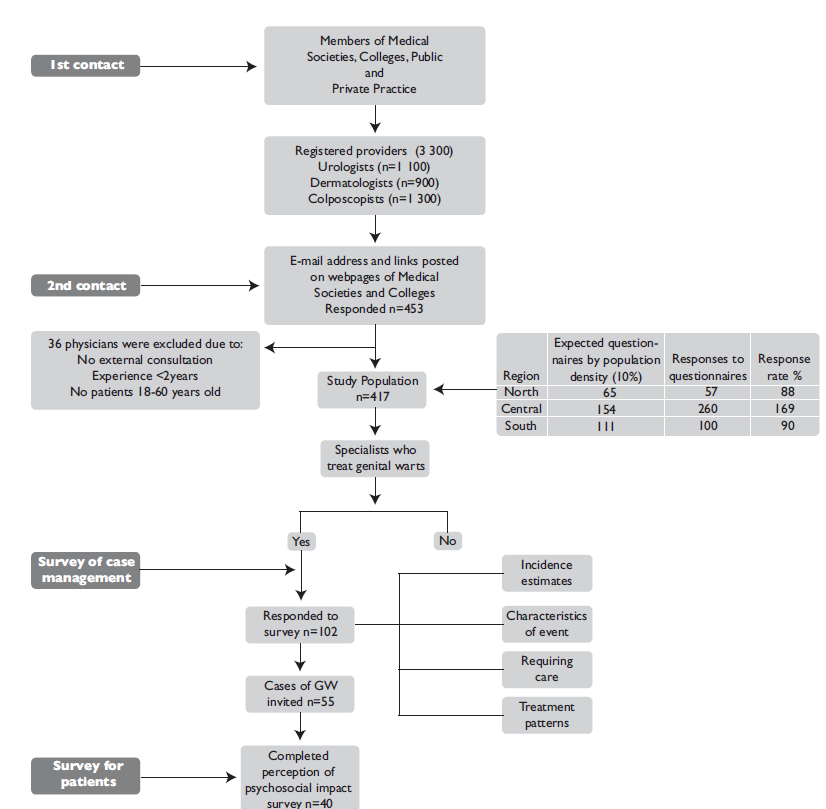
GW: genital wards
North: Baja California, Baja California Sur, Sonora, Coahuila, Chihuahua, Durango, Nuevo León, Tamaulipas
Central: Aguascalientes, Colima, Ciudad de México, Guanajuato, Jalisco, Estado de México, Michoacán, Nayarit, Querétaro, San Luis Potosí, Sinaloa, Zacatecas
South: Campeche, Chiapas, Guerrero, Hidalgo, Morelos, Oaxaca, Puebla, Quintana Roo, Tabasco, Tlaxcala, Veracruz, Yucatán.
Figure 1 Population Study Selection Flow Diagram
A primary survey was used to obtain demographic characteristics and clinical practice information from all participants. This survey was mainly administered through a web-based platform, and providers who required assistance were helped by phone or completed a paper-based version. The survey was anonymous and strictly confidential. Specialists who completed the primary survey and reported that they treat patients with GW using standard procedures were asked to participate in a second survey. The additional survey collected information about the number of GW cases observed during a typical week, including the estimated number of new cases, and the types of procedures used to treat GW.
To evaluate the psychosocial burden of GW among patients, we used the HPV Impact Profile (HIP) questionnaire, which uses a linear 0-100 point scale, with higher values indicating better conditions.25 We also applied the CECA instrument (Spanish acronym for the Specific Questionnaire for Condylomata Acuminata), a valid and reliable self-administered questionnaire that measures health-related quality of life (HRQL) in patients with GW.26 This instrument assesses emotional well-being and sexual activity, with higher scores corresponding to a better QoL.
The provider and patient survey responses were entered into a database. The data were used to estimate the total number of GW cases per week and per year for each specialist, and to estimate of annual total GW cases, and estimate the total cost of GW case-management. Some data were excluded from analysis, including data from specialists who did not see patients with GW, specialists with less than 2 years of experience, and specialists who only saw patients under 18 years or over 60 years of age.
The costs to treat GW were estimated for the three types of specialists, and are reported in USD. To convert Mexican pesos to USD we used the average exchange rate of $18.13 pesos per USD reported by the National Bank of Mexico in 2017. All data analyses were conducted using the STATA statistical software package version 12.0* and Microsoft Excel (2013). The study protocol, questionnaires, procedures, and informed consent forms were approved by the Ethical Committee of the National Institute of Public Health (CI:985, No. 1036).
Results
Specialist characteristics
We collected demographic and clinical practice data from 417 specialists (12.6% of the total specialists registered in the Medical Societies and Colleges in Mexico) using the primary survey. Most of the specialists were colposcopists (n=227), followed by urologists (n=158) and dermatologists (n=32), and 62.4% were from the Central region of Mexico (table I). A subset of 102 specialists (24.5%) also completed the secondary survey and provided information regarding the number of their patients with GW, resource utilization, and treatment practices. The provider response rate was adequate based on population distribution estimates, assuming that providers are proportionally distributed by population size and region. As table I indicates, 64% of the respondents are male, with an average age of 46.3 years for all respondents (range 24 to 75 years). Notably, 84.9% of the sample reported practicing in an urban area, including 93.8% of dermatologists and 78.9% of colposcopists. Nearly half of respondents (47%) stated that their primary practice is at a private, Institution, and one-third indicated that their secondary practice was at a public hospital.
Table I Characteristics of the specialists who treat patients with genital warts
|
Total n=417 n (%) |
Colposcopy n=227 n (%) |
Urology n=158 n (%) |
Dermatology n=32 n (%) |
|||||
|
Sex* |
||||||||
|
Males |
267 (64.0) |
104 (45.8) |
147 (93.0) |
16 (50.0) |
||||
|
Females |
131 (31.4) |
115 (50.7) |
2 (1.3) |
14 (43.8) |
||||
|
Age, mean (SD) |
46.3 (11.1) |
47.8 (9.7) |
42.5 (12.2) |
52.0 (11.7) |
||||
|
Years in practice, |
||||||||
|
Mean (SD) |
16.0 (10.3) |
16.7 (9.1) |
13.5(10.9) |
22.0 (11.9) |
||||
|
Region‡ |
||||||||
|
North |
57 (13.7) |
29 (12.8) |
25 (15.8) |
3 (9.4) |
||||
|
Central |
260 (62.4) |
125 (55.1) |
110 (69.6) |
25 (78.1) |
||||
|
South |
100 (24.0) |
73 (32.2) |
23 (14.6) |
4 (12.5) |
||||
|
Working Area* |
||||||||
|
Urban |
354 (84.9) |
179 (78.9) |
145 (91.8) |
30 (93.8) |
||||
|
Suburban |
42 (10.1) |
37 (16.3) |
4 (2.5) |
1 (3.1) |
||||
|
Rural |
4 (1.0) |
4 (1.8) |
0 (0.0) |
0 (0.0) |
||||
|
Primary work location§ |
||||||||
|
Private practice clinic |
196 (47.0) |
126 (55.5) |
58 (36.7) |
12 (37.5) |
||||
|
Private hospital |
50 (12.0) |
27 (11.9) |
21 (13.3) |
2 (6.3) |
||||
|
Public hospital |
186 (44.6) |
98 (43.2) |
69 (43.7) |
19 (59.4) |
||||
|
Other# |
16 (3.8) |
15 (6.6) |
0 (0.0) |
1 (3.1) |
||||
|
Patients per week& |
||||||||
|
Total, mean (SD) |
39.1 (33.8) |
38.7 (30.5) |
28.1 (16.1) |
66.1 (42.1) |
||||
|
Males, mean (SD) |
7.6 (14.4) |
- |
19.6 (10.8) |
26.4 (17.9) |
||||
|
Females, Mean (SD) |
31.9 (30.8) |
38.7 (30.5) |
8.4 (7.3) |
39.7 (28.2) |
||||
* Do not sum 100% by missing values
‡ North: Baja California, Baja California Sur, Sonora, Coahuila, Chihuahua, Durango, Nuevo León, Tamaulipas; Central: Aguascalientes, Colima, Ciudad de México, Guanajuato, Jalisco, Estado de México, Michoacán, Nayarit, Querétaro, San Luis Potosí, Sinaloa, Zacatecas; South: Campeche, Chiapas, Guerrero, Hidalgo, Morelos, Oaxaca, Puebla, Quintana Roo, Tabasco, Tlaxcala, Veracruz, Yucatán
§ Sum more than 100% because the specialists selected more than one option
# Other Services Mentioned: Clinical Lab, Sexual Health Services of a NGO (Non-Governmental Organization)
& Total of patients attended by any reason
Incidence and prevalence estimates
All three specialists reported that most of the patients with GW they see are “drop-ins/not referred”. The next most common referral option for GW patients was from primary care specialists. When asked what specific types of providers regularly refer patients with GW, the primary care specialists were consistently selected. The highest frequency of referrals was from colposcopists, urologists and dermatologists (table II). Based on their estimates we calculated that 11 400 new cases of GW are diagnosed each week.
Table II Incidence and prevalence of genital warts (GW) in Mexico
|
Specialist |
N |
Total patients cared per week‡ |
Patients with GW per week‡ |
New patients with GW per week‡ |
||||||||||
|
Males |
Females |
Males |
Females |
Males |
Females |
|||||||||
|
Colposcopists |
1300 |
- |
30 |
- |
4 |
- |
2 |
|||||||
|
- |
39 000 |
- |
5 200 |
- |
2 600 |
|||||||||
|
Urologists |
1100 |
18 |
6 |
3 |
1 |
2.5 |
1 |
|||||||
|
19 800 |
6 600 |
3 300 |
1 100 |
2 750 |
1 100 |
|||||||||
|
Dermatologists |
900 |
24.5 |
35.5 |
3 |
3 |
3.5 |
2 |
|||||||
|
22 050 |
31 950 |
2 700 |
2 700 |
3 150 |
1 800 |
|||||||||
|
Total specialist* |
3300 |
41 850 |
77 550 |
6 000 |
9 000 |
5 900 |
5 500 |
|||||||
|
New patients estimated per year§ |
2 008 800 |
3 722 400 |
288 000 |
432 000 |
283 200 |
264 000 |
||||||||
* Total specialists registered with a specialty medical association in Mexico
‡ Median of patients
§ Considering 48 working weeks in a year
Total weeks worked per year (48 weeks)
Treatment practices
According to information reported by dermatologists and urologists, the most common diagnostic procedure to identify GW in males is visual examination with or without acetic acid (61.6% and 51.4%, respectively). The most frequent diagnostic method among females is visual examination with acetic acid (72.7%). Dermatologists report using visual examination with or without acetic acid, the Papanicolaou test, and colposcopy in equal proportions to detect GW in females (table III). The median number of visits required to manage GW from diagnosis until treatment is complete are four median visits for colposcopists and dermatologists, and three visits for urologists (table III).
Table III Resource utilization for diagnosis and treatment of episodes of genital warts, November 2011 to April 2013, Mexico
|
Characteristic |
Colposcopy n=44 |
Urology n=42 |
Dermatology n=16 |
|||||||
|
Females |
Males |
Females |
Males |
Females |
||||||
|
Time elapsed until medical care, median days (p25, p75) |
28 (7,49) |
28 (14,49) |
17.5 (10.5,56) |
28 (28,56) |
24.5 (14,28) |
|||||
|
Diagnostic methods, % of patients applied |
||||||||||
|
Visual exam/acetic acid test |
67.1 |
61.6 |
15.3 |
51.4 |
33.4 |
|||||
|
Anoscopy /proctoscopy |
22.4 |
15.7 |
1.3 |
4.4 |
0.0 |
|||||
|
Histologic exam/biopsy |
46.7 |
23.2 |
3.3 |
2.8 |
10.4 |
|||||
|
Cytology/Papanicolaou |
33.1 |
- |
5.6 |
- |
33.1 |
|||||
|
Colposcopy |
72.7 |
- |
4.4 |
- |
33.6 |
|||||
|
Hybrid capture II/PCR |
16.8 |
15.8 |
0.6 |
1.9 |
0.0 |
|||||
|
Urethroscopy /Meatoscopy |
10.2 |
27.6 |
0.0 |
11.7 |
0.0 |
|||||
|
Other diagnostic method* |
1.7 |
47.5 |
0.0 |
20 |
0.0 |
|||||
|
Duration of treatment, median days (p25, p75) |
28 (7,56) |
6 (1,7) |
14 (7,42) |
56 (28,140) |
56 (28,84) |
|||||
|
Duration of treatment, median visits (p25, p75) |
4 (3, 6) |
3.5 (3,6) |
3 (3,4) |
4 (3,6) |
4 (3,7) |
|||||
* Other techniques mentioned: androscopy /penoscopy/dermatoscopy
PCR: Polymerase chain reaction
The specialists who participated in this study reported the different treatment procedures used for the last 20 patients they saw in their practice. Electrosurgery was used 42.4% of the time, followed by cryotherapy (17.2%), which was used by dermatologists an average of 3.33 times per patient. Trichloroacetic acid was used by colposcopists an estimated 3.42 times per patient. Podophyllin resin was the most common topical agent used to treat males, while imiquimod was the most common agent used for females. Finally, urologists reported use of various other treatments, which mostly include topical agents such as imiquimod, with an average of 32 applications of this treatment per episode per patient (data not shown).
Cost estimates
The estimated cost to treat a single GW episode in our study was estimated to be $342.06 USD ($290.27-$435.25 USD) (table IV). These costs varied depending on the sex of the patients and by different specialists, with a larger number of visits for men. The estimated annual cost to treat GW was $ 194.58 million USD (table IV).
Table IV Costs of treating genital warts by type of specialist in Mexico*
|
Treatment |
Unitary cost $ |
Colposcopists |
Urology |
Dermatology |
||||||||||
|
# of sesions needed‡ |
Cost $ |
# of sesions needed‡ |
Cost $ |
# of sesions needed‡ |
Cost $ |
|||||||||
|
Costs of treatment |
||||||||||||||
|
Consultation |
33.37 |
3 |
100.10 |
2.4 |
80.08 |
2.8 |
93.43 |
|||||||
|
Crioterapy |
66.73 |
0.25 |
16.68 |
0.75 |
50.05 |
1.3 |
86.75 |
|||||||
|
Electrosurgery |
100.10 |
0.8 |
80.08 |
1 |
100.10 |
1 |
100.10 |
|||||||
|
Curettage |
66.73 |
0.5 |
33.37 |
0.2 |
13.35 |
1 |
66.73 |
|||||||
|
Tricoloroacetic Acid |
33.37 |
0.9 |
30.03 |
1 |
33.37 |
0.5 |
16.68 |
|||||||
|
Aldara 5% cream |
6.44 |
6 |
38.63 |
2 |
12.88 |
8 |
51.51 |
|||||||
|
Wartec cream 0.15% |
4.45 |
0.4 |
1.78 |
0.1 |
0.45 |
4.5 |
20.05 |
|||||||
|
Total cost per treatment |
300.67 |
290.27 |
435.25 |
|||||||||||
|
Proyetions of annual costs of treatment | ||||||||||||||
|
# Pacients estimated per week |
2 |
3.50 |
5.50 |
|||||||||||
|
Total specialists across country |
1 300 |
1 100 |
900 |
|||||||||||
|
Total of new pacients treated per week |
124 800 |
184 800 |
237 600 |
|||||||||||
|
Total costs per specialists in millions $ |
37.52 |
53.64 |
103.42 |
|||||||||||
|
Total costs in USD millions $ |
194.58 |
|||||||||||||
* In US dollars reported by the National Bank of Mexico (Banxico), June 2017
‡ Median of the number that specialists reported using each specific procedure per episode of genital warts
Patient characteristics and psychosocial burden
Seventy patients with GW were asked to report how their QoL is impacted by GW, and 55 of them agreed to participate in our study. A total of 40 patients completed the survey, for a response rate of 57%. The average age of patients was 32.8 years (range 18 to 69 years), 50% of the sample was female, and most patients were from urban areas in Central Mexico. The majority of participants identified as heterosexual (70%); and of the remaining participants (30%), 88.9% of males and 11.1% of females identified as homosexual. The average age at sexually debut was 17 (16.3-18.5) years. Approximately 15% responded that they “always” use condoms, regardless of type of sexual activity. Nearly all participants (94%) consulted a specialist during their most recent outbreak of GW, and approximately 60% made an appointment to see a specialist in less than five weeks. Dermatologists and internists were the most commonly consulted specialists. More than 66% of patients had a GW episode that lasted nine weeks or more, and 20% of males reported that they experienced recurring GW.
The psychosocial burden assessed using the HIP survey yielded an average score of 39.9, with males indicating a slightly worse perception of psychosocial impact than females. The average CECA score was 51.9 with a similar impact in the emotional and sexual areas (47.6) (table V). We were unable to compare these results due to the absence of a control group.
Table V Psychosocial impact of genital warts in patients
|
Total n=40 |
Males n=20 |
Females* n=20 |
||||
|
Total points HIP‡ |
||||||
|
Average (SD) |
39.9 (14.1) |
41.1 (11.9) |
38.5 (16.7) |
|||
|
Min, max |
12.9, 67.9 |
21.1, 61.9 |
12.9, 67.9 |
|||
|
Total points CECA§ |
||||||
|
Average (SD) |
51.9 (18.9) |
55.0 (19.2) |
47.2 (18.1) |
|||
|
Min, max |
22, 96 |
22, 96 |
26, 90 |
|||
|
Points CECA - Emotional |
||||||
|
Average (SD) |
47.6 (16.0) |
49.8 (16.6) |
44.1 (15.1) |
|||
|
Min, max |
20, 83.3 |
20, 83.3 |
20, 70 |
|||
|
Points CECA - Sexual |
||||||
|
Average (SD) |
47.6 (25.5) |
51.2 (25.4) |
42.2 (25.8) |
|||
|
Min, max |
10, 100 |
20, 100 |
20, 100 |
|||
* The HIP values were not calculated for four females because they did not respond to this section of the survey. The CECA values were not calculated for seven females because they did not respond to this section of the survey
‡ Total HIP (HPV Impact Profile) scores ranged from 0 (no impact) to 100 (worst impact)
§ Greater CECA (Cuestionario Específico para Condiloma Acuminado) values indicate better conditions
SD: Standard deviation
Discussion
Our study provides a comprehensive review of the burden of GW in Mexico, and our results suggest that there is a high incidence and elevated costs due to this disease. The health burden of GW has been assessed in many countries using different approaches. Since there is no national registry in Mexico, there is a lack of reliable information that could be used to estimate the true burden of GW in Mexico. We estimated an annual incidence rate of 547 200 cases of GW among individuals 50 years or older in Mexico. The methodology we used to estimate the national incidence and prevalence of GW has been used in other countries, and several studies show that incidence and prevalence vary by region.23,27,28 For example, an incidence rate of 8.7 per 1 000 person-years was found in the placebo arm of an HPV vaccine clinical trial in a population of 15-26 year olds in Latin America.18 To have a reference of the number of new cases of GW in Mexico, we estimated the incidence rate to be 432 059 cases of GW among individuals 50 years of age or older, using reproductive health information from the Mexican Health and Nutrition Survey, 2012.29 Our data indicate an incidence rate of 4.3 per 1 000 person-years, compared to an Australian study using national hospital morbidity data that found an incidence rate of 2.19 per 1 000 person-years.21
The incidence of GW observed in our study is higher than most other published studies, and is similar to the results of research with younger participants (15-30 years).9,18,19,21,30 However, the average age of our patient sample was 32.8 years and we did not include younger participants who could have contributed to an overestimate of the prevalence. Interestingly, our patient sample reported consulting with internists for their most recent GW episode. This suggests that a non-negligible number of internists also regularly treat GW, in addition to specialists. Future research should explore GW referral, treatment, and management practices from a primary care perspective.
Another finding of our study is that the median number of visits for GW treatment was between three and four, and the most common treatments reported by specialists are ablative treatments and electrosurgery. Compared to other studies, the specialists we surveyed reported fewer visits per GW episode, which could be related to the type of treatment used, since most other studies indicate use of self-applied therapies.21,22,23 The high number of visits and ablative treatment could be due to delayed diagnoses in more advanced stages of the disease, which may require more visits per treatment. In addition, our study reports information regarding both public and private practice, with the latter reporting a higher number of visits. Although GW are not life-threatening, several studies have found that they are associated with anxiety, fear of rejection, discomfort, pain, emotional stress, and treatment is usually lengthy and painful.14,15 GW may also be associated with greater vulnerability of infection with HIV.31 In a UK study, patients reported similar CECA scores to our sample, mean CECA emotional (40) and sexual (46) scores.7 Also, a recently published report of a Cochrane systematic review revealed that patients with GW had a lower QoL compared to other non-malignant HPV-related diseases. Our study suggests that there is a deterioration of the QoL in patients with GW, but further research should be carried out to explore the global impact with specific instruments and use of a control group to compare the results.
This is the first study to report the incidence, treatment, management, and referral patterns of GW in Mexico. This study shows the significant impact GW have on public health due to their high incidence, elevated costs, and negative effect on patient QoL. There are several limitations in this study. One limitation is that incidence was estimated using information obtained from specialists who regularly treat GW. Furthermore, findings from the referral section of our questionnaire for both specialists and patients indicate a high level of involvement from the primary care providers, who were not surveyed as part of our study. These discrepancies may limit the accuracy of our estimate of the annual incidence of GW. Another limitation is the generalizability of our results, since the population included in the study may not represent the country’s population at large and the Central region was overrepresented. There may be a considerable number of persons living with GW who never receive a diagnosis because they do not regularly consult a specialist or because they may never be referred to a specialist. Despite these limitations, this study is a first attempt to estimate the burden of GW in Mexico. Our data shows that GW are a common disease, which exerts a considerable impact on health services and in the QoL of patients.











 nova página do texto(beta)
nova página do texto(beta)


