Introduction
HPV screening and vaccination are complementary preventive options often implemented as separate and non-coordinated public health programs. The HPV-FASTER protocols aim to address this disconnect by combining both strategies with the ultimate purpose of accelerating the reduction of cervical cancer incidence and mortality and making the programs both cost-effective and sustainable.
Results from two phase III trials comparing HPV vaccination against placebo among adult women (aged up to 45 years and 55 years for 4vHPV and 2vHPV vaccines, respectively)1,2 showing high protection against HPV type specific infections and persistent infections and the excellent and consistent results of the HPV-screening trials3,4.5 provide the basis for the HPV-FASTER proposal. The recognition of indications to vaccinate adult women in Europe6,7,8 and the US9 which do not include an upper age limit, favor the exploration of combined protocols of screening and vaccination and broadening the vaccine indications in developed and developing countries.
HPV vaccination trials in adult women
Evidence from epidemiological studies confirms that the risk of HPV infections persist as long as the individual is sexually active, albeit the risk of novel infections reduces with age in parallel with the reduction of new sexual partners.10 More recent cohort studies suggest that the risk of progression after HPV infection is constant irrespective of the age at infection.11 HPV vaccination trials in adult women confirmed the efficacy and safety of the vaccination. In such trials, the study groups include a fair proportion of HPV positive individuals and the observed protection is limited to the HPV types not prevalent at the time of vaccination. Therefore, HPV positive individuals will require a closer follow up and eventual treatment of any precancerous lesions. However, these women acquire long term protection against future HPV infections with the types included in the vaccine.
In the adult women’s trials, two broad groups of women can be identified. The first group comprised women who entered the ‘per-protocol’ or ‘according-to-protocol’ analyses of vaccine efficacy. These are typically defined as those who at study entry were: i) HPV16/18-DNA negative in cervical samples and serologically negative for HPV16/18 antibodies (an indirect marker of past infections); ii) had normal or only low-grade cervical cytology abnormalities at baseline and at month 7 after the completion of the vaccination protocol, and iii) received the three required vaccine doses at the specified timing of day one, one or two months, and six months without protocol violations. The second group included all women in the ‘intention-to-treat’ or ‘total-vaccinated-cohort’ protocols who received at least one dose of the HPV vaccine, irrespective of HPV status in serum or by cytology at study entry or at the completion of the vaccination scheme. Trials of both the 4vHPV and 2vHPV vaccines confirmed that protection against infections-and their related outcomes (cervical pre-cancer or cancer)-caused by vaccine-related HPV types was very high, provided that the women were HPV-DNA negative for the vaccine type at the time of vaccination; estimates of vaccine efficacy in the per-protocol groups were in the range of 85 to 90%, depending on the trial end points.1,2 Reduced, but nonetheless important, vaccine efficacies of approximately 50% were calculated for the intention-to-treat cohorts.1,2 HPV-DNA-positive women did not show any evidence of protection against diseases related to HPV types that they tested positive for at the time of vaccination.12 Thus, vaccination can offer protection to women without a current infection or disease, irrespective of previous viral exposure, and among those currently infected, can protect against further infections as well as re-infection with the same HPV type. Importantly, no safety concerns were reported for women that were HPV positive and received three doses of HPV vaccine13 or in women inadvertently vaccinated in the first months of pregnancy.14 Similar trials are in advanced stage or completion using the nine valent vaccine.
The HPV FASTER concept
In accordance with these findings, the proposal of the HPV-FASTER protocol is to offer HPV vaccination to women in a broad age range of 9 to 45 years irrespective of HPV-infection status. Women of any age above 25/30 years would, in addition to the vaccination, be screened using a validated HPV test as part of their initial visit; women who test HPV-positive would be offered triage and follow-up diagnostic tests and treatment in accordance with recommended guidelines.
Figure 1 provides a schematic representation of the HPV-FASTER concept. With adequate follow up of women who test positive for HPV at the time of vaccination, the lifetime cervical cancer risk of individuals identified as HPV -negative and HPV vaccinated with a broad spectrum vaccine should be very low, tending to zero. Further screening requirements of these women would consequently be reduced to one or two lifetime screening events.
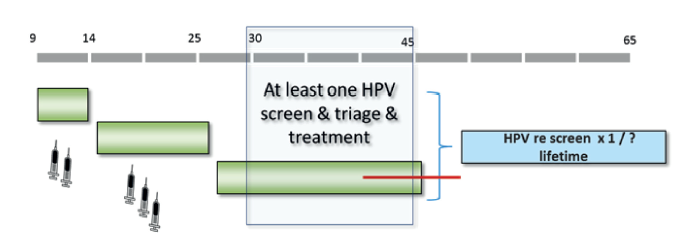
Figure 1. The HPV-FASTER strategy proposes to 1) continue the generalized vaccination campaign of the 9 to 14 years old; 2) Expand the catch-up vaccination to at least age 25 to 30 and 3) offer HPV vaccination to women aged 30 to 45 years (exact cutoff ages to be determined). In addition, any women at the ages 25 to 30 and above will be offered HPV screening test with concurrent follow up (triage and diagnostics) of the HPV positive women and if required, treatment of the pre-neoplastic lesions
Because the sensitivity of HPV tests for cervical intraepithelial neoplasia of grade 2 or higher (CIN2+) is not 100%, around 5 to 10% of the HPV-DNA-positive women will be misclassified as HPV negative and will not benefit from early diagnosis and treatment, and perhaps a second screening event may be necessary in the populations that can cope with the logistics of organizing it successfully.
A major benefit from the HPV FASTER protocols is that the predicted subsequent needs for screening may be dramatically reduced to one/two lifetime visits, thus increasing sustainability and compliance as well as alleviation of the burden and workload at the health centers, typically overloaded already with patient care.
If vaccination programs include also boys and young males -say to age 26-, the global impact is likely to be accelerated by enhancing herd protection and increasing the resilience of the vaccination program to temporary vaccination failures. HPV vaccines have shown a strong herd protection effect,15 which at least in part, could be attributed to a reduction of the transmission rates of HPV- positive women receiving vaccination. Cost effectiveness of these vaccination protocols need to be calibrate to the country and be attentive of the vaccine costs. Adding boys and young males into the generalized vaccination scheme has thus the potential to accelerate disease control/elimination while protecting males from HPV induced gender specific malignancies even if they leave the female vaccinated herd protection.
The first controlled trial under way is now ongoing in Mexico, where women undergoing HPV screening are offered HPV vaccination in a comparative trial mode. The study is intended to prove the safety of expanding the screening intervals to 10 + years endpoint. Intermediate endpoints will document the added value of including vaccination in the screening protocol by assessing the impact on HPV infection, persistent infection and CIN lesions.16
The best data available from population studies in adult women that would resemble the HPV-FASTER proposal are the results of the vaccination program in Australia that included women up to 26 years of age with an average vaccination coverage close to 65%, followed by a switching of the screening program to an HPV based primary screening alternative. Long term follow up of these gigantic national cohorts is expected to show that the incidence of CIN2+ and of cervical cancer in these populations is extremely low and therefore that requirements for further screening may be reduced to perhaps a second additional HPV screening round within a decade and at around menopause to handle the few HPV positive women that may have escaped detection at the time of their first screen (<5%) and the cases to be due to HPV types not included in the broad spectrum vaccine.
One of the controversial issues for the HPV-FASTER strategy is whether to vaccinate women irrespective of HPV status or to restrict vaccination to only those who are HPV-DNA/ mRNA negative. This is because current HPV vaccines lack therapeutic effect against the development of cervical lesions in woman who are already HPV-positive at the time of vaccination.12 In favor of the nonselective approach, the evidence indicates that: 1) vaccination of HPV-positive women or those with CIN2+ is safe; 2) vaccination does not interfere with the treatment or follow-up of CIN2+ cases; 3) it would be simpler logistically, and would facilitate compliance with three-dose vaccination regimes if the initial vaccine dose is delivered in combination with an HPV test in women aged ≥30 years; and 4) vaccination would offer protection against infection and future disease caused by the other HPV types included in the vaccine that are not associated with the prevalent infection/lesion. Further interest in vaccinating HPV-positive adult women (including women with a history of CIN2/3) comes from evidence that these women are at high lifetime risk of subsequent additional HPV related cancers of the ano-genital tract and the oropharynx.17,18
The potential impact of a one-dose vaccination protocols
Finally, an interesting concept still poorly explored, hypothesized that vaccination of middle aged and young adult women offers the potential to boost the global impact of the vaccination program by reinforcing the herd protection effect.19 Under this hypothesis, the presence of HPV antibodies in the cervical-vaginal fluid may result in the shedding of virions already coated with antibodies, thus with a potentially reduced capacity to infect novel sexual partners. Typically HPV positive women with normal cytology identified at screening are invited to more frequent follow up visits and 6 to 12 month observation period are common in screening protocols and guidelines.20 However, in the absence of any effective treatment, these observational time intervals create an opportunity in which transmission is likely to occur thus contributing to increase the global risk of infection of the population. This novel frame of understanding requires close verification and some studies are ongoing to this respect before a formal recommendation to vaccinate HPV positive women (with or without cervical lesions) can be incorporated as part of the routine screening programs.
Much interest is now devoted to exploring if one dose of HPV vaccine would ensure long term protection against HPV infection and subsequent cancer. Such opportunity has been suggested by indirect evidence from clinical trials in which partially vaccinated girls and young women were followed up for antibody concentrations in serum and subsequent cervical lesions. In such observations, women receiving one dose showed significant protection after seven years of follow up.21,22 Should this information be confirmed in the ongoing formal trials, reduction of the vaccination indication to one dose would greatly facilitate the logistics and increase the vaccination coverage. Likewise, further work will be worth doing to verify if the one dose regime would also be applicable to women above 25 and to adult women in screening ages thus approaching the objective of intervention campaigns in which one visit could be recommended including HPV screen/treat and vaccination.23
Conclusion
In most developing countries, changing the paradigm of cervical cancer prevention from a strategy of repeated screening visits and triage/treatment of the pre-neoplastic lesions to a campaign-type strategy tending to a one lifetime visit that includes screen/treat and vaccinate is an important alternative.
In developed countries, where screening is largely integrated into the health services, the option to receive vaccination against a significant reduction of the screening requirements is likely to be discussed as a right to know of the opportunities for prevention available to women. Under this frame, the health system is required to provide unbiased information to women for an informed option of receiving or not the HPV vaccine. The public health systems in developed countries need to understand that the integration of screening protocols with the vaccination campaigns is necessary and highly desirable. In practical term, this is already occurring when vaccinated cohorts are massively entering the screening ages.











 text new page (beta)
text new page (beta)


